blood bank samples
advertisement

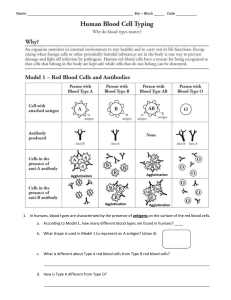
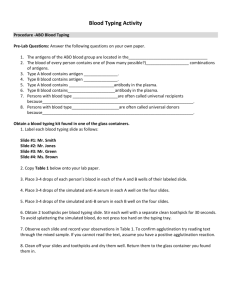
Life's Blood Table of Contents CLASS NOTES LABORATORY TECHNIQUES: REAGENTS, REACTION GRADING; CELL WASHING; SAMPLE COLLECTION BLOOD BANKING REAGENTS The techniques used in Blood Bank involve mixing antigens, usually on red blood cells with antibodies. The environment where this reaction occurs can range in temperature from 4oC to 37oC. With the most common being room temperature for ABO and the initial Rh(D) testing and 37oC when screening and identifying other clinically significant antigen-antibody reactions. In a number of situations we are looking for particular antigens on the red cell such as looking for A or B antigens to determine a patient's ABO type. Other times we may be looking for particular antibodies that may cause transfusion reactions or hemolytic disease of the newborn. Depending on whether we are looking for a particular antigen or antibody will determine what reagents we are going to use. If we are looking for an A antigen on a patient's red cells, we will use known anti-A reagent that will cause agglutination of the A antigens on the red cells. If the patient has on B antigens or no ABO antigens, as in the case of an O individual, their cells will not agglutinate with anti-A reagent. Sources of Antigen Testing: In almost all blood bank techniques we have red cells with antigens present. These red cells may either reagent red cells with known antigens, patient red cells, or donor red cells. The reagent red cells are commercially prepared and have all the red cell antigens identified. When we use red cells where the antigens have already been determined, we can identify the possible antibodies present. For example: Anti-A and Anti-B are expected antibodies in patient's who lack that particular antigen. Therefore if a patient or donor has only the A antigen on their red cells, then they should have anti-B in their serum. When we test their serum with A1 and B cells, agglutination will occur with the B cells and not with the A1cells since they have an anti-B. The reagent cells used for blood banking include the following: A1 and B cells for confirmation of the ABO type in all patients and donors other than newborn babies Antibody screening cells are O cells that have been studied to determine the presence of a number of antigens for specific antibodies that are known to cause transfusion reactions and hemolytic disease of the newborn. The antibody screening technique is part of all compatibility tests done before blood is transfused. Some of the more common antibodies detected are anti-D, anti-E, anti-K. Antibody identification cell panel are again O cells with the specific antigens known. Usually there are between 8 and 12 different cells in a cell panel. The pattern of positive and negative reactions helps identify the antibody. Sources of Antibody for Testing Antibody is found in serum. If it is the patient's serum that is being tested, we do not know what antibody may be present so we are using one of the 3 types of reagent cells listed about. If the serum is commercial reagent, the specific antibody present is already known. The commercial serum reagent is referred to as antisera. Therefore, we use Anti-A antisera to determine if a patient or donor is Type A. If we are trying to determine if the patient is Rh + or Rh -, we will use anti-Rho (D) antisera. Table 1 is a summary of known and unknown sources of both antigens and antibodies. Known Source with known components Antigen Reagent Red Blood Cells Antibody Commercial Antisera Table 1 Unknown components - The source is either the patient or the donor Patient or Donor red blood cells Patient or Donor serum or plasma Testing Procedures Routinely Done in Blood Banking In a transfusion service there are a number procedures routinely done. The ones noted in red are those done even in small hospitals whereas the rest are more likely done at larger hospitals and reference laboratories: ABO/Rh(D) typing Antigen typing from other blood group systems such as Rh antigens other than D, Kell, Kidd, and Duffy Antibody screening for antibodies form to blood group antigens other than A and B Antibody identification to determine the specific antibodies detected in the antibody screening Crossmatch, or compatibility testing, which determines whether donor blood can probably be safely transfused to the recipient Table 2 summarizes the sources of both the antigen and antibody (Modified from Basic & Applied Concepts of Immunology, Blaney and Howard, lst ed., p. 39 Procedure ABO/Rh typing Purpose Source of Antigen Detects A, B, and D Patient's RBC's Source of Antibody Commercial anti-A, Antigen typing Detects antigens of other blood group Patient's RBC's or systems (examples: Donor RBC's K, E, C, Fya, Jka) Detects antibodies Commercial Antibody screening with specificity of Screening Cells RBC antigens Identifies the Antibody Commercial Panel specificity of RBC identification Cells antibodies Determines serologic compatibility between Crossmatch Donor RBC's donor and patient before transfusion anti-B, and anti-D Commercial antisera to the specific antigens (examples: anti-K, anti-E, anti-C, anti-Fya, anti-Jka) Patient's serum Patient's serum Patient's serum GRADING REACTIONS Grading agglutination reactions gives an indication of the relative amount of antigen or antibody present. All tubes tests should be graded. The technique used in the resuspension of the cells will affect the grading of the reaction. The correct procedure for resuspending and grading reactions follow: 1. Resuspension Procedure: use lighted agglutination viewer read only one tube at a time hold tube upright position cell button so it is facing you in the