File
advertisement
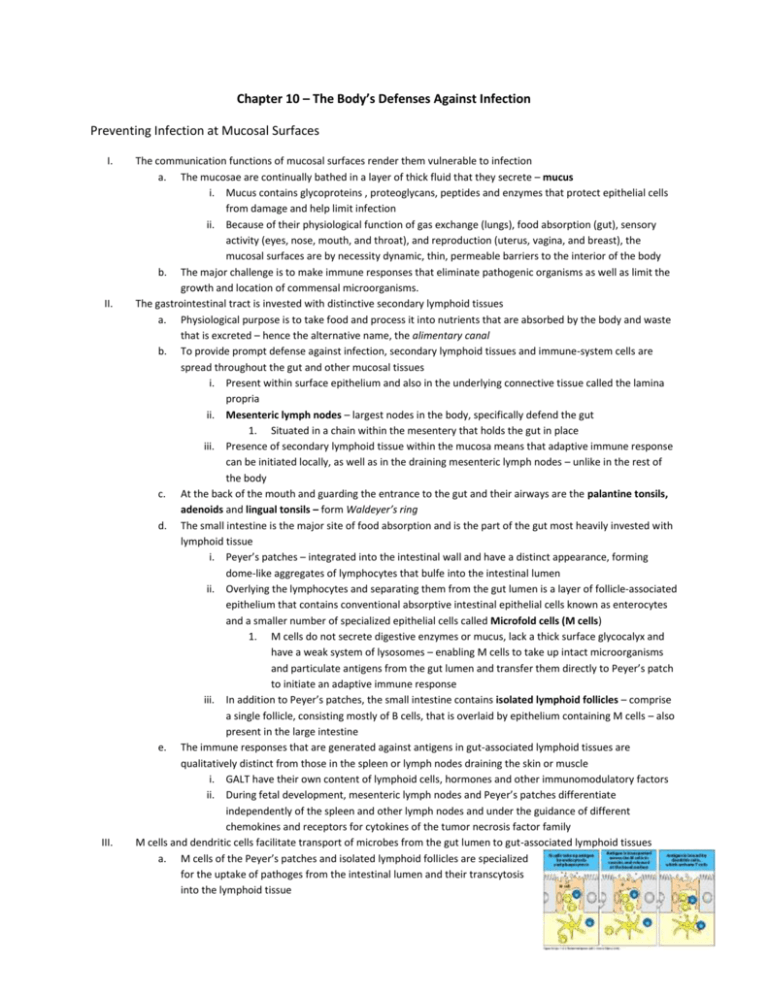
Chapter 10 – The Body’s Defenses Against Infection Preventing Infection at Mucosal Surfaces I. II. III. The communication functions of mucosal surfaces render them vulnerable to infection a. The mucosae are continually bathed in a layer of thick fluid that they secrete – mucus i. Mucus contains glycoproteins , proteoglycans, peptides and enzymes that protect epithelial cells from damage and help limit infection ii. Because of their physiological function of gas exchange (lungs), food absorption (gut), sensory activity (eyes, nose, mouth, and throat), and reproduction (uterus, vagina, and breast), the mucosal surfaces are by necessity dynamic, thin, permeable barriers to the interior of the body b. The major challenge is to make immune responses that eliminate pathogenic organisms as well as limit the growth and location of commensal microorganisms. The gastrointestinal tract is invested with distinctive secondary lymphoid tissues a. Physiological purpose is to take food and process it into nutrients that are absorbed by the body and waste that is excreted – hence the alternative name, the alimentary canal b. To provide prompt defense against infection, secondary lymphoid tissues and immune-system cells are spread throughout the gut and other mucosal tissues i. Present within surface epithelium and also in the underlying connective tissue called the lamina propria ii. Mesenteric lymph nodes – largest nodes in the body, specifically defend the gut 1. Situated in a chain within the mesentery that holds the gut in place iii. Presence of secondary lymphoid tissue within the mucosa means that adaptive immune response can be initiated locally, as well as in the draining mesenteric lymph nodes – unlike in the rest of the body c. At the back of the mouth and guarding the entrance to the gut and their airways are the palantine tonsils, adenoids and lingual tonsils – form Waldeyer’s ring d. The small intestine is the major site of food absorption and is the part of the gut most heavily invested with lymphoid tissue i. Peyer’s patches – integrated into the intestinal wall and have a distinct appearance, forming dome-like aggregates of lymphocytes that bulfe into the intestinal lumen ii. Overlying the lymphocytes and separating them from the gut lumen is a layer of follicle-associated epithelium that contains conventional absorptive intestinal epithelial cells known as enterocytes and a smaller number of specialized epithelial cells called Microfold cells (M cells) 1. M cells do not secrete digestive enzymes or mucus, lack a thick surface glycocalyx and have a weak system of lysosomes – enabling M cells to take up intact microorganisms and particulate antigens from the gut lumen and transfer them directly to Peyer’s patch to initiate an adaptive immune response iii. In addition to Peyer’s patches, the small intestine contains isolated lymphoid follicles – comprise a single follicle, consisting mostly of B cells, that is overlaid by epithelium containing M cells – also present in the large intestine e. The immune responses that are generated against antigens in gut-associated lymphoid tissues are qualitatively distinct from those in the spleen or lymph nodes draining the skin or muscle i. GALT have their own content of lymphoid cells, hormones and other immunomodulatory factors ii. During fetal development, mesenteric lymph nodes and Peyer’s patches differentiate independently of the spleen and other lymph nodes and under the guidance of different chemokines and receptors for cytokines of the tumor necrosis factor family M cells and dendritic cells facilitate transport of microbes from the gut lumen to gut-associated lymphoid tissues a. M cells of the Peyer’s patches and isolated lymphoid follicles are specialized for the uptake of pathoges from the intestinal lumen and their transcytosis into the lymphoid tissue b. IV. V. Transcytosis releases microorganisms at the M cells basal membrane. Here, dendritic cells take up microbes to process and present their antigens to naïve T cells i. Antigen-loaded dendritic cells either migrate from the dome region to the T cell area of the Peyer’s patch, or via the draining lymphatics to a mesenteric lymph node, where they meet and stimulate antigen-specific naïve T cells c. Dendritic cells resident in the lamina propria outside the organized lymphoid tissues can also capture pathogens independently of M cells i. In response to infection these dendritic cells become more mobile – move into epithelial wall or send processes through it that can capture microbes and antigens without disturbing the integrity of the epithelial barrier ii. The dendritic cells then move into the T cell area of the GALT or travel into draining lymph to the T cell area of a mesenteric lymph node, to stimulate antigen specific T cells Effector lymphocytes