The Colon: An Overlooked Site for Therapeutics in Dialysis Patients
advertisement

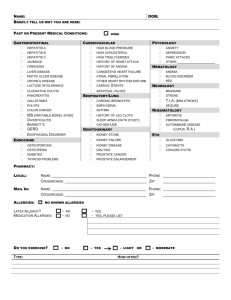
The Colon: An Overlooked Site for Therapeutics in Dialysis Patients Ruben Poesen 1, Björn Meijers 1, Pieter Evenepoel 1 1 Department of Microbiology and Immunology, Division of Nephrology, University Hospitals Leuven, B-3000 Leuven, Belgium Word count abstract: 164 Word count main body: 4204 Figures: 1 Tables: 1 Key words: colon, chronic kidney disease, dialysis Address for correspondence: P. Evenepoel, MD, PhD Dienst nefrologie Universitair Ziekenhuis Gasthuisberg Herestraat 49 B-3000 Leuven BELGIUM Tel. +32-16-344591 Fax. +32-16-344599 e-mail: Pieter.Evenepoel@uz.kuleuven.ac.be Acknowledgments: RP is recipient of a Ph.D. fellowship of the Research Foundation - Flanders (FWO) (grant 11E9813N) 1 ABSTRACT Morbidity and mortality related to chronic kidney disease remains unacceptable high, despite tremendous progress in its prevention and treatment. In an ongoing quest to improve outcome in chronic kidney disease patients, the colon might be an appealing but largely underexplored therapeutic target. A clear bi-directional functional relationship exists between the colon and kidney, also referred as to the colo-renal axis. Uremia has an important impact on the colonic microbiome. The microbiome, in turn, is an important source of uremic toxins, with p-cresyl sulfate and indoxyl sulfate as important prototypes. These co-metabolites accumulate in the face of a falling kidney function, and may accelerate the progression of renal and cardiovascular disease. Several therapeutic interventions, including prebiotics and adsorbants, specifically target these colon-derived uremic toxins originating from bacterial metabolism. As kidney function declines, the colon also gains importance in the homeostasis and disposal of potassium and oxalate. Their colonic secretion may be increased by drugs increasing the expression of cAMP and by probiotics (e.g., Oxalobacter formigenes). 2 INTRODUCTION Chronic kidney disease (CKD) has become a global health issue and reaches epidemic proportions (1,2). Mounting data point to the lethal synergy between CKD and cardiovascular disease (3-5) with a cardiovascular mortality in CKD patients treated with hemodialysis that is more than fivefold higher than in the general population (5,6). Improving this poor prognosis is an ongoing challenge for the nephrology community. Conventional dialysis techniques, however, seem to have reached their limits. Indeed, recent large randomized controlled trials (HEMO, ADEMEX) failed to show an improvement of patient outcome by increasing the removal of low-molecular-mass water-soluble solutes and even middle molecules above standard of care (7,8). Renal transplantation, undoubtedly the best treatment option in patients with end-stage renal disease (9), is hampered by organ shortage, and morbidity related to the surgical procedure and life-long immunosuppression. Therefore, a need for alternative or adjuvant therapeutic strategies persists. It is well established that the large intestine plays a non-negligible role in the homeostasis of several electrolytes and minerals, and disposal of nitrogenous waste products. Finally, the large intestine is an important source of uremic toxins (10). Therefore, targeting the large intestine might be a promising adjuvant approach to tackle the high morbidity and mortality burden in CKD. Gastrointestinal interventions in medicine are not new, but date back to ancient times. For example, in 40 B.C., Dioscorides, a Greek physician, pharmacologist and botanist advocated terra sigillata for treating multiple disorders, including diseases of the kidney. More recently, induced diarrhea and intestinal perfusion have been used with variable success and tolerance to treat uremia (11). With the advent of dialysis (Dr. W. Kolff, first successful dialysis in 1945 (12)) and renal transplantation (Dr. J. Murray, first successful transplantation in 1954 (13)) and potent drug therapy (e.g., angiotensin converting enzyme inhibitors, 1975 (14)), interest in gastrointestinal interventions in CKD patients has waned. An increased awareness of the limitations of current treatment options has renewed interest in alternative therapeutics in recent years. This review aims to summarize important functions of the colon, both in health and CKD, and to discuss the colon as a therapeutic target in CKD. 3 THE COLON IN HEALTH The human large intestine is approximately 150 cm long with an internal surface area of 1.3 m², and weighs approximately 220 g, of which 80 % is moisture. The colonic transit time ranges from 20 to 140 hours (mean 60 hours) (15). It has long been thought that the principal role of the colon was to confer a mechanism for the orderly disposal of waste products of digestion, and to absorb salt and water. Approximately 1.5 liters of electrolyte-rich fluid per day, accounting for 90 % of the salt and water entering the proximal colon, is absorbed by the colonic epithelium. The key determinant of colonic water absorption is the rate of sodium absorption, which can be electrogenic via the epithelial sodium channel or electroneutral via parallel sodium/hydrogen and chloride/bicarbonateexchange. The colon also contributes to acid-base homeostasis by secreting bicarbonate via the chloride/bicarbonate-exchanger, which helps in buffering organic acids produced by colonic bacteria. These organic acids mainly originate from carbohydrate fermentation (vide infra), which is most prominent in the proximal colon, thereby explaining the acidic intraluminal mean pH of 5.6 in this part of the colon. The pH then gradually increases along the length of the colon, reaching a mean pH of 6.6 at the distal part of the colon. Finally, a significant net potassium secretion occurs in the colon via several apical potassium channels with a total fecal potassium excretion averaging 10-15 mmol/d (15,16). The large intestine provides an important reservoir for a microbial community, which is complex and diverse, biochemically very active, and interacts with its host (17,18). The colonic microbiome has a clear role in the development and modulation of the human gut immune system (19). In addition, a number of vitamins are partly derived from the colonic microbial flora: vitamin K, nicotinic acid, folate, pyridoxine, vitamin B12 and thiamine (15). Furthermore, it has become clear that the colon is responsible for salvaging energy and nitrogen from carbohydrate and protein not digested in the upper gastrointestinal tract, a process known as fermentation. Colonic bacterial species can roughly be categorized as saccharolytic (i.e., those that predominantly ferment carbohydrates) or proteolytic 4 (i.e., those that are predominantly protein fermenters). In general, carbohydrate fermentation is considered beneficial to the host, mainly by production of short-chain fatty acids (20,21). Butyrate, for example, is a major energy source for the colonic epithelium (22). Protein fermentation (putrefaction), on the other hand, leads to a variety of end-products including short- or branchedchain fatty acids, and other co-metabolites, some of which are potentially toxic such as ammonia, amines, thiols, phenols, and indoles (23,24). It is generally accepted that the most important regulator of bacterial metabolism, besides colonic transit time, is nutrient availability and especially the ratio of available carbohydrate to nitrogen (25,26). In case of carbohydrate excess, the fermentation process shifts towards lower production of amino acid metabolites through three different mechanisms. Firstly, as carbohydrate fermentation results in a decrease of the intraluminal pH through production of short-chain fatty acids, large intestinal protease activity will decrease resulting