In vitro evaluation of antimicrobial activity of
advertisement

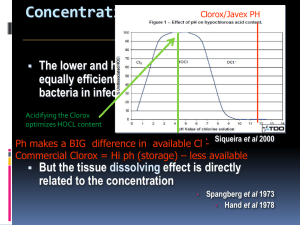
Waad M. Kheder, BDS, MSc (Conservative Dentistry), MSc /Dental specialtyProsthodontics. University of Toronto/ Toronto, Ontario/ Canada In vitro evaluation of antimicrobial activity of chlorhexidine and sodium hypochlorite irrigant solutions Abstract: The aim of this study is to investigate in vitro the antimicrobial activeness by the agar diffusion test two different concentrations of two endodontic irrigants 0.1% or 0.2 % chlorhexidine and1% or 3% sodium hypochlorite to Staphylococcus aureus, Enterococcus faecalis, Pseudomonas aeruginosa, Escherichia coli and a mixer of these species. Under the condition of the agar diffusion test, all solutions has exhibited zones of antimicrobial activity; however, chlorhexidine had the best antimicrobial effectiveness for both Staphylococcus aureus and Enterococcus facealis in both concentrations, while sodium hypochlorite has the best antimicrobial effectiveness against Pseudomonas aeruginosa even with 1% concentration. On the other hand, low concentration of chlorhexidine has been effective as the high concentration of sodium hypochlorite for Escherichia Coli and the mixed culture of four types of the bacteria are used in our study. Sodium hypochlorite and chlorhexidine gluconate at all tested concentrations can be used as irrigating solutions owing to their antimicrobial properties. Key words: agar diffusion test, antimicrobial activity, chlohexidine, endodontic irrigant, sodium hypochlorite Introduction: Chemo mechanical debridement of the root canal is an important phase of endodontic treatment. Elimination of pulpal tissue, microbiote and their by-products, organic and inorganic debris by mechanical instrumentation and chemical irrigation are objectives of this essential part of endodontic procedure. Despite all efforts to achieve a root canal system free of bacteria, it is evident that bacteria can still survive in areas that are not accessible to current cleaning and shaping procedures.1Irrigation is an essential part of root canal debridement because it allows for cleaning beyond what might be achieved by root canal instrumentation alone. However; the endodontic success has been directly related to the presence of negative bacterial culture before root canal filling.2 Although, various irrigant solutions have been indicated for the root canal disinfection and many of them have shown varied degrees of antimicrobial effectiveness, the choice of the ideal irrigant solution and its concentration is a challenge. Byström and Sundqvist has showed that there is no antibacterial difference between 0.5% and 5% sodium hypochlorite (NaOCl) solutions.3 Heling and Chandler by analyzing the antimicrobial effect of irrigants, they concluded that 0.12% chlorhexidine (CHX) and 1% NaOCl were similarly effective.4 While Ohara et al. compared six irrigants on selected anaerobic bacteria and they concluded that 0.2% CHX was the most effective, 5.25% NaOCl was less effective while the saline proved to be totally ineffective.5 Ayhan et al. reported the antimicrobial effects of various endodontic irrigants on selected microorganisms and observed that 5.25% NaOCl was superior and the reduced concentration of 0.5% resulted in significantly decreased antimicrobial effectiveness.6 Facultative microorganisms such as Enterococcus faecalis (E. faecalis), Staphylococcuc aureus (S. aureus), and even Candida albicans (C. albicans) are considered to be the most resistant species in the oral cavity, and one possible cause of root canal treatment failure.7 An endodontic irrigant should ideally exhibit powerful antimicrobial activity, dissolve organic tissue remnants, disinfect the root canal space, flush out debris from the instrumented root canals, provide lubrication, and have no cytotoxic effects on the periradicular tissues, among other properties.8 NaOCl has many of these properties but it has a cytotoxic effect when injected into the periapical tissues, a foul smell and taste, a tendency to bleach clothes, and corrosive potential. It is also noticed to produce