populate healthy mucosal tissue in the absence of infection a. Integrated into the epithelial layer of the small intestine is a distinctive type of CD8 T cell called the intraepithelial lymphocyte – which have been actiated by antigen and contain intracellular granules like those of CD8 cytotoxic T cells i. Intraepithelial lymphocytes can either be α:β CD8 T cells or ϒ:δ CD8 T cells ii. Express T cell receptors with a limited range of antigen specificities and they have a distinctive combination of chemokine receptors and adhesion molecules that enables them to take up their unique position within the intestinal epithelium b. The lamina propria contains a variety of effector lymphocytes – CD4 T cells, CD8 T cells and plasma cells - as well as dendritic cells and the occasional eosinophils or mast cell c. In contrast to skin and other tissues, the healthy intestinal mucosa sustains a chronic adaptive immune response i. Achieved by constant sampling of gut’s contents by M cells and dendritic cells, as well as the continual stimulation of B and T cells in a myriad of local immune responses in the GALT 1. Most of the foreign antigens are innocuous – do not create a state of inflammation of symptoms of disease ii. Because of their chronic state of stimulation, lymphocytes in the mucosal surface are able to respond quickly to any breach of the mucosal barrier and prevent inundation of the mucosal tissue with the gut contents B cells and T cells commit to mucosal lymphoid tissues after they encounter their specific antigen a. Naïve B and T cells that emerge from primary lymphoid organs are not restricted in their recirculation – can recirculate via the lymph and blood through both the mucosal and systemic compartments of the immune system i. Naïve B and T cells enter the Peyer’s patches and mesenteric lymph nodes from the blood via high endothelial venules, attracted by chemokines CCL21 and CCL19, which are released by the lymphoid organ and bind CCR7 on naïve lymphocytes 1. If the lymphocyte does not recognize specific antigen – continues recirculation 2. If the lymphocyte does recognize specific antigen – retained in Peyer’s patches/mesenteric lymph node and is activated to proliferate and differentiate into effector and memory lymphocytes a. Activation is accompanied by loss of CCR7 and cell-adhesion molecule Lselectin, and thus the ability to enter secondary lymphoid tissues from blood b. B and T cells activated in a Peyer’s patch leave in the lymph and travel via mesenteric lymph nodes to the thoracic duct to the blood ; those activated in mesenteric lymph node leave in efferent lymph and them reach the blood c. Once in the bloodstream, mucosally activated lymphocytes home to the type of mucosa in which they were activated and enter it from the blood i. VI. VII. Gut homing effector lymphocytes express integrin α4:β7, which binds specifically to the mucosal vascular addressin MAdCAM-1 present on endothelial cells of blood vessels in the gut wall ii. Guiding lymphocytes into gut tissue is chemokine CCL25, which is secreted by epithelium of the small intestine and binds CCR9 on effector lymphocytes iii. By this route, activated lymphocytes enter lamina propria – B cells develop into plasma cells making secretory IgA and T cells activate intestinal macrophages ii. Only lymphocytes that first encounter antigen in GALT are induced to express gut-specific homing receptors and integrins 1. Induction is under control of intestinal dendritic cells and is mediated by retinoic acid, a derivative of vitamin A made by these cells 2. Analogous tissue specificity are acquired by effector T cells activated in non-mucosal tissues Effector lymphocytes activated in any one mucosal tissue recirculate through all mucosal tissues a. MAdCAM-1 is not restricted to intestinal blood vessels but is also present on the vasculature serving other mucosal tissues i. As a result, B and T cells first activated in GALT can recirculate as effector cells to the respiratory tract and vice versa. Thus, secondary lymphoid tissues of mucosal surfaces form a unified and exclusive network of recirculation of effector cells b. Naïve B cells activated in Peyer’s patches and mesenteric lymph nodes preferentially undergo isotype switching to IgA, the dominant antibody in mucosal secretions i. Process is directed by cytokine transforming growth factor (TGF-β) abd occurs in the organized lymphoid tissues of the gut ii. After B cell activation and differentiation, cells express α4:β7 and CCR9. Effector B cells leave secondary lymphoid tissue in efferent lymph and travel to the blood – some will then return to lamina propria close to where they were activated and others will go to lamina propria in the same, as well as different, tissue iii. In lamina propria, B cells differentiate into plasma cells and synthesize intact J-chain-linked IgA dimers which are secreted into