mirror very gently shake the tube and observe how the cells come off the cell button 2. Grading Reactions swirling off = negative coming off in chunks = positive continue shaking till all cells resuspended tilt tube, read and grade reaction 3. Grading system: 4+ = solid clump 3+ = several large clumps 2+ = small to medium sized clumps; clear background 1+ = small clumps; cloudy background +w = tiny aggregates; cloudy background + micro = positive upon microscopic examination only MF = mixed field. Small clumps amidst many unagglutinated cells. Can be confused with 1+ hem = hemolyzed (a positive reaction) neg = negative, no agglutination (Never use - for negative; either write neg or 0) WASHED CELL SUSPENSIONS 3% Red Blood Cell Concentration in Saline Between 2-5% cell suspension provides optimum antigen concentration for the tube method for red blood cells typing. To make sure your suspension is within this range use reagent red cells for comparison. Washing Red Blood Cells Before Making the 3% Suspension The purpose of washing the red blood cells is to remove plasma, which contains substance that may interfere with antigen-antibody reaction. The following may be in the plasma and may interfere with testing: Soluble antigens such as A and B may be present and neutralize your reagent. Interfering proteins such as Wharton's jelly that is seen in newborn cord blood, cold-acting autoimmune antibodies, and increased levels of immunoglobulins that may cause either agglutination or rouleaux.. Hemolyzed red blood cells due to a difficult draw will interfere in your grading interpretation of hemolysis Fibrinogen can result in fibrin strands forming that makes grading reactions difficult. Good Technique when washing and making a 3% cell suspension involves the following: Place 1 to 3 drops of blood in the tube Aim the tip of the saline bottle towards the center of the tube and forcibly squirt saline into the tube. Fill the tube 3/4 full of saline (there will be less splattering in the centrifuge) Centrifuge long enough spin to pull most of cells into a button in the bottom of the tube. Decant the saline completely Shake the tube to resuspend cell button before washing the cells again. It will depend on the procedure being done as to how many washings are going to be done. COLLECTING BLOOD BANK SAMPLES Samples for Blood Bank Testing Most samples for blood banking are drawn into a red top tube - serum is preferred. (No clot activation tube should be used since the patient's red cells may also need to used and no other chemicals should be present) A few tests require an EDTA sample if complement is not to be activated. Serum must be tested while fresh to ensure good complement activity. Antigens on cells are stable longer (months) in a clot tube. Patient Identification The patient MUST be positively identified and preferably banded. Some institutions use specific Blood Bank arm bands. Ask patient to state his/her name. Responsible party should identify patient if he/she cannot. Verify information by comparing to ID band. Resolve any differences before proceeding with the blood draw. Labeling of Sample The information on sample MUST match information on ID band, which would also need to be consistent with the order. Information on samples MUST include the following: Name (last, first, middle initial) and no nicknames. Unique identification number such as medical record number or possibly social security number. Date and time sample drawn along with the signature or unique identifier of phlebotomist (on sample or on orders) Gender and birthdate desirable but not mandatory. The date of birth provides another unique identifier along with the medical record number and full name of the patient. Mislabeled Samples Do NOT accept any sample not properly labeled. The following are what would warrant an improperly labeled specimen: Missing information Incorrect information Information on sample not matching information on orders Improperly labeled samples must be discarded if the problem cannot be resolved. In the case of an emergency blood draw on a patient who is unidentified at that time, the blood specimen must also discarded when both name and medical record number have changed (ex. John Doe, #12240253 becomes Jack Adams # 37859012) unless ID tags with both sets of information remain in place OBJECTIVES - GRADING REACTIONS; WASHED CELL SUSPENSIONS; BLOOD BANK SAMPLES Identify sources of antigen and antibody used in testing. Explain why it is important to grade agglutination reactions. Describe the proper resuspension technique Explain how the resuspension technique affects the graded result Describe how each of the following looks: 4+, 3+, 2+, 1+, w+, micro +, hem., MF, neg 6. State the optimum % cell concentration for blood bank testing 7. Explain why the above concentration is best 8. Describe the proper technique for adequate washing of cells 9. Explain how you can tell if your cell suspensions are the proper concentration 10. Name four plasma (or serum) constituents washing removes, and tell why it is desirable to remove them before doing blood bank testing 11. Describe the proper procedure for identifying a patient when obtaining a sample for blood bank testing 12. Explain what should be done if there is a discrepancy in the patient's identification 13. State the information required on all samples for blood banking testing 14. Explain why gender and birthdate are helpful. 1. 2. 3. 4. 5. Performance objectives: 1. Correctly prepare washed 3% suspensions of patient or donor red cells for blood bank testing 2. Utilize the proper resuspension technique to read agglutination reactions 3. Properly obtain a sample for blood bank testing, including use of proper tubes, identification of patient, and labeling of samples