in a lower availability of amino acids (27). Secondly, bacterial amino acid metabolism is decreased through the so-called “catabolite repression” (27,28). This implies that, in the presence of fermentable carbohydrates, the expression of genes involved in bacterial metabolism of amino acids is suppressed. Finally, fermentation of carbohydrates provides energy to the microflora, thereby increasing incorporation of α-amino nitrogen, provided to the large intestine by protein escaping digestion in the upper gut and from blood urea that has diffused into intestinal contents (i.e., urea recycling into the bacteria), into the expanding bacterial biomass (29,30). Conversely, in case of carbohydrate deprivation, nitrogen will be predominantly fermented, thereby increasing the production of potentially toxic co-metabolites (25). These waste products are largely absorbed, metabolized and subsequently excreted by the kidneys, at least partly through renal tubular secretion (31). THE COLON IN CHRONIC KIDNEY DISEASE The kidneys play an important role in preserving the “milieu intérieur”. As the number of nephrons declines, compensatory hormonal and non-hormonal mechanisms are activated to maintain 5 homeostasis of electrolytes and minerals, and to limit the accumulation of waste products. These mechanisms not only involve the kidneys but also the colon. It is noticed that many patients with progressive CKD remain normokalemic despite a deteriorating excretory renal function (32). This observation is only partly explained by an adaptive increase in renal tubular potassium excretion, because urinary potassium losses still are substantially lower than in healthy individuals, even after adjustment for potassium intake (32,33). It has long been known that fecal potassium losses in patients with CKD are elevated, suggesting either decreased intestinal absorption or increased secretion (33,34). Subsequent animal studies pointed to increased colonic potassium secretion in CKD (35,36). The mechanisms involved include an increased sodium/potassium ATPase-mediated potassium uptake at the basolateral membrane, a secondary rise in intracellular potassium concentration, and an increase in apical membrane permeability for potassium (32,37,38), likely reflecting an increased expression of cAMP-regulated apical BK channels (32,39). Literature data suggest that aldosterone at least partly mediate the increased colonic potassium secretion (40-42). Whether the colon also plays a role in the maintenance of phosphate homeostasis is unknown. It is well established that in normal circumstances most of dietary phosphate is absorbed in the small intestine (43). Nonetheless, the observation that phosphate enemas induce severe hyperphosphatemia unequivocally demonstrates the colonic capacity to absorb phosphate (44,45). Available evidence indicates that phosphate transport across the colonic epithelium is passive and paracellular (45), and therefore electrochemical gradient-driven. Data on free phosphate concentrations in colonic contents are non-existing. Therefore, it is not known whether under physiological conditions the electrochemical gradient favors absorption or secretion. From a theoretical point of view, CKD-related hyperphosphatemia may be hypothesized to push the balance toward secretion. Furthermore, there also are colon-related adaptive mechanisms in oxalate homeostasis in CKD. As oxalate is accumulating in the face of a declining renal function, reversal of the normal colonic 6 absorptive state to a net secretory state has been observed (46). The exact mechanism behind this phenomenon is largely unknown, although cAMP might herein also be a relevant mediator (47). Like other disease states, including obesity (48) and inflammatory bowel disease (49), CKD goes along with a distinct gut microbiome (50). Decreases of both the Lactobacillaceae and Prevotellaceae families are most remarkably. Dietary restrictions and drug therapy (e.g., phosphate binders, frequent antibiotic use) may at least partly account for this change in gut microbiome. Hemodialysis patients, as compared with control subjects, consume significantly less dietary fiber, an important source of fermentable carbohydrates in the colon (51). This low dietary fiber intake most probably reflects restricted ingestion of fruits and vegetables. It should however be of note that changes in the gut microbiome were also observed in a uremic rat model without dietary restrictions, suggesting that uremia per se also has an impact (50). Clinical evidence furthermore suggests that protein assimilation in the small intestine is impaired (52). As a consequence, an increased amount of dietary protein will become available in the colon. The decreased ratio of available carbohydrate to protein (α-amino nitrogen) in the large intestine may favor a shift from a saccharolytic to a proteolytic fermentation pattern. This shift is accentuated by high ammonia concentrations resulting from bacteria-mediated hydrolysis of urea. High levels of ammonia are responsible for elevated pH and foster overgrowth of proteolytic species. In addition, colonic transit time is significantly prolonged in CKD (53,54). As a consequence, a larger part of the colon becomes carbohydrate deprived which in turn will induce an upstream expansion of proteolytic species (24). Besides a different gut microbiome, uremia might also impair the intestinal barrier function with an increase in intestinal permeability (55-58). Putative mechanisms include disruption of the colonic epithelial tight-junction apparatus (59) and presence of subclinical chronic inflammation along the intestinal tract (60). Other contributing factors are intestinal mucosal ischemia due to splanchnic hypoperfusion (especially during hemodialysis treatment) and venous congestion due to heart failure 7 (61,62). Dysfunction of the intestinal barrier in CKD is associated with bacterial translocation and endotoxemia, which is related to systemic inflammation, malnutrition, cardiovascular disease, and possibly reduced survival (56,58,59,63,64). The large intestine is increasingly recognized to be a relevant source of uremic retention solutes in CKD (10) (Figure 1). Important prototypes of uremic retention solutes originating from colonic bacterial metabolism include p-cresyl sulfate and indoxyl sulfate (10). p-Cresyl sulfate is the endproduct of the combined actions of bacterial fermentation of tyrosine to p-cresol and endogenous sulfate conjugation. Likewise, indoxyl sulfate is the end-product of bacterial fermentation of the amino acid tryptophan to indole followed by endogenous oxidation and sulfate conjugation (65). Observational studies in patients at various stages of CKD linked both p-cresyl sulfate and indoxyl sulfate to overall mortality (66-68), cardiovascular disease (69,70) and CKD progression (71). Further mechanistic studies demonstrated uremic concentrations of p-cresyl sulfate and indoxyl sulfate to elicit oxidative stress (72,73), to induce endothelial dysfunction (74-76) and cardiac remodeling (77), and to accelerate CKD progression (78,79). Both p-cresyl sulfate and indoxyl sulfate are highly protein-bound, which explains their limited removal by conventional dialysis techniques (80). Besides renal retention, increased colonic generation most probably contributes to the high circulating levels of these co-metabolites (up to 10 fold increase) in CKD. Indeed, 24h urinary excretion rates of pcresol (as a surrogate for 24h colonic generation rates) were found to be significantly higher in subjects with glomerular filtration rate < 60 ml/min per 1.73m² than in those with glomerular filtration rate ≥ 60 ml/min per 1.73m² (52). This observation supports the thesis that CKD favors a proteolytic fermentation pattern, as outlined above. Finally, it should be of