NICU Rotation Summar.. - Pediatrics House Staff
advertisement

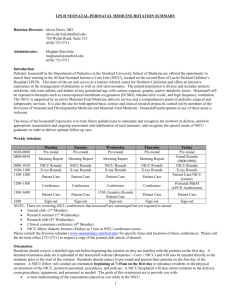
NICU – 5 Min Curriculum Rotation Director: Alexis Davis, MD, alexis.davis@stanford.edu, (650) 723-5711 Administrator: Meghan Stawitcke, meghans4@stanford.edu (650) 723-5711 Key Rotation Issues: Orientation: o Residents will pre-round on their patients on the first day o Fellow conducts orientation in NICU beginning at 7:15am- PLEASE REVIEW THE ORIENTATION SLIDE SET POSTED ON THE HOUSESTAFF WEBSITE AND EMAILED TO YOU PRIOR TO THE START OF THE ROTATION. The Hospitalist will re-orient you to the delivery room later in the day/week. Goals are to give clear expectations, tools to fulfill expectations, and an appreciation for how you may enhance your education while in NICU o Direct patient care/delivery responsibilities begin immediately thereafter. Team: o ALL NICU staff from clerks to social workers have an integral role on the NICU team! o A junior resident and three NNPs comprise each team. One NNP will serve as a mentor for patient care questions and to cover your patients when you are post-call or in clinic. o PATIENT DISTRIBUTION: on-service/on-call fellow determines based on volume and what’s anticipated. Pick-up patients you admit if possible. ADVOCATE FOR YOUR INTERESTS. Weekdays: rounds conducted as two teams beginning at 9:00am o Arrive early enough to pick up new patients (typically 7:00am) o 10:30 X-ray rounds – 2nd floor reading room, reviews studies prior 24 hrs. Attend and give succinct “one-liner” about your patient & indication for study. o Wednesday 1330 – Genetics and dysmorphology bedside teaching rounds o Fridays 1100 – Fellows lectures, NICU conference room o Fridays 1200 – Perinatal Morbidity and Mortality conference, LPCH Boardroom. Housestaff are expected to present cases if their patient is chosen for discussion. o Sign-out: 4pm NICU conference room M-F, purpose to communicate anticipated o/n issues. Do not sign-out routine diagnostics/therapeutics. Team walks through unit following sign-out to review issues with bedside RNs. Weekends: rounds conducted as two teams beginning at 9:30 o Pre-rounding duties will be allocated by the on-call NICU fellow, and housestaff should expect to round on their own patients as well as others. o Write orders during rounds as time permits o Divide rest of work among on-call team following rounds o Sign-out to incoming night coverage: 4pm in NNP office Feedback: Written evals via Medhub from attendings, NNPs, fellows, peers on service. Residents expected to solicit verbal feedback from attendings each week. Verbal feedback on delivery room skills will be provided by the PICN Attending Group. Prior to 1st Shift: Familiarize yourself with the NICU Guide on-line Review NRP manual and algorithms prior to CAPE session/starting rotation Unique Expectations: Carry NICU phone Delivery Room Attendance – TOP PRIORITY. ATTEND ALL DELIVERIES (DAY/NIGHT) REQUIRING PEDIATRIC TEAM with exception of pre-rounding, AM rounds, sign-out rounds, morning report & noon conference. o You will supervise interns at all deliveries along with a hospitalist, NNP, or fellow o Complete Delivery Room Attendance log card after each delivery; review with hospitalists mid-way in rotation. Turn in to Jadene Wong at rotation completion. Resident Roles and Responsibilities o Pre-round and provide daily documentation for your patients o Updates the sign-out sheet daily NICU – 5 Min Curriculum o o Supervise 3rd year medical students caring for your patients; review and co-signs notes Attend weekly Perinatal Morbidity & Mortality Conference; present patient histories when applicable Weekly Schedule 0630-0800 0800-0830 0900-1030 1030-1100 1100-1200 1200-1300 1300-1600 Monday Pre-round Tuesday Pre-round Wednesday Pre-round Thursday Pre-round Morning Report Morning Report Morning Report Morning Report NICU Rounds X-ray Rounds NICU Rounds X-ray Rounds NICU Rounds X-ray Rounds NICU Rounds X-ray Rounds Patient Care Patient Care Patient Care Patient Care Conference Conference Conference Conference Friday Pre-round Grand Rounds (0800-0900) NICU Rounds X-ray Rounds Patient Care/Fellow lectures Perinatal M&M (LPCH Auditorium) 1330: Genetics Rounds Patient Care Patient Care Patient Care 1600 Sign-out Sign-out Sign-out Sign-out Sign-out NOTE: There are recurring NICU conferences that housestaff are encouraged but not required to attend: Journal club (3rd Monday) Research seminar (1st Wednesday) Research club (4th Wednesday) Clinical consensus conference (4th Monday) NICU fellows’ didactic lectures (Fridays in the NICU conference room) Please consult the division calendar (www.neonatology.stanford.edu) for specific times and locations of these conferences. Please call the division office (723-5711) to request a copy of the journal club article, if desired. Patient Care Patient Care Night Call NNP, resident, Fellow and hospitalist on-call together. Resident is 1st call for all patients until 6:00am. Attend all deliveries if not involved in acute situation or mid-procedure in unit. Any issues not able to be addressed by housestaff are to be referred to the NNP, Gap provider, or fellow for consultation. DO NOT HESITATE TO ASK FOR HELP. Nurses may also consult one of these providers if they are concerned that the answer they get from you is suboptimal- this is standard procedure in the NICU. Midnight rounds- focus on the reviewing new lab results or other physiologic parameters (as instructed during sign-out rounds) and to ensure that the appropriate tests are ordered for the morning. Any significant change in patient status or procedures performed should be documented in the patient chart and signed out to the daytime team. Documentation and Communication H&Ps: Required on all patients with special circumstances as follows: - Post-op patients admitted for observation only – if surgical H&P already completed, written post-op accept note with physical is sufficient. - PICN transfers with prior H&P only require accept note. (NOTE: Infants transferred from the Well Baby Nursery require an H&P) Transfers and Discharges: All patients leaving the NICU require a written report that summarizes the events of their NICU hospitalization. This is usually best accomplished through a systems-based or problem-based approach, however, less complicated patients may only merit a brief summary. Include newborn screening, immunizations, hearing screening, or any other health surveillance issues. - Send discharge summary with any transfers to other facilities and/or primary care physicians - Maintain sign-out and Interim Summary documents in Cerner, especially for any potential weekend discharges or unexpected overnight transfers. Updates to Interim Summaries should be done weekly and noted in the ad hoc charting. Communication: Housestaff will be expected to provide updates for the parents of their patients. They should also ensure that a member of the NICU team makes direct communication with the receiving physician/private pediatrician at the time of transfer or discharge. Discuss with your attending to determine which member of the team would be most appropriate to initiate this conversation.