allergic reactions.9 Therefore, an equally effective but safer irrigant is desirable. CHX is widely used as a mouth rinse in the prevention and treatment of periodontal diseases and dental caries, and has been suggested as an irrigating solution or intracanal dressing in endodontic therapy. The antimicrobial properties of both irrigating solutions have been tested against E. faecalis.9 However, their antimicrobial activity against microorganisms such S. aureus and C. albicans, which are also considered to be resistant to endodontic therapy, has not been well investigated yet. Therefore, the aim of this study is to investigate in vitro, the antimicrobial activeness by the agar diffusion test, two different concentrations of two endodontic irrigants solutions (0.1% or 0.2 % CHX and1% or 3% sodium hypochlorite) against S. aureus , E. faecalis, Psedomonas aeruginosa (P. aeruginosa), Escherichia coli (E. coli) and a mixed culture of these bacteria. Materials and method Four reference bacterial strains – S. aureus (ATCC 29213), E. faecalis (ATCC 29212), P. aeruginosa (ATCC 27853), and E. coli (ATCC 25922), has been obtained from American Type Culture Collection, and one mixture of these is also included in the study. The strains were inoculated in 7 ml brain heart infusion (BHIA; Difco Laboratories, Detroit, MI, USA) and incubated at 37oC for 24 h. The 5 biological indicators were cultivated on the surface of brain heart infusion agar (BHIA; Difco Laboratories, Detroit, MI, USA) following the same incubation conditions. Microbial cells were resuspended in saline to give a final concentration of about 3 x 108 cells/ml, similar to that of tube #1 of the Mac Farland scale. One ml of each of these pure suspensions has been used to obtain a mixture of the test microorganisms. The irrigant solutions tested in this experiment were 1%, %3 NaOCl, 0.2%, 0.1% CHX, and sterile distilled water. Twenty five Petri plates with 20 ml of BHIA were inoculated with 0.1 ml of the microbial suspensions, using sterile swabs that were spread on the medium, obtaining growth in junction. Seventy five paper disks (9 mm in diameter) were immersed in the experimental solutions for 1 min and then 3 paper disks were placed over the BHIA surface in each agar plate. The plates were maintained for 1 hour at room temperature, and then incubated at 37oC for 48 hours. The diameter of microbial inhibition was measured around the paper disks containing the substances. Positive and negative controls were done, maintaining the plates inoculated and without inoculums, for the same time periods and under identical incubation conditions. (Positive and negative controls consisted of plates incubated for the same period under identical conditions with and without inocula) All assays were carried out under aseptic conditions. This procedure has been done in the microbiology lab of Gulf Medical college (Dubai,UAE). RESULTS: The antimicrobial activities of 1%, 3% NaOCl, 0.2%, 0.1% CHX, and sterile distilled water are shown in Table 1. The saline control groups did not inhibit growth of any of the microorganisms tested. The magnitude of antimicrobial effect was influenced by the concentration of irrigant solutions. The positive control has showed bacterial growth, while the negative control has showed no growth. CHX had the best antimicrobial effectiveness for both S. aureus and E. facealis in both concentrations, while NaOCl had the best antimicrobial effectiveness against P. aeruginosa even with 1% concentration. On the other hand, low concentration of CHX was as effective as the high concentration of NaOCl for E. Coli and the mixed culture of the four types of the bacteria used in our experiment. Discussion: NaOCl solution is, to date, the most commonly employed root canal irrigant, but no general agreement exists regarding its optimal concentration, which ranges from 0.5% to 5.25%. According to our study, the antimicrobial effectiveness of NaOCl is proportional to its concentration. In order to reduce the cytotoxic effects, 1% NaOCl is recommended. The high pH of NaOCl interferes in cytoplasmic membrane integrity with