note that the survival time of anephric, germ-free rats is nearly twice that of conventionally raised rats (81) THE COLON AS THERAPEUTIC TARGET IN CHRONIC KIDNEY DISEASE 8 The role of the colon in the homeostasis of electrolytes and minerals, and in the clearance of waste products is limited in patients with normal renal function, but gains importance as renal function declines. In the following section, current evidence with regard to therapeutic interventions targeting the colon in CKD is summarized. Potassium Hyperkalemia remains a frequent and life-threatening complication in patients receiving hemodialysis. It is estimated that more than 10 % of dialysis patients are facing higher than normal potassium values, conferring an increased mortality risk (82). Since cAMP-regulated apical BK channels regulate colonic potassium secretion (32,39), drugs increasing colonic cAMP expression such as the laxative bisacodyl might prove useful when renal excretion becomes deficient. In a study by Mathialahan et al., bisacodyl (titrated according desirable stool frequency) was administered to 8 control subjects and 13 hemodialysis patients (83). After 2 weeks of treatment, bisacodyl significantly decreased the mean interdialytic serum potassium concentration (0.4 ± 0.1 mmol/l) in hemodialysis patients, but no effect was observed in control subjects. Treatment with lactulose, on the other hand, had no effect on the serum potassium concentration, making a solvent drag effect due to laxatives less plausible. Thus, bisacodyl might be a valuable adjuvant treatment option for hyperkalemia, but larger and longer-term studies are required to confirm these finding. Given the putative role of aldosterone as an activator of colonic potassium secretion (40,41), aldosterone agonists, e.g., fludrocortisone, may also be considered a valuable option(84-88). Nyman et al., treating symptomatic hypotension in 5 anuric dialysis patients with fludrocortisone for 3 to 9 months (85), noted a decrease in serum potassium from 4.7 to 4.0 mmol/l. This finding was also reported by Singhal et al. (86); they observed a similar decrease in patients treated with 0.1 - 0.3 mg/d fludrocortisone for 3 to 6 months. A note of caution is, however, warranted, as a recent study in oligo- to anuric hemodialysis patients demonstrated a survival benefit with mineralocorticoid 9 receptor antagonist spironolactone (89). The long-term effects of fludrocortisone on clinical outcomes have not been studied to date. Finally, polystyrene sulfonate potassium binding resins, already reported in 1961 (90), remains a valuable and efficient treatment option for hyperkalemia (91). Recent case reports of colon necrosis complicating the use of this resin warrant caution (92,93). Treatment, however, should be considered safe when precautions are taken into account. These include the avoidance of high-sorbitol mixtures (max. 33 % sorbitol), and exclusion of patients with functional and structural intestinal abnormalities (91). Phosphate Hyperphosphatemia is a common complication in patients with advanced CKD with up to 52 % of dialysis patients having serum phosphate levels > 5.5 mg/dl (94). As hyperphosphatemia is associated with cardiovascular disease (95) and mortality (96), therapeutic interventions seem mandatory. Dietary phosphate restriction is usually insufficient to maintain phosphate levels within the normal range and up to 90 % of dialysis patients need treatment with phosphate binders (97). Hereby, increasing amounts of phosphate are disposed in the colon as calcium phosphate, lanthanum phosphate or bound to resins. Remarkably little is known about the fate of this complexed phosphate in the colon. Equally little is known about the role of the microbiome in overall phosphate homeostasis. Theoretically, the microbiome may lower the phosphate exposure to the host either by lowering the colonic bioavailability (98) or by storing phosphate in the bacterial biomass as polyphosphate (99). Bacteria use inorganic phosphate as the preferred phosphate source. When inorganic phosphate is available in excess, it is taken up by the inorganic phosphate transport (Pit) system that is constitutively expressed in the bacterial cell membranes (100). It should be of note that colonic bacteria, as opposed to human metabolism, possess phytase and thus can release phosphate from phytate containing nutrients such as plants. Suppressing microbial phytase activity may be another theoretical tool to lower the phosphate exposure. Of interest, leavened bread (i.e., 10 must breads) have a higher phosphate bioavailability than unleavened products as yeast is also capable of hydrolyzing phytate (101). Oxalate Massive oxalate retention is rather uncommon in dialysis patients, except in primary hyperoxaluria (102). Dialysis patients with secondary hyperoxaluria exhibited approximately fivefold increases in oxalate levels (103), but clinically relevant secondary oxalosis is rarely seen with current dialysis techniques due to its relatively easy dialytic removal. Of note, calcium-oxalate nephrocalcinosis is a frequent finding in the early post-transplant period and is related to oxalate accumulation during dialysis. Preliminary evidence suggest that calcium-oxalate nephrocalcinosis may compromise graft survival (104,105). Thus, oxalate accumulation in dialysis patients, and especially those listed for transplantation, might be more relevant than currently acknowledged. In normal circumstances, intestinal (i.e., exogenous) oxalate uptake is not important (106). Nonetheless, certain disease states, e.g., inflammatory bowel disease and malabsorption following anti-obesity surgery, are associated with a significant increase in intestinal (i.e., colonic) oxalate absorption, also known as enteric or secondary hyperoxaluria (107-109). One way to reduce intestinal absorption is to decrease dietary intake, but formal advice about dietary restrictions is challenging (106). Besides dietary intake of oxalate itself, bioavailability also depends on co-ingested nutrients (106). For example, high dietary calcium intake is associated with a decreased oxalate uptake due to an intraluminal calcium-oxalate binding effect (110). Phosphate binders are related with a diminished urinary oxalate excretion, and, not surprisingly, this effect was most pronounced in the case of calcium-based phosphate binders (111,112). Oral ingestion of conjugated bile acids might be another oxalate lowering treatment, certainly when dealing with patients with steatorrhea due to bile acid malabsorption (113). Cholestyramine has also been used to bind oxalate in the gut and to reduce its uptake, but results are not consistent (114,115). 