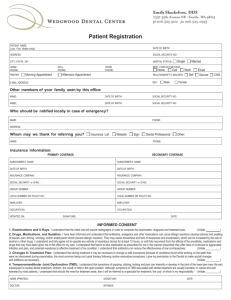
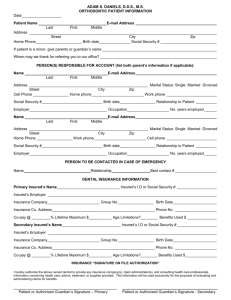
Kenneth S. Carlough D.M.D., M.D.S. Jeffrey E. Burzin D.D.S. Laura J
advertisement
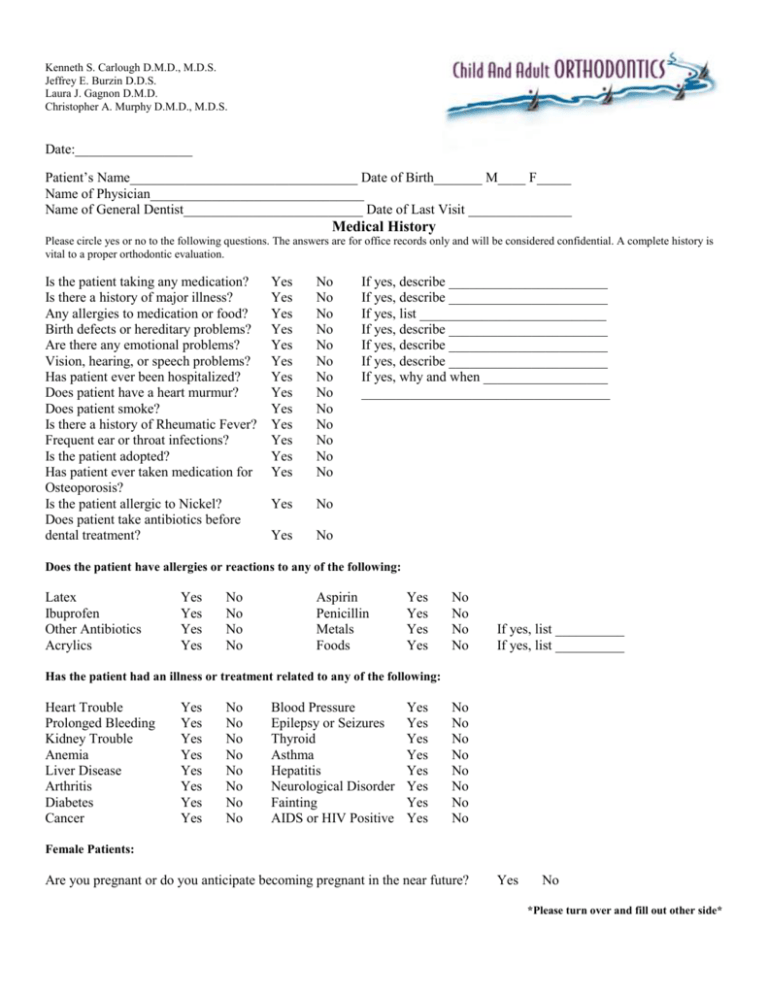
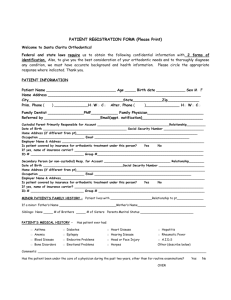
Kenneth S. Carlough D.M.D., M.D.S. Jeffrey E. Burzin D.D.S. Laura J. Gagnon D.M.D. Christopher A. Murphy D.M.D., M.D.S. Date:_________________ Patient’s Name_________________________________ Date of Birth_______ M____ F_____ Name of Physician_______________________________ Name of General Dentist__________________________ Date of Last Visit _______________ Medical History Please circle yes or no to the following questions. The answers are for office records only and will be considered confidential. A complete history is vital to a proper orthodontic evaluation. Is the patient taking any medication? Is there a history of major illness? Any allergies to medication or food? Birth defects or hereditary problems? Are there any emotional problems? Vision, hearing, or speech problems? Has patient ever been hospitalized? Does patient have a heart murmur? Does patient smoke? Is there a history of Rheumatic Fever? Frequent ear or throat infections? Is the patient adopted? Has patient ever taken medication for Osteoporosis? Is the patient allergic to Nickel? Does patient take antibiotics before dental treatment? Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes No No No No No No No No No No No No No Yes No Yes No If yes, describe _______________________ If yes, describe _______________________ If yes, list ___________________________ If yes, describe _______________________ If yes, describe _______________________ If yes, describe _______________________ If yes, why and when __________________ ____________________________________ Does the patient have allergies or reactions to any of the following: Latex Ibuprofen Other Antibiotics Acrylics Yes Yes Yes Yes No No No No Aspirin Penicillin Metals Foods Yes Yes Yes Yes No No No No If yes, list __________ If yes, list __________ Has the patient had an illness or treatment related to any of the following: Heart Trouble Prolonged Bleeding Kidney Trouble Anemia Liver Disease Arthritis Diabetes Cancer Yes Yes Yes Yes Yes Yes Yes Yes No No No No No No No No Blood Pressure Epilepsy or Seizures Thyroid Asthma Hepatitis Neurological Disorder Fainting AIDS or HIV Positive Yes Yes Yes Yes Yes Yes Yes Yes No No No No No No No No Female Patients: Are you pregnant or do you anticipate becoming pregnant in the near future? Yes No *Please turn over and fill out other side* Dental History Has the patient ever sucked their thumb or fingers? If yes, until what age?____________________ Yes No Have there been any severe injuries to the face or jaws? If yes, describe__________________________ _____________________________________________ Yes No Does the patient have jaw or TMJ problems? If yes, describe _________________________ ____________________________________________ Yes No Unusual dental problems? Yes No If yes, describe _________________________ Does the patient grind their teeth at night or during the day? Yes No Has the patient ever been told that they have periodontal or gum disease? Yes No History of speech problems? Yes No Does patient frequently breathe through their mouth? Yes No Has patient had any previous orthodontic treatment? Yes No What is the reason for this visit? _______________________________________________ NOTES: _________________________________________________________________ _________________________________________________________________________ _________________________________________________________________________ I authorize Child and Adult Orthodontics to take the necessary X-rays before, during and after my child’s orthodontic treatment. Initials________ Signature of Patient, Parent or Guardian______________________________ Date ___________ Updated History Date Initials __________ _________ __________ _________ __________ _________ __________ _________ __________ _________ __________ _________