irreversible enzymatic inhibition, biosynthetic alterations in cell metabolism and phospholipid destruction observed in lipidicperoxidation. The amino acid chloramination reaction forming chloramines interferes in cell metabolism. Oxidation promotes irreversible enzymatic inhibition of bacteria replacing hydrogen with chlorine. Enzyme inactivation can be observed in the reaction of chlorine with amino groups (NH2-) and an irreversible oxidation of sulphydryl groups (SH) of bacteria enzymes (cystein). Thus, NaOCl presents antimicrobial activity with action on bacterial essential enzymatic sites promoting irreversible inactivation originated by hydroxyl ions and chloramination action. Dissolution of organic tissue can be verified in the saponification reaction when NaOCl destroys fatty acids and lipids resulting in soap and glycerol.10,11 CHX has been recommended as an alternative irrigating solution to NaOCl, especially in cases of open apex owing to its biocompatibility or in cases of related allergy to bleaching solutions.12 CHX is a cationic agent (biguanide group; 4chlorophenyl radical), which exhibits antibacterial activity. The cationic nature of the compound promotes connection with anionic compound at the bacterial surface (phosphate groups from teicoic acid at Gram-positive and lipopolysaccharide at Gram-negative bacteria) capable of altering its integrity. The potassium ion, being a small entity, is the first substance to appear when the cytoplasmic membrane is damaged. The alteration of the cytoplasmic membrane permeability promotes precipitation of cytoplasmic proteins, alters cellular osmotic balance, interferes with metabolism, growth, cell division, inhibits the membrane ATPase and inhibits the anaerobic process.13,14,15 Various results have been reported for irrigant antimicrobial effectiveness. Similar results have been reported for NaOCl and CHX16,4,12 ; however, another research has shown that NaOCl has better antimicrobial activity than CHX 6,17,18, or, conversely, that CHX has better antimicrobial activity than NaOCl 5,19. Different experimental methods, biological indicators, concentrations, exposure time or the period of analysis may have caused these differences. The irrigant of choice should be one that exerts its antimicrobial activity against the majority of microorganisms found in the root canal and dentinal tubules. Other properties beyond antimicrobial activity must also be investigated before the final collection of an irrigant solution, such as minimum inhibitory concentration, tissue dissolution capacity, detoxification of endotoxin and acceptable biological compatibility. For this reason, it is important to know both the type of an irrigant to kill microorganisms and the irrigant’s minimum concentration that provide these requirements. In the present work, the highest antimicrobial effectiveness was for 0.2% CHX against all tested microorganisms except P. aeruginosa; On the other hand, there is no significant difference between the antimicrobial effectiveness of 1% & 3% NAOCl against P. aeruginosa. Although P. aeruginosa is not frequently isolated from root canals, it has been considered, because it is a bacterium that is too difficult to eliminate from root canals.20 The combination of NaOCl and chlorhexidine forms a precipitate. This NaOCl/CHX precipitate tends to occlude the dentinal tubules. Therefore; caution should be exercised when irrigating with NaOCl and CHX.21 We have concluded that NaOCl and chlorhexidine gluconate at all tested concentrations can be used as irrigating solutions owing to their antimicrobial properties. However using both types of irrigants as alternative steps during treatment is advised to get the benefits of both and avoid NaOCl/CHX precipitate formation on the same time. By using NaOCl we will overcome the shortcoming of CHX as CHX does not dissolve organic tissues. References: 1- Byström A, Sundqvist G. Bacteriologic evaluation of the efficacy of mechanical root canal instrumentation in endodontic therapy. Scand J Dent Res 1981; 89:321328. 2- Sjogren U, Figdor S, Persson S, et al. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. J Endod 1997; 30:297-306. 3- Byström A, Sundqvist G. The antibacterial action of sodium hypochlorite and EDTA in 60 cases of endodontic therapy. Int Endod J 1985; 18:35-40. 4- Heling I, Chandler NP. Antimicrobial effect of irrigant combinations within dentinal tubules. Int Endod J 1998; 31:8-14. 5- Ohara PK, Torabinejad M, Kettering JD. Antibacterial effect of various endodontic irrigants on selected anaerobic bacteria. Endod Dent Traumatol 1993; 9:95-100. 6- Ayhan H, Sultan N, Cirak M, Ruhi MZ, Bodur H. Antimicrobial effects of various endodontic irrigants on selected microorganisms. Int Endod J 1999; 32:99-102. 7- Gomes BPFA, Drucker DB, Lilley JD. Association of endodontic symptoms and signs with particular combinations of specific bacteria. Int Endod J 1996; 29:69-75. 8- Harrison JW. Irrigation of the root canal system. Dent Clin North Am 1984; 4:797-808. 9- Morgana Eli Vianna, ,Brenda P. F. A. Gomes, Vanessa Bellocchio Berber, Alexandre Augusto Zaia, Caio Cezar Randi Ferraz, and Francisco Jose´ de SouzaFilho. In vitro evaluation of the antimicrobial activity of chlorhexidine and sodium hypochlorite. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004; 97:79-84. 10- Estrela C, Estrela CRA, Barbin EL, Spanó JC, Marchesan MA, Pécora JD. Mechanism of action of sodium hypochlorite. Braz Dent J 2002; 2:113-117. 11- Baumgartner JC, Cuenin PR. Efficacy of several concentrations of sodium hypochlorite for root canal irrigation. J Endod 1992; 18:605-12. 12- Jeansonne MJ, White RR.A comparison of 2.0% chlorhexidine gluconate and 5.25% sodium hypochlorite as antimicrobial endodontic irrigants. J Endod 1994; 20:276-278. 13- Rolla G, Melsen B.On the mechanism of the plaque inhibition by chlorhexidine. J Dent Res 1975; 54:57-62. 14- Jenkins S, Addy M, Wade W.The mechanism of action of chlorhexidine. J Clin Periodontol 1988; 15:415-424. 15- Greenstein G., Berman C, Jaffin R. Chlorhexidine: an adjunct to periodontal therapy. J Periodontol 1986; 57:370-377. 16- Gomes BPFA, Ferraz CCR, Vianna ME, Berber VB, Teixeira FB, Souza-Filho FJ.In vitro antimicrobial activity of several concentrations of sodium hypochlorite and chlorhexidine gluconate in the elimination of Enterococcus faecalis. Int Endod J 2001; 34: 424-428. 17- Ringel AM, Patterson SS, Newton CW, Miller CH, Mulhern JM. In vivo evaluation of chlorhexidine gluconate solution and sodium hypochlorite solution as root canal irrigants. J Endod1982; 8:200-204. 18- Siqueira JF, Batista MD, Fraga RC, Uzeda M. Antimicrobial effects of endodontic irrigants on black-pigmented Gram-negative anaerobes and facultative bacteria. J Endod 1998; 24:414-416. 19- Silva CAG. Efetividade an timicrobiana do hipoclorito de sódio eclorexidina como irrigantes endodônticos. [Master’s thesis]. Porto Alegre: Universidade Luterana de Brasil, 1999. 20- Yoshida M, Kimura K, Fukushima Hisanori, Toda T. Treatment of Tooth with Incurable Periapical Pathosis Using Chair-side Anaerobic Incubation System-A Case with Persistent Aerobic Gram-negative Rod Infection. Japanese Journal of Conservative Dentistry 2000; 439(2):383-389. 21- Tung BB, Baumgartner J C and John CM. Evaluation of the Interaction between Sodium Hypochlorite and Chlorhexidine Gluconate and its Effect on Root Dentin. J Endod 2008; 34(2):181-185. Table 1. Means of the diameters (in mm) of the inhibition zones by the agar diffusion test. S. aureus 1% NaOCl 3%NaO Cl 0.2%CH X 0.1%CH X Distilled water E.faceali s P. aeruginosa E . Coli Mixture 14.3mm 12.7mm 16mm 14.7mm 13.3mm 14.5+14+ 12.6+12 16.1+16 15.1+14.6 13.4+13.2 14.3 .8+12.7 .3+16.5 +14.3 +13.3 19mm 14mm 17.7mm 17.3mm 15.7mm 19.3+18.7 13.8+14 17.6+18 17.2+17.3 15.5+15.6 +19 .1+14.2 +17.4 +17.4 +16.9 24mm 22mm 14.7mm 19.3mm 17.3mm 24.1+23.9 21.7+22 14.6+14 19.2+19.5 17.4+17.1 +24 .3+22 .5+14.9 +19.3 +17.4 21.7mm 17.3mm 12mm 17mm 15.7mm 21.7+22+ 17.1+17 11.8+11 16.8+16.9 15.2+15.7 21.4 0 .4+17.5 0 .9+12.3 0 +17.3 0 +16.1 0 30 25 20 S. aureus E.facealis 15 P. aeruginosa E . Coli 10 Mixture 5 0 1% NaOCl 3%NaOCl 0.2%CHX 0.1%CHX Distilled water Graph 1: comparing the arithmetic mean of inhibition zones between experimental solutions.