11 Similar to potassium, active colonic oxalate secretion is cAMP-mediated (39). Therefore, upregulating intestinal cAMP (e.g., bisacolyl) might theoretically also attenuate oxalate accumulation, but studies evaluating this effect are lacking. There is increasing evidence that colonic microbiota in general, and Oxalobacter formigenes more specifically, are important in oxalate homeostasis (116,117). Higher rates of colonization with Oxalobacter formigenes are associated with a reduced prevalence of oxalate stones in the general population (117). It is hypothesized that Oxalobacter formigenes not only degrades ingested oxalate, but also triggers colonic secretion (118), which is possibly mediated by an anion exchanger (putative anion transporter-1) (119). Oxalobacter formigenes therapy normalizes serum oxalate levels in an animal model of primary hyperoxaluria (120). Human studies, however, show mixed results, possibly due to small sample size. In a clinical intervention study, Oxalobacter formigenes-containing capsules induced a > 35 % decrease (range 38.5 – 92 %) in urinary oxalate excretion in 4 out of 6 patients after 1 month (121). A substantial serum oxalate lowering effect was also observed in 2 infants with primary hyperoxaluria (122). Although encouraging, these finding were not confirmed in a randomized controlled trial including 19 patients with primary hyperoxaluria (123). The exact role of Oxalobacter formigenes therefore remains uncertain. Larger studies, also including patients with enteric hyperoxaluria, are needed to establish the added value of Oxalobacter formigenes administration. Besides Oxalobacter formigenes, probiotics mainly containing lactobacilli have been evaluated in the treatment of hyperoxaluria (124-126). Results are, however, discordant, either due to differences in lactobacilli strains or case-mix. Uremic retention metabolites originating from bacterial protein fermentation p-Cresyl sulfate and indoxyl sulfate are the most extensively studied colon-derived uremic retention solutes. Both are related to overall mortality (66-68) and cardiovascular disease (69,70). Due to their 12 high protein binding, their removal with current dialysis techniques is rather limited. Interventions to decrease the intestinal production and/or absorption may be an appealing alternative (Figure 1). Interventions targeting intestinal production The generation of toxic microbial co-metabolites can be modulated by selectively increasing saccharolytic and reducing proteolytic bacteria in the colon. Probiotics Probiotics have been defined as “viable organisms that, when ingested in sufficient amounts, exert positive health effects” (127). Although numerous studies have evaluated the effects of probiotics, only a limited number have looked at their effects in renal disease, studying intermediate end-points, e.g., change in serum concentrations or urinary excretion of marker molecules (124,126,128-131) (Table 1). Studies investigating the impact of probiotics on hard clinical end-points (e.g., cardiovascular events, mortality) in renal disease have not been conducted to date. Antibiotics The composition of the colonic microbiome can be influenced by antibiotic therapy. Experience herein is mainly limited to patients with liver failure where therapy with rifaxamin appeared successful in preventing relapses of hepatic encephalopathy (132). Preliminary own data suggest that broad spectrum antibiotics lower p-cresol serum levels in maintenance peritoneal dialysis patients (unpublished). An ongoing prospective clinical trial aims to confirm these findings (ClinicalTrials.gov ID: NCT00433342). Prebiotics Another approach to reduce generation of bacterial metabolites is to increase the ratio of available carbohydrate to nitrogen, which, as outlined previously, is an important regulator of bacterial α13 amino nitrogen metabolism (25,26). The term prebiotic, first coined by Gibson and Roberfroid, refers to “a non-digestible food ingredient that beneficially affects the host by selectively stimulating the growth and/or activity of one or a limited number of bacteria in the colon, and thus improves host health” (127). Whereas numerous compounds are known to escape digestion in the small intestine, a limited number of molecules result in selective stimulation of microbiota. At present, only bifidogenic, non-digestible oligo- and polysaccharides (particularly inulin, its hydrolysis product oligofructose, and (trans)galacto-oligosaccharides) fulfill all the criteria for prebiotic classification (133). In a study of 9 patients with CKD but not yet on dialysis, it was found that fermentable carbohydrates shifted nitrogen excretion from the urinary route to fecal excretion, thereby reducing plasma urea concentrations (134). Whether this resulted in a decreased generation of other uremic retention solutes was not studied. A study in healthy volunteers has demonstrated lowering of urinary p-cresol excretion by the ingestion of a 50/50 v/v mixture of inulin and fructooligosaccharides (135). A recent phase I/II trial confirmed that p-cresol generation and p-cresyl sulfate serum concentrations were also lowered in hemodialysis patients by this prebiotic (136). Wheat bran extract, a food-grade preparation highly enriched in arabinoxylan oligosaccharides, is another prebiotic which has been shown to reduce urinary p-cresol excretion in healthy volunteers (137). A pilot study, investigating its benefits in CKD, will be initiated in the near future. Dietary fiber Fruit and vegetables are important sources of dietary fibers (i.e., non-digestible carbohydrates), and it was demonstrated that a vegetarian diet reduced urinary excretion of indoxyl sulfate and p-cresyl sulfate (138). Nonetheless, fruit and vegetables are often restricted in CKD because of their high potassium content. Limiting protein intake might also reduce generation of bacterial waste products, but its feasibility is questionable as it confers a risk of malnutrition. Drug therapy 14 An alternative method to increase delivery of fermentable carbohydrate to the colon is to inhibit small intestine assimilation by means of α-glucosidase inhibitors such as acarbose. This was already evaluated in healthy volunteers, showing significantly lower serum concentrations of p-cresol and the 24h urinary excretion of p-cresol (as a surrogate for colonic generation rate) (139). An intervention study looking at the effects of acarbose in patients with CKD is ongoing. Theoretically, the colonic transit time might be another therapeutic target. As colonic transit time is significantly prolonged in CKD (53), it could be hypothesized that selectively accelerating the colonic transit might be of benefit. Decreasing its transit time, e.g. by laxatives, might result in less time for bacterial proliferation, and less generation and absorption of their toxic waste products. Adsorptive strategies Therapeutic interventions may also reduce intestinal absorption through intraluminal adsorption onto high-affinity surfaces. AST-120 (Kremezin®, Kureha Chemical Industry) is an orally administered adsorbent consisting of spherical carbon particles 0.2–0.4 mm in diameter (140). It is capable of adsorbing significant amounts of various organic compounds in the large intestine, including indoxyl sulfate (141,142), p-cresol (143), and food-derived advanced glycation end-products (144). It has been shown to retard the progression of renal failure in Japanese patients with mild-to-moderate CKD (145,146). A phase II dose-finding study in US patients with CKD confirmed a dose-dependent reduction in indoxyl sulfate serum concentrations (142). A large, multicenter randomized trial is currently testing whether AST-120 can slow the progression of CKD (Evaluating Prevention of Progression In Chronic Kidney Disease (EPPIC-1/2); ClinicalTrials.gov ID: NCT00500682/NCT00501046). Preliminary results, however, appeared rather disappointing with no proven efficacy of AST-120, although subgroup analysis suggested that AST-120 may have its value in patients with acceptable compliance and risk factors of progression of CKD (147). Further studies are thus needed to clarify the role and benefit of AST-120 in CKD. Sevelamer hydrochloride (Renagel®, Genzyme), a non-metal-based phosphate binder, is another potentially useful adsorbent therapy. In 15 addition to phosphate binding, it has been shown to bind uremic retention solutes in vitro, including indole (10–15 %) and p-cresol (40–50 %, dependent on pH) (148). Despite this observation, sevelamer did not result in decreased serum concentrations of indoxyl sulfate or p-cresol, neither in a mouse model of CKD (149), nor in hemodialysis patients (150). CONCLUSION As is shown, a clear bi-directional interplay exists between the large intestine and the kidney. Many of these interactions are at least partly mediated by the colonic microbiome. The large intestine plays an ambiguous role in CKD. On the one hand, the colon contributes to the homeostasis of potassium and the disposal of nitrogenous waste products and oxalate, but on the other hand, the large intestine is an important source of uremic toxins. Parallel to the increased awareness of the importance of the host-microbiome interaction, therapies targeting the colon will undoubtedly gain interest in CKD and beyond. ACKNOWLEDGEMENTS RP is recipient of a Ph.D. fellowship of the Research Foundation - Flanders (FWO) (grant 11E9813N) 16 Reference List 1. Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS: Prevalence of chronic kidney disease in the United States. JAMA 298:2038-2047, 2007 2. Collins AJ, Foley R, Herzog C, Chavers B, Gilbertson D, Ishani A, Kasiske B, Liu J, Mau LW, McBean M, Murray A, St Peter W, Xue J, Fan Q, Guo H, Li Q, Li S, Li S, Peng Y, Qiu Y, Roberts T, Skeans M, Snyder J, Solid C, Wang C, Weinhandl E, Zaun D, Zhang R, Arko C, Chen SC, Dalleska F, Daniels F, Dunning S, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L: Excerpts from the United States Renal Data System 2007 annual data report. Am J Kidney Dis 51:S1-320, 2008 3. Sarnak MJ, Levey AS: Cardiovascular disease and chronic renal disease: a new paradigm. Am J Kidney Dis 35:S117-S131, 2000 4. Foley RN, Wang C, Collins AJ: Cardiovascular risk factor profiles and kidney function stage in the US general population: the NHANES III study. Mayo Clin Proc 80:1270-1277, 2005 5. Foley RN, Parfrey PS, Sarnak MJ: Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol 9:S16-S23, 1998 6. de Jager DJ, Grootendorst DC, Jager KJ, van Dijk PC, Tomas LM, Ansell D, Collart F, Finne P, Heaf JG, De Meester J, Wetzels JF, Rosendaal FR, Dekker FW: Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA 302:1782-1789, 2009 7. Eknoyan G, Beck GJ, Cheung AK, Daugirdas JT, Greene T, Kusek JW, Allon M, Bailey J, Delmez JA, Depner TA, Dwyer JT, Levey AS, Levin NW, Milford E, Ornt DB, Rocco MV, Schulman G, Schwab SJ, Teehan BP, Toto R: Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med 347:2010-2019, 2002 8. Paniagua R, Amato D, Vonesh E, Correa-Rotter R, Ramos A, Moran J, Mujais S: Effects of increased peritoneal clearances on mortality rates in peritoneal dialysis: ADEMEX, a prospective, randomized, controlled trial. J Am Soc Nephrol 13:1307-1320, 2002 9. Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, Held PJ, Port FK: Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 341:1725-1730, 1999 10. Aronov PA, Luo FJ, Plummer NS, Quan Z, Holmes S, Hostetter TH, Meyer TW: Colonic contribution to uremic solutes. J Am Soc Nephrol 22:1769-1776, 2011 11. Friedman EA: Bowel as a kidney substitute in renal failure. Am J Kidney Dis 28:943-950, 1996 12. Kolff WJ, Berk HT, ter Welle M, van der Ley AJ, van Dijk EC, van Noordwijk J: The artificial kidney: A dialyzer with a great area. Acta Med Scand. CXVII:121-134:121-134, 1944 13. Barry JM Murray JE: The first human renal transplants. J Urol 176:888-890, 2006 14. Brunner HR, Waeber B, Wauters JP, Turin G, McKinstry D, Gavras H: Inappropriate renin secretion unmasked by captopril (SQ 14 225) in hypertension of chronic renal failure. Lancet 2:704-707, 1978 17 15. Wilson M: Microbial Inhabitants of Humans: Their Ecology and Role in Health and Disease. Cambridge University Press, 2004 16. Gennari FJ Weise WJ: Acid-base disturbances in gastrointestinal disease. Clin J Am Soc Nephrol 3:1861-1868, 2008 17. Lozupone CA, Stombaugh JI, Gordon JI, Jansson JK, Knight R: Diversity, stability and resilience of the human gut microbiota. Nature 489:220-230, 2012 18. Tremaroli V Backhed F: Functional interactions between the gut microbiota and host metabolism. Nature 489:242-249, 2012 19. Maynard CL, Elson CO, Hatton RD, Weaver CT: Reciprocal interactions of the intestinal microbiota and immune system. Nature 489:231-241, 2012 20. Cummings JH: Fermentation in the human large intestine: evidence and implications for health. Lancet 1:1206-1209, 1983 21. Topping DL, Clifton PM: Short-chain fatty acids and human colonic function: roles of resistant starch and nonstarch polysaccharides. Physiol Rev 81:1031-1064, 2001 22. Roediger WE: Utilization of nutrients by isolated epithelial cells of the rat colon. Gastroenterology 83:424-429, 1982 23. Gibson SA, McFarlan C, Hay S, Macfarlane GT: Significance of microflora in proteolysis in the colon. Appl Environ Microbiol 55:679-683, 1989 24. Cummings JH, Hill MJ, Bone ES, Branch WJ, Jenkins DJ: The effect of meat protein and dietary fiber on colonic function and metabolism. II. Bacterial metabolites in feces and urine. Am J Clin Nutr 32:2094-2101, 1979 25. Birkett A, Muir J, Phillips J, Jones G, O'Dea K: Resistant starch lowers fecal concentrations of ammonia and phenols in humans. Am J Clin Nutr 63:766-772, 1996 26. Smith EA, Macfarlane GT: Enumeration of human colonic bacteria producing phenolic and indolic compounds: effects of pH, carbohydrate availability and retention time on dissimilatory aromatic amino acid metabolism. J Appl Bacteriol 81:288-302, 1996 27. Vince A, Dawson AM, Park N, O'Grady F: Ammonia production by intestinal bacteria. Gut 14:171-177, 1973 28. Vince AJ, Burridge SM: Ammonia production by intestinal bacteria: the effects of lactose, lactulose and glucose. J Med Microbiol 13:177-191, 1980 29. Vince A, Killingley M, Wrong OM: Effect of lactulose on ammonia production in a fecal incubation system. Gastroenterology 74:544-549, 1978 30. Vince AJ, McNeil NI, Wager JD, Wrong OM: The effect of lactulose, pectin, arabinogalactan and cellulose on the production of organic acids and metabolism of ammonia by intestinal bacteria in a faecal incubation system. Br J Nutr 63:17-26, 1990 31. Deguchi T, Kusuhara H, Takadate A, Endou H, Otagiri M, Sugiyama Y: Characterization of uremic toxin transport by organic anion transporters in the kidney. Kidney Int 65:162-174, 2004 18 32. Mathialahan T, Maclennan KA, Sandle LN, Verbeke C, Sandle GI: Enhanced large intestinal potassium permeability in end-stage renal disease. J Pathol 206:46-51, 2005 33. Hayes CP, Jr., McLeod ME, Robinson RR: An extrarenal mechanism for the maintenance of potassium balance in severe chronic renal failure. Trans Assoc Am Physicians 80:207-216, 1967 34. Wilson DR, Ing TS, Metcalfe-Gibson A, Wrong OM: The chemical composition of faeces in uraemia, as revealed by in-vivo faecal dialysis. Clin Sci 35:197-209, 1968 35. Fisher KA, Binder HJ, Hayslett JP: Potassium secretion by colonic mucosal cells after potassium adaptation. Am J Physiol 231:987-994, 1976 36. Kliger AS, Binder HJ, Bastl C, Hayslett JP: Demonstration of active potassium transport in the mammalian colon. J Clin Invest 67:1189-1196, 1981 37. Kashgarian M, Taylor CR, Binder HJ, Hayslett JP: Amplification of cell membrane surface in potassium adaptation. Lab Invest 42:581-588, 1980 38. Sandle GI, Foster ES, Lewis SA, Binder HJ, Hayslett JP: The electrical basis for enhanced potassium secretion in rat distal colon during dietary potassium loading. Pflugers Arch 403:433439, 1985 39. Foster ES, Sandle GI, Hayslett JP, Binder HJ: Cyclic adenosine monophosphate stimulates active potassium secretion in the rat colon. Gastroenterology 84:324-330, 1983 40. Turnamian SG, Binder HJ: Aldosterone and glucocorticoid receptor-specific agonists regulate ion transport in rat proximal colon. Am J Physiol 258:G492-G498, 1990 41. Rechkemmer G, Halm DR: Aldosterone stimulates K secretion across mammalian colon independent of Na absorption. Proc Natl Acad Sci U S A 86:397-401, 1989 42. Silva P, Charney AN, Epstein FH: Potassium adaptation and Na-K-ATPase activity in mucosa of colon. Am J Physiol 229:1576-1579, 1975 43. Sabbagh Y, Giral H, Caldas Y, Levi M, Schiavi SC: Intestinal phosphate transport. Adv Chronic Kidney Dis 18:85-90, 2011 44. Eckstein J, Savic S, Eugster T, Pargger H, Gurke L, Pechula M, Steiger J, Mayr M: Extensive