PFP - South Carolina Hospital Association
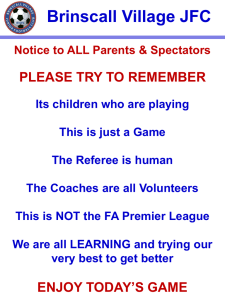
advertisement

Partnership for Patients Background On July 6, 2011, the Center for Medicare & Medicaid Services (CMS) Center for Medicare and Medicaid Innovation (The Innovation Center) announced that it will spend more than $200 million to help hospitals reduce preventable readmissions by 20 percent and preventable hospital-acquired conditions by 40 percent through the Partnership for Patients (PFP) initiative. This is a two-year program with a third year option. Under the Affordable Care Act and the 2009 stimulus law, hospitals have 6 percent of their reimbursement at risk for failure to achieve quality goals such as reduced readmissions, harm prevention and adherence to evidence-based best practices. This program will help hospitals develop the processes, understand the measures and share knowledge to be best prepared for the time when the reimbursement penalties take effect. Hospitals that do not participate in this program will run the risk of falling further behind, as this program will raise the bar for all hospitals. This will increase the likelihood of payment penalties for low-performing hospitals. And we anticipate that these sorts of penalties will extend to Medicaid and private payors over time. Members of the Premier alliance are already accomplishing many of the goals of the PFP, and Premier’s QUEST® program was a model for this program. This initiative is a perfect fit for our alliance, as we have done this work for more than a decade. Given this alignment between the goals of the Innovation Center and Premier’s own longstanding work in the area of quality improvement and harm reduction, Premier has been selected as one of the Hospital Engagement Networks (HENs). The program is expected to start at the end of 2011. Participation in PFP is free of charge to hospitals, but hospitals may only join one HEC. All hospitals are eligible for this program including critical access, rehabilitation and long-term acute care hospitals. Highlights of Premier’s Hospital Engagement Contractor approach Some key highlights of our approach: We will use Premier’s proven Collaborative Methodology™ to drive the improvement, which has powered programs such as HQID™ and the QUEST collaboratives, which have set a performance standard for the nation. A data submission portal will enable easy reporting of the measures and allow benchmarking and tracking progress within the cohort. For those who use Premier products, the majority of the data submission is already automated. More than 540 hospitals have signed Letters of Intent (LOIs) to work with Premier. Additionally, more than 100 hospitals will work as Affinity Teams through the South Carolina Hospital Association, the Healthcare Association of Hawaii, and Yankee Alliance and will share learnings across the cohorts. The Premier team has aligned with industry leaders as subcontractors: Booz Allen Hamilton, Health Research and Analysis (HRA), StrategyGen, and Millennium Services 2000+ Incorporated. Subject matter experts will help guide our efforts and engage with participating members: o Harlan Krumholz, MD, will be an expert advisor on readmissions and measurement. o Atul Gawande, MD, will be an expert advisor on patient safety, surgical infections and process improvement. o Healthcare Performance Improvement (HPI) will be a lead advisor for culture change and leadership education and training. o The Institute for Healthcare Improvement (IHI) will serve as an advisor on our overall approach to harm reduction. A clinical improvement advisor will be assigned to each participating organization. This skilled facilitator and quality improvement expert will carry a caseload of up to 30 hospitals, with a goal to deliver customized information and knowledge that helps accelerate improvement. The Premier and Affinity Teams will use information provided by CMS’ designated national content developer, and employ a range of performance improvement efforts designed to support hospitals in efforts to reduce hospitalacquired conditions (HACs)by 40 percent and readmissions by 20 percent. The offerings will address readmissions, 10 HACs, leadership engagement and cultural change. The specific HACs covered are: adverse drug events (ADE), catheter-associated urinary tract infections (CAUTI), central line-associated bloodstream infections (CLABSI), injuries from falls and immobility, obstetrical adverse events, pressure ulcers, preventable readmissions, surgical site infections, venous thromboembolism (VTE), and ventilator-associated pneumonia (VAP). The improvement and knowledge sharing delivery modalities will include: Sprints o A Sprint is a short-term, rapid-cycle improvement webinar series to drive change in specific indicators or processes of care. Conducted over 90 to 120 days and typically self-directed, the Sprint consists of up to four webinar learning sessions that are 60 to 90 minutes in length. Mini-collaboratives o Mini-collaboratives rely on a structured model, providing participants an opportunity to work together, set specific goals, share ideas and information, run tests, measure progress, implement changes, and share results. A mini-collaborative is a six- to nine-month initiative focused on a specific condition, disease state, or process of care. o Sprints and mini-collaboratives focused on each of the 10 harm areas (HACs) will be staggered so that hospitals will be able to adequately plan for each learning activity and provide available staff resources for training. Face-to-face national meetings o Premier hosts biannual in-person meetings to provide an additional forum to share best practices and organizational successes. Each meeting is a peer-to-peer learning session where all best practices and change concepts developed will be made transparent and openly discussed. Regional meetings and best practice open houses o Premier will host regional best-practice meetings in months four, 10, 16, and 22 of the two-year contract. In each region, we will also identify facilities to host open houses for attendees. Premier Performance Improvement Portal™ o This dynamic online community of industry specialists, hospital and health system peers, and Premier knowledge experts is dedicated to quality improvement. Users can access the portal’s extensive library of clinical, operational and financial best practice tools, templates and methodologies gleaned from the nation’s top performers to improve hospital performance. Leadership and culture change programming o Premier will conduct specific programming on leadership and culture change, to be conducted with C-suite hospital executives and subject matter experts from Healthcare Process Improvement (HPI), who specialize in this type of training and engagement. Premier will also offer three four-hour-long sessions at both inperson national meetings dedicated to leadership and culture change issues, presented in a mixed didactic/interactive workshop format. Because of the diversity of organizations, the curriculum must be flexible; meet the needs of varied roles, expertise and education levels within regions; and be offered via multiple methods of delivery (e.g., self-paced, in-person, virtual and case studies).