the sub-epithelial space, from where they are transcytosed by poly-Ig and delivered to mucosal surface c. In nursing mothers, activated B cells will home from the mucosal tissues to the lactating mammary gland and contribute their dimeric IgA to the breast milk – will represent all antibody response the mother has recently made to microorganisms, food and infections ; passed to infant – provide comprehensive protective mucosal immunity directed toward normal gut flora and endemic pathogens Dimeric IgA binds pathogens at various sites in mucosal tissues a. Dimeric IgA is secreted in mucosal tissues by plasma cells that derive from B cells activated in the mucosal immune system i. Dimeric IgA can bind antigens and pathogens at several different locations 1. VIII. IX. X. XI. In the lamina propria IgA can bind pathogens and antigens and carry them to intestinal lumen on transcytosis. 2. During transcytosis, free IgA can bind pathogens and antigens that have been internalized into endosomes 3. IgA that has been secreted and is present at mucosal surface can bind pathogens and toxins in the gut lumen 4. Secreted IgA can bind pathogens on an M cell surface and by passing through the M cell can take them into the secondary lymphoid tissue 5. As free IgA passes through an M cell, it can bind pathogens in the endosomes and take them into secondary lymphoid tissue Two subclasses of IgA have complementary properties for controlling microbial populations a. The two IgA subclasses differ mainly in the hinge region, which is twice as long in IgA1 than in IgA2 i. The drawback to the longer hinge region is the increased susceptibility to proteolytic cleavage 1. Major bacterial pathogens have evolved specific proteases that cleave the IgA1 hinge and separate the Fc and Fab regions, preventing antibody from targeting the bacteria – bacteria coated with Fab fragments of IgA1 can become more able to adhere to mucosal epithelium, penetrate physical barrier, and gain access to lamina propria ii. In the case where IgA1 is cleaved by proteases, IgA2 synthesis helps control the infection – bacteria have yet to evolve a protease that can cleave IgA2 b. Normally the switch to IgA secretion goes from IgM to IgA1, but in the presence of TNF-family cytokine APRIL, isotype switches from IgM to IgA2 Humans with selective deficiency of IgA do not succumb to infection a. Selective IgA deficiency – little to no IgA, but makes all other immunoglobulin isotypes b. Most people are healthy, and are often oblivious to their lack of antibody – lack of IgA is compensated for by increased production of other isotypes i. Most importantly IgM because it can be secreted by mucosal tissues by the same mechanism as dimeric IgA because it contains the J chain necessary for binding to the poly-Ig receptor c. Chronic lung disease is more common in people with IgA deficiency in industrialized countries Intestinal epithelial cells contribute to innate defense of the gut a. To detect the presence of bacteria in their cytoplasm, epithelial cells have intracellular sensors called nucleotide-binding oligomerization domain proteins NOD proteins – structurally related to the toll-like receptors i. NOD1 recognizes a muramyl tripeptide that contains diaminopimelic acid, which is present only in the cell walls of G- bacteria ii. NOD2 recognizes a muramyl dipeptide present in the peptidoglycans of most bacterial cell walls b. Binding to its ligand causes NOD protein form oligomers that activate the protein kinase RICK which turns on NFκB signaling pathway in the epithelial cell. This causes the cell to make and release cytokines, chemokines and antibacterial defensins Intestinal helminth infections provoke strong TH2 mediated immune responses a. Parasites cause disease by competing with the host for nutrients or by causing local damage to epithelial cells or blood vessels b. Characteristic of immunity to almost all helminth infections is that a response dominated by TH2 CD4 T cells is protective, whereas a TH1 biased response fails to eliminate the pathogen and produces inflammatory response that damages mucosal surfaces of human host i. Bias toward TH2 is cause by worm products that influence the dendritic cells presenting worm antigens ii. Major antibody – IgE –binding releases major basic protein and other cytotoxic molecules that damage and kill the worms iii. Mast cells activated by worm antigens bound to IgE release mediators such as histamine that cause the smooth muscle to contract, helping to expel the worm Immunological memory and the secondary immune response XII. The antibodies formed during a primary immune response prevent reinfection for several months after disease a. After successful termination of infection by the primary immune response, elevated levels of high-affinity pathogen-specific antibody will be present in the blood and lymph or at mucosal surfaces