calcifications induced by hyperphosphataemia caused by phosphate-based enema in a patient after kidney transplantation. Nephrol Dial Transplant 21:2013-2016, 2006 45. Hu MS, Kayne LH, Jamgotchian N, Ward HJ, Lee DB: Paracellular phosphate absorption in rat colon: a mechanism for enema-induced hyperphosphatemia. Miner Electrolyte Metab 23:7-12, 1997 46. Hatch M, Freel RW, Vaziri ND: Intestinal excretion of oxalate in chronic renal failure. J Am Soc Nephrol 5:1339-1343, 1994 47. Hatch M, Freel RW, Vaziri ND: Mechanisms of oxalate absorption and secretion across the rabbit distal colon. Pflugers Arch 426:101-109, 1994 48. Ley RE, Turnbaugh PJ, Klein S, Gordon JI: Microbial ecology: human gut microbes associated with obesity. Nature 444:1022-1023, 2006 19 49. Dicksved J, Halfvarson J, Rosenquist M, Jarnerot G, Tysk C, Apajalahti J, Engstrand L, Jansson JK: Molecular analysis of the gut microbiota of identical twins with Crohn's disease. ISME J 2:716727, 2008 50. Vaziri ND, Wong J, Pahl M, Piceno YM, Yuan J, Desantis TZ, Ni Z, Nguyen TH, Andersen GL: Chronic kidney disease alters intestinal microbial flora. Kidney Int, 2012, ePub ahead of print 51. Kalantar-Zadeh K, Kopple JD, Deepak S, Block D, Block G: Food intake characteristics of hemodialysis patients as obtained by food frequency questionnaire. J Ren Nutr 12:17-31, 2002 52. Bammens B, Verbeke K, Vanrenterghem Y, Evenepoel P: Evidence for impaired assimilation of protein in chronic renal failure. Kidney Int 64:2196-2203, 2003 53. Wu MJ, Chang CS, Cheng CH, Chen CH, Lee WC, Hsu YH, Shu KH, Tang MJ: Colonic transit time in long-term dialysis patients. Am J Kidney Dis 44:322-327, 2004 54. Lefebvre HP, Ferre JP, Watson AD, Brown CA, Serthelon JP, Laroute V, Concordet D, Toutain PL: Small bowel motility and colonic transit are altered in dogs with moderate renal failure. Am J Physiol Regul Integr Comp Physiol 281:R230-R238, 2001 55. Magnusson M, Magnusson KE, Sundqvist T, Denneberg T: Impaired intestinal barrier function measured by differently sized polyethylene glycols in patients with chronic renal failure. Gut 32:754-759, 1991 56. de Almeida Duarte JB, de Aguilar-Nascimento JE, Nascimento M, Nochi RJ, Jr.: Bacterial translocation in experimental uremia. Urol Res 32:266-270, 2004 57. Goncalves S, Pecoits-Filho R, Perreto S, Barberato SH, Stinghen AE, Lima EG, Fuerbringer R, Sauthier SM, Riella MC: Associations between renal function, volume status and endotoxaemia in chronic kidney disease patients. Nephrol Dial Transplant 21:2788-2794, 2006 58. Wang F, Jiang H, Shi K, Ren Y, Zhang P, Cheng S: Gut bacterial translocation is associated with microinflammation in end-stage renal disease patients. Nephrology (Carlton) 17:733-738, 2012 59. Vaziri ND, Yuan J, Rahimi A, Ni Z, Said H, Subramanian VS: Disintegration of colonic epithelial tight junction in uremia: a likely cause of CKD-associated inflammation. Nephrol Dial Transplant 27:2686-2693, 2012 60. Vaziri ND, Dure-Smith B, Miller R, Mirahmadi MK: Pathology of gastrointestinal tract in chronic hemodialysis patients: an autopsy study of 78 cases. Am J Gastroenterol 80:608-611, 1985 61. Krack A, Sharma R, Figulla HR, Anker SD: The importance of the gastrointestinal system in the pathogenesis of heart failure. Eur Heart J 26:2368-2374, 2005 62. Jakob SM, Ruokonen E, Vuolteenaho O, Lampainen E, Takala J: Splanchnic perfusion during hemodialysis: evidence for marginal tissue perfusion. Crit Care Med 29:1393-1398, 2001 63. McIntyre CW, Harrison LE, Eldehni MT, Jefferies HJ, Szeto CC, John SG, Sigrist MK, Burton JO, Hothi D, Korsheed S, Owen PJ, Lai KB, Li PK: Circulating endotoxemia: a novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. Clin J Am Soc Nephrol 6:133-141, 2011 64. Ritz E: Intestinal-renal syndrome: mirage or reality? Blood Purif 31:70-76, 2011 20 65. Meyer TW, Hostetter TH: Uremic solutes from colon microbes. Kidney Int 81:949-954, 2012 66. Barreto FC, Barreto DV, Liabeuf S, Meert N, Glorieux G, Temmar M, Choukroun G, Vanholder R, Massy ZA: Serum indoxyl sulfate is associated with vascular disease and mortality in chronic kidney disease patients. Clin J Am Soc Nephrol 4:1551-1558, 2009 67. Liabeuf S, Barreto DV, Barreto FC, Meert N, Glorieux G, Schepers E, Temmar M, Choukroun G, Vanholder R, Massy ZA: Free p-cresylsulphate is a predictor of mortality in patients at different stages of chronic kidney disease. Nephrol Dial Transplant 25:1183-1191, 2010 68. Bammens B, Evenepoel P, Keuleers H, Verbeke K, Vanrenterghem Y: Free serum concentrations of the protein-bound retention solute p-cresol predict mortality in hemodialysis patients. Kidney Int 69:1081-1087, 2006 69. Meijers BK, Bammens B, De Moor B, Verbeke K, Vanrenterghem Y, Evenepoel P: Free p-cresol is associated with cardiovascular disease in hemodialysis patients. Kidney Int 73:1174-1180, 2008 70. Meijers BK, Claes K, Bammens B, de Loor H, Viaene L, Verbeke K, Kuypers D, Vanrenterghem Y, Evenepoel P: p-Cresol and cardiovascular risk in mild-to-moderate kidney disease. Clin J Am Soc Nephrol 5:1182-1189, 2010 71. Wu IW, Hsu KH, Lee CC, Sun CY, Hsu HJ, Tsai CJ, Tzen CY, Wang YC, Lin CY, Wu MS: p-Cresyl sulphate and indoxyl sulphate predict progression of chronic kidney disease. Nephrol Dial Transplant 26:938-947, 2011 72. Dou L, Jourde-Chiche N, Faure V, Cerini C, Berland Y, Dignat-George F, Brunet P: The uremic solute indoxyl sulfate induces oxidative stress in endothelial cells. J Thromb Haemost 5:13021308, 2007 73. Motojima M, Hosokawa A, Yamato H, Muraki T, Yoshioka T: Uremic toxins of organic anions upregulate PAI-1 expression by induction of NF-kappaB and free radical in proximal tubular cells. Kidney Int 63:1671-1680, 2003 74. Dou L, Bertrand E, Cerini C, Faure V, Sampol J, Vanholder R, Berland Y, Brunet P: The uremic solutes p-cresol and indoxyl sulfate inhibit endothelial proliferation and wound repair. Kidney Int 65:442-451, 2004 75. Meijers BK, Van Kerckhoven S, Verbeke K, Dehaen W, Vanrenterghem Y, Hoylaerts MF, Evenepoel P: The uremic retention solute p-cresyl sulfate and markers of endothelial damage. Am J Kidney Dis 54:891-901, 2009 76. Tumur Z, Niwa T: Indoxyl sulfate inhibits nitric oxide production and cell viability by inducing oxidative stress in vascular endothelial cells. Am J Nephrol 29:551-557, 2009 77. Lekawanvijit S, Adrahtas A, Kelly DJ, Kompa AR, Wang BH, Krum H: Does indoxyl sulfate, a uraemic toxin, have direct effects on cardiac fibroblasts and myocytes? Eur Heart J 31:17711779, 2010 78. Gelasco AK, Raymond JR: Indoxyl sulfate induces complex redox alterations in mesangial cells. Am J Physiol Renal Physiol 290:F1551-F1558, 2006 21 79. Miyazaki T, Ise M, Hirata M, Endo K, Ito Y, Seo H, Niwa T: Indoxyl sulfate stimulates renal synthesis of transforming growth factor-beta 1 and progression of renal failure. Kidney Int Suppl 63:S211-S214, 1997 80. Meyer TW, Leeper EC, Bartlett DW, Depner TA, Lit YZ, Robertson CR, Hostetter TH: Increasing dialysate flow and dialyzer mass transfer area coefficient to increase the clearance of proteinbound solutes. J Am Soc Nephrol 15:1927-1935, 2004 81. Einheber A Carter D: The role of the microbial flora in uremia. I. Survival times of germfree, limited-flora, and conventionalized rats after bilateral nephrectomy and fasting. J Exp Med 123:239-250, 1966 82. Iseki K, Uehara H, Nishime K, Tokuyama K, Yoshihara K, Kinjo K, Shiohira Y, Fukiyama K: Impact of the initial levels of laboratory variables on survival in chronic dialysis patients. Am J Kidney Dis 28:541-548, 1996 83. Mathialahan T, Sandle GI: Dietary potassium and laxatives as regulators of colonic potassium secretion in end-stage renal disease. Nephrol Dial Transplant 18:341-347, 2003 84. Imbriano LJ, Durham JH, Maesaka JK: Treating interdialytic hyperkalemia with fludrocortisone. Semin Dial 16:5-7, 2003 85. Nyman N, Mulgaonkar S, Walcer R, Viscuso R, Jacobs MG: Effects of a mineralocorticoid on extra-renal potassium (K+) homeostasis in anuric patients. Kidney Int 23:155A-1983 86. Singhal PC, Desroches L, Mattana J, Abramovici M, Wagner JD, Maesaka JK: Mineralocorticoid therapy lowers serum potassium in patients with end-stage renal disease. Am J Nephrol 13:138-141, 1993 87. Kim DM, Chung JH, Yoon SH, Kim HL: Effect of fludrocortisone acetate on reducing serum potassium levels in patients with end-stage renal disease undergoing haemodialysis. Nephrol Dial Transplant 22:3273-3276, 2007 88. Furuya R, Kumagai H, Sakao T, Maruyama Y, Hishida A: Potassium-lowering effect of mineralocorticoid therapy in patients undergoing hemodialysis. Nephron 92:576-581, 2002 89. Matsumoto Y, Kageyama S, Mori Y, Yakushigawa T, Arihara K: Spironolactone Reduces Cardioand Cerebrovascular Morbidity and Mortality in Hemodialysis Patients, (abstract) J Am Soc Nephrol 23:36A, 2012 90. Scherr L, Ogden DA, Mead AW, Ritz N, Rubin AL: Management of hyperkalemia with a cationexchange resin. N Engl J Med 264:115-119, 1961 91. Watson M, Abbott KC, Yuan CM: Damned if you do, damned if you don't: potassium binding resins in hyperkalemia. Clin J Am Soc Nephrol 5:1723-1726, 2010 92. Sterns RH, Rojas M, Bernstein P, Chennupati S: Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective? J Am Soc Nephrol 21:733-735, 2010 93. Gerstman BB, Kirkman R, Platt R: Intestinal necrosis associated with postoperative orally administered sodium polystyrene sulfonate in sorbitol. Am J Kidney Dis 20:159-161, 1992 22 94. Young EW, Albert JM, Satayathum S, Goodkin DA, Pisoni RL, Akiba T, Akizawa T, Kurokawa K, Bommer J, Piera L, Port FK: Predictors and consequences of altered mineral metabolism: the Dialysis Outcomes and Practice Patterns Study. Kidney Int 67:1179-1187, 2005 95. Dhingra R, Sullivan LM, Fox CS, Wang TJ, D'Agostino RB, Sr., Gaziano JM, Vasan RS: Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Arch Intern Med 167:879-885, 2007 96. Kestenbaum B, Sampson JN, Rudser KD, Patterson DJ, Seliger SL, Young B, Sherrard DJ, Andress DL: Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol 16:520-528, 2005 97. Lopes AA, Tong L, Thumma J, Li Y, Fuller DS, Morgenstern H, Bommer J, Kerr PG, Tentori F, Akiba T, Gillespie BW, Robinson BM, Port FK, Pisoni RL: Phosphate binder use and mortality among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS): evaluation of possible confounding by nutritional status. Am J Kidney Dis 60:90-101, 2012 98. Ogawa T, Shimada M, Nagano N, Ito K, Ando T, Shimomura Y, Ando Y, Otsuka K: Oral administration of Bifidobacterium longum in a gastro-resistant seamless capsule decreases serum phosphate levels in patients receiving haemodialysis. Clinical Kidney Journal 5:373-374, 2012 99. Crocetti GR, Hugenholtz P, Bond PL, Schuler A, Keller J, Jenkins D, Blackall LL: Identification of polyphosphate-accumulating organisms and design of 16S rRNA-directed probes for their detection and quantitation. Appl Environ Microbiol 66:1175-1182, 2000 100. Hirota R, Kuroda A, Kato J, Ohtake H: Bacterial phosphate metabolism and its application to phosphorus recovery and industrial bioprocesses. J Biosci Bioeng 109:423-432, 2010 101. Erdman JW, Macdonald IA, Zeisel SH: Present Knowledge in Nutrition (10th edition). International Life Sciences Institute, 2012 102. Marangella M, Petrarulo M, Cosseddu D, Vitale C, Linari F: Oxalate balance studies in patients on hemodialysis for type I primary hyperoxaluria. Am J Kidney Dis 19:546-553, 1992 103. Marangella M, Vitale C, Petrarulo M, Tricerri A, Cerelli E, Cadario A, Barbos MP, Linari F: Bony content of oxalate in patients with primary hyperoxaluria or oxalosis-unrelated renal failure. Kidney Int 48:182-187, 1995 104. Elgstoen KB, Johnsen LF, Woldseth B, Morkrid L, Hartmann A: Plasma oxalate following kidney transplantation in patients without primary hyperoxaluria. Nephrol Dial Transplant 25:23412345, 2010 105. Pinheiro HS, Camara NO, Osaki KS, De Moura LA, Pacheco-Silva A: Early presence of calcium oxalate deposition in kidney graft biopsies is associated with poor long-term graft survival. Am J Transplant 5:323-329, 2005 106. Jaeger P, Robertson WG: Role of dietary intake and intestinal absorption of oxalate in calcium stone formation. Nephron Physiol 98:64-71, 2004 107. Pardi DS, Tremaine WJ, Sandborn WJ, McCarthy JT: Renal and urologic complications of inflammatory bowel disease. Am J Gastroenterol 93:504-514, 1998 23 108. Duffey BG, Alanee S, Pedro RN, Hinck B, Kriedberg C, Ikramuddin S, Kellogg T, Stessman M, Moeding A, Monga M: Hyperoxaluria is a long-term consequence of Roux-en-Y Gastric bypass: a 2-year prospective longitudinal study. J Am Coll Surg 211:8-15, 2010 109. Ahmed MH Byrne CD: Bariatric surgery and renal function: a precarious balance between benefit and harm. Nephrol Dial Transplant 25:3142-3147, 2010 110. Marshall RW, Cochran M, Hodgkinson A: Relationships between calcium and oxalic acid intake in the diet and their excretion in the urine of normal and renal-stone-forming subjects. Clin Sci 43:91-99, 1972 111. Caravaca F, Ruiz AB, Escola JM, Hernandez GR, Cerezo I, Fernandez N, Barroso S, Martin MV: Either calcium carbonate or sevelamer decreases urinary oxalate excretion in chronic renal failure patients. Nefrologia 27:466-471, 2007 112. Lieske JC, Regnier C, Dillon JJ: Use of sevelamer hydrochloride as an oxalate binder. J Urol 179:1407-1410, 2008 113. Emmett M, Guirl MJ, Santa Ana CA, Porter JL, Neimark S, Hofmann AF, Fordtran JS: Conjugated bile acid replacement therapy reduces urinary oxalate excretion in short bowel syndrome. Am J Kidney Dis 41:230-237, 2003 114. Stauffer JQ: Hyperoxaluria and intestinal disease. The role of steatorrhea and dietary calcium in regulating intestinal oxalate absorption. Am J Dig Dis 22:921-928, 1977 115. Caspary WF, Tonissen J, Lankisch PG: 'Enteral' hyperoxaluria. Effect of cholestyramine, calcium, neomycin, and bile acids on intestinal oxalate absorption in man. Acta Hepatogastroenterol (Stuttg) 24:193-200, 1977 116. Kelly JP, Curhan GC, Cave DR, Anderson TE, Kaufman DW: Factors related to colonization with Oxalobacter formigenes in U.S. adults. J Endourol 25:673-679, 2011 117. Sidhu H, Schmidt ME, Cornelius JG, Thamilselvan S, Khan SR, Hesse A, Peck AB: Direct correlation between hyperoxaluria/oxalate stone disease and the absence of the gastrointestinal tract-dwelling bacterium Oxalobacter formigenes: possible prevention by gut recolonization or enzyme replacement therapy. J Am Soc Nephrol 10 Suppl 14:S334-S340, 1999 118. Hatch M, Cornelius J, Allison M, Sidhu H, Peck A, Freel RW: Oxalobacter sp. reduces urinary oxalate excretion by promoting enteric oxalate secretion. Kidney Int 69:691-698, 2006 119. Jiang Z, Asplin JR, Evan AP, Rajendran VM, Velazquez H, Nottoli TP, Binder HJ, Aronson PS: Calcium oxalate urolithiasis in mice lacking anion transporter Slc26a6. Nat Genet 38:474-478, 2006 120. Hatch M, Gjymishka A, Salido EC, Allison MJ, Freel RW: Enteric oxalate elimination is induced and oxalate is normalized in a mouse model of primary hyperoxaluria following intestinal colonization with Oxalobacter. Am J Physiol Gastrointest Liver Physiol 300:G461-G469, 2011 121. Hoppe B, Beck B, Gatter N, von UG, Tischer A, Hesse A, Laube N, Kaul P, Sidhu H: Oxalobacter formigenes: a potential tool for the treatment of primary hyperoxaluria type 1. Kidney Int 70:1305-1311, 2006 24 122. Hoppe B, Dittlich K, Fehrenbach H, Plum G, Beck BB: Reduction of plasma oxalate levels by oral application of Oxalobacter formigenes in 2 patients with infantile oxalosis. Am J Kidney Dis 58:453-455, 2011 123. Hoppe B, Groothoff JW, Hulton SA, Cochat P, Niaudet P, Kemper MJ, Deschenes G, Unwin R, Milliner D: Efficacy and safety of Oxalobacter formigenes to reduce urinary oxalate in primary hyperoxaluria. Nephrol Dial Transplant 26:3609-3615, 2011 124. Lieske JC, Goldfarb DS, De Simone C, Regnier C: Use of a probiotic to decrease enteric hyperoxaluria. Kidney Int 68:1244-1249, 2005 125. Lieske JC, Tremaine WJ, De Simone C, O'Connor HM, Li X, Bergstralh EJ, Goldfarb DS: Diet, but not oral probiotics, effectively reduces urinary oxalate excretion and calcium oxalate supersaturation. Kidney Int 78:1178-1185, 2010 126. Goldfarb DS, Modersitzki F, Asplin JR: A randomized, controlled trial of lactic acid bacteria for idiopathic hyperoxaluria. Clin J Am Soc Nephrol 2:745-749, 2007 127. Chow J: Probiotics and prebiotics: A brief overview. J Ren Nutr 12:76-86, 2002 128. Hida M, Aiba Y, Sawamura S, Suzuki N, Satoh T, Koga Y: Inhibition of the accumulation of uremic toxins in the blood and their precursors in the feces after oral administration of Lebenin, a lactic acid bacteria preparation, to uremic patients undergoing hemodialysis. Nephron 74:349-355, 1996 129. Campieri C, Campieri M, Bertuzzi V, Swennen E, Matteuzzi D, Stefoni S, Pirovano F, Centi C, Ulisse S, Famularo G, De SC: Reduction of oxaluria after an oral course of lactic acid bacteria at high concentration. Kidney Int 60:1097-1105, 2001 130. Takayama F, Taki K, Niwa T: Bifidobacterium in gastro-resistant seamless capsule reduces serum levels of indoxyl sulfate in patients on hemodialysis. Am J Kidney Dis 41:S142-S145, 2003 131. Taki K, Takayama F, Niwa T: Beneficial effects of Bifidobacteria in a gastroresistant seamless capsule on hyperhomocysteinemia in hemodialysis patients. J Ren Nutr 15:77-80, 2005 132. Bass NM, Mullen KD, Sanyal A, Poordad F, Neff G, Leevy CB, Sigal S, Sheikh MY, Beavers K, Frederick T, Teperman L, Hillebrand D, Huang S, Merchant K, Shaw A, Bortey E, Forbes WP: Rifaximin treatment in hepatic encephalopathy. N Engl J Med 362:1071-1081, 2010 133. de Vrese M, Schrezenmeir J: Probiotics, prebiotics, and synbiotics. Adv Biochem Eng Biotechnol 111:1-66, 2008 134. Younes H, Egret N, Hadj-Abdelkader M, Remesy C, Demigne C, Gueret C, Deteix P, Alphonse JC: Fermentable carbohydrate supplementation alters nitrogen excretion in chronic renal failure. J Ren Nutr 16:67-74, 2006 135. De Preeter V, Vanhoutte T, Huys G, Swings J, De Vuyst L, Rutgeerts P, Verbeke K: Effects of Lactobacillus casei Shirota, Bifidobacterium breve, and oligofructose-enriched inulin on colonic nitrogen-protein metabolism in healthy humans. Am J Physiol Gastrointest Liver Physiol 292:G358-G368, 2007 25 136. Meijers BK, De Preeter V, Verbeke K, Vanrenterghem Y, Evenepoel P: p-Cresyl sulfate serum concentrations in haemodialysis patients are reduced by the prebiotic oligofructose-enriched inulin. Nephrol Dial Transplant 25:219-224, 2010 137. Francois IE, Lescroart O, Veraverbeke WS, Marzorati M, Possemiers S, Evenepoel P, Hamer H, Houben E, Windey K, Welling GW, Delcour JA, Courtin CM, Verbeke K, Broekaert WF: Effects of a wheat bran extract containing arabinoxylan oligosaccharides on gastrointestinal health parameters in healthy adult human volunteers: a double-blind, randomised, placebocontrolled, cross-over trial. Br J Nutr:1-14, 2012, ePub ahead of print 138. Patel KP, Luo FJ, Plummer NS, Hostetter TH, Meyer TW: The production of p-cresol sulfate and indoxyl sulfate in vegetarians versus omnivores. Clin J Am Soc Nephrol 7:982-988, 2012 139. Evenepoel P, Bammens B, Verbeke K, Vanrenterghem Y: Acarbose treatment lowers generation and serum concentrations of the protein-bound solute p-cresol: a pilot study. Kidney Int 70:192-198, 2006 140. Marier JF, Guilbaud R, Kambhampati SR, Mathew P, Moberly J, Lee J, Salazar DE: The effect of AST-120 on the single-dose pharmacokinetics of losartan and losartan acid (E-3174) in healthy subjects. J Clin Pharmacol 46:310-320, 2006 141. Niwa T, Nomura T, Sugiyama S, Miyazaki T, Tsukushi S, Tsutsui S: The protein metabolite hypothesis, a model for the progression of renal failure: an oral adsorbent lowers indoxyl sulfate levels in undialyzed uremic patients. Kidney Int Suppl 62:S23-S28, 1997 142. Schulman G, Agarwal R, Acharya M, Berl T, Blumenthal S, Kopyt N: A multicenter, randomized, double-blind, placebo-controlled, dose-ranging study of AST-120 (Kremezin) in patients with moderate to severe CKD. Am J Kidney Dis 47:565-577, 2006 143. Niwa T, Ise M, Miyazaki T, Meada K: Suppressive effect of an oral sorbent on the accumulation of p-cresol in the serum of experimental uremic rats. Nephron 65:82-87, 1993 144. Yamagishi S, Nakamura K, Matsui T, Inoue H, Takeuchi M: Oral administration of AST-120 (Kremezin) is a promising therapeutic strategy for advanced glycation end product (AGE)related disorders. Med Hypotheses 69:666-668, 2007 145. Owada A, Nakao M, Koike J, Ujiie K, Tomita K, Shiigai T: Effects of oral adsorbent AST-120 on the progression of chronic renal failure: a randomized controlled study. Kidney Int Suppl 63:S188-S190, 1997 146. Shoji T, Wada A, Inoue K, Hayashi D, Tomida K, Furumatsu Y, Kaneko T, Okada N, Fukuhara Y, Imai E, Tsubakihara Y: Prospective randomized study evaluating the efficacy of the spherical adsorptive carbon AST-120 in chronic kidney disease patients with moderate decrease in renal function. Nephron Clin Pract 105:c99-107, 2007 147. Schulman G, Berl T, Beck GJ, Remuzzi G, Eberhard R: EPPIC (Evaluating Prevention of Progression In Chronic Kidney Disease): Results from 2 Phase III, Randomized, PlaceboControlled, Double-Blind Trials of AST-120 in Adults with CKD, (abstract) ASN 2012 148. De Smet R, Thermote F, Lameire N, Vanholder R: Sevalemer hydrochloride adsorbs the uremic compounds indoxyl sulfate, (abstract) J Am Soc Nephrol 14: 206A: 2004 26 149. Phan O, Ivanovski O, Nguyen-Khoa T, Mothu N, Angulo J, Westenfeld R, Ketteler M, Meert N, Maizel J, Nikolov IG, Vanholder R, Lacour B, Drueke TB, Massy ZA: Sevelamer prevents uremiaenhanced atherosclerosis progression in apolipoprotein E-deficient mice. Circulation 112:28752882, 2005 150. Brandenburg VM, Schlieper G, Heussen N, Holzmann S, Busch B, Evenepoel P, Vanholder R, Meijers B, Meert N, Fassbender WJ, Floege J, Jahnen-Dechent W, Ketteler M: Serological cardiovascular and mortality risk predictors in dialysis patients receiving sevelamer: a prospective study. Nephrol Dial Transplant 25:2672-2679, 2010 27 FIGURES Figure 1: The colon as a source of uremic retention solutes: pathophysiology and therapeutic targets Colonic microbial metabolism can be roughly categorized as saccharolytic (carbohydrate fermentation, e.g., Prevotella) or proteolytic (protein fermentation, e.g., Bacteroides). Carbohydrate and protein fermentation predominate in the right and left colon, respectively. Saccharolytic metabolism is considered beneficial with generation of short-chain fatty acids, whereas proteolytic metabolism may generate toxic solutes such as p-cresol and indole. Colon-related therapies targeting these solutes can be divided in those modulating the microbiome, microbial metabolism and adsorption. (SCFA’s: Short-chain fatty acids; CHO: Carbohydrate) 28 TABLES Table 1: Studies with probiotic preparations in kidney disease Study Hida et al.(128) Campieri et al.(129) Lieske et al.(124) Goldfarb et al.(126) Takayama et al.(130). Taki et al.(131) Primary end-point Indoxyl sulfate p-Cresol Urinary oxalate excretion Urinary oxalate excretion Urinary oxalate excretion Indoxyl sulfate n 20 Strain Lactic acid bacilli (Lebenin) 6 10 10a 11 Indoxyl sulfate Homocysteine 27 Lactic acid bacilli Lactic acid bacilli (Oxadrop) Lactic acid bacilli (Oxadrop) Bifidobacterium longum (Bifina) Bifidobacterium longum (Bifina) n, number of patients in active treatment arm aRandomized controlled trial 29 Result ─30% serum indoxyl sulfate No change serum p-cresol ─40% Urinary oxalate excretion ─19% Urinary oxalate excretion No significant changes ─30% serum indoxyl sulfate ─9% serum indoxyl sulfate ─9% plasma homocysteine