- D-Scholarship@Pitt
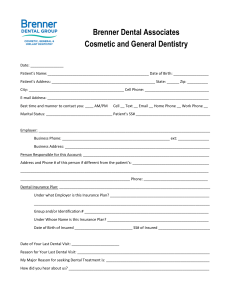
advertisement

A REVIEW OF SCHOOL-BASED DENTAL SEALANT PROGRAMS AND THE DEVEOPMENT OF A STATEWIDE SCHOOL-BASED DENTAL SEALANT PROGRAM MANUAL IN PENNSLVANIA by Kaitlyn Burgess BA, BS, University of Florida, 2011 Submitted to the Graduate Faculty of Graduate School of Public Health in partial fulfillment of the requirements for the degree of Master of Public Health University of Pittsburgh 2015 UNIVERSITY OF PITTSBURGH GRADUATE SCHOOL OF PUBLIC HEALTH This essay is submitted by Kaitlyn Burgess on April 20, 2015 and approved by Essay Advisor: David Finegold, MD Professor of Human Genetics Director, Multidisciplinary MPH Program Graduate School of Public Health University of Pittsburgh _________________________________ Essay Reader: Richard Rubin, DDS, MPH ________________________________ Assistant Professor School of Dental Medicine Liaison for Multidisciplinary MPH Program School of Dental Medicine University of Pittsburgh ii Copyright © by Kaitlyn Burgess 2015 iii David Finegold, MD A REVIEW OF SCHOOL-BASED DENTAL SEALANT PROGRAMS AND THE DEVEOPMENT OF A STATEWIDE SCHOOL-BASED DENTAL SEALANT PROGRAM MANUAL IN PENNSLVANIA Kaitlyn Burgess, MPH University of Pittsburgh, 2015 ABSTRACT Background: Dental caries is the single most common chronic childhood disease. There is a disproportionately high level of dental caries experience in children from low-income families. Dental sealants have been proven to be effective at preventing caries development. Access to care is an enormous obstacle preventing necessary dental treatment such as dental sealants in school-aged children; school-based dental sealant programs (SBSPs) have been shown to minimize barriers to dental care, increase sealant use and decrease caries incidence. Although Pennsylvania has indicated the need to create dental public health interventions, no such statewide program has been developed for a SBSP. Public Health Relevance: Due to the high prevalence of untreated dental decay in schoolaged children in Pennsylvania, a school-based sealant program is a feasible and needed way to increase sealant use and reduce dental caries incidence in children. This goal is in accordance with the benchmarks set out by Health People 2020. Proposed Intervention: This essay proposes developing a statewide school-based dental sealant program manual for use by counties across Pennsylvania. iv TABLE OF CONTENTS 1.0 INTRODUCTION ........................................................................................................ 1 2.0 PUBLIC HEALTH SIGNIFICANCE OF DENTAL CARIES IN SCHOOL-AGED CHILDREN ................................................................................................................................... 2 2.1 CAUSES AND EFFECTS OF DENTAL CARIES IN CHILDREN .............. 2 2.2 PREVENTION, TREATMENT AND COST OF DENTAL CARIES ........... 3 2.3 INTRODUCTION TO SBSPS ............................................................................ 5 2.4 NEEDS ASSESSMENT FOR A SBSP IN PENNSYLVANIA ........................ 5 3.0 DETAILED REVIEW OTEMPERATURES AT 1 HOUR OF LIFEF SBSPS ...... 7 3.1 REVIEW OF EXISTING SBSPS ....................................................................... 7 3.1.1 Literature Search of SBSPs ............................................................................ 7 3.1.2 Best Practice Examples of SBSPs ................................................................... 8 3.1.3 Existing SBSPs in Pennsylvania .................................................................... 11 3.2 AVAILABLE RESOURCES TO CREATE A STATEWIDE SBSP MANUAL ............................................................................................................................ 12 3.3 4.0 DISCUSSION AND APPLICATIONS FOR PENNSYLVANIA .................. 14 PROPOSAL FOR STATEWIDE SBSP MANUAL IN PENNSYLVANIA .......... 15 4.1 GOALS AND AIMS .......................................................................................... 15 4.2 MANUAL OUTLINE ........................................................................................ 15 v 4.2.1 Strategic Partners ......................................................................................... 15 4.2.2 Participants ................................................................................................... 16 4.2.3 Personnel ....................................................................................................... 17 4.2.4 Equipment and Supplies ................................................................................ 18 4.2.5 Timeline ......................................................................................................... 19 4.2.6 Forms............................................................................................................. 20 4.2.7 Evaluation ..................................................................................................... 20 4.3 5.0 DISCUSSION ..................................................................................................... 21 4.3.1 Intended Public Health Outcomes ................................................................. 21 4.3.2 Anticipated Obstacles .................................................................................... 21 4.3.3 Sustainability ................................................................................................. 22 4.3.4 Funding Sources ............................................................................................ 23 CONCLUSION ........................................................................................................... 23 BIBLIOGRAPHY ....................................................................................................................... 24 vi LIST OF TABLES Table 1. Pennsylvania Medical Assistance Dental Fee Schedule for Children Under 21 .............. 4 Table 2. Summary of Successful Statewide SBSPs ........................................................................ 9 Table 3. Tentative Program Timeline ........................................................................................... 19 vii 1.0 INTRODUCTION The public health significance of dental caries is well documented. Epidemiological studies show that caries can affect people of all ages, races, genders and socioeconomic statuses; however people of low SES are at a higher risk for developing dental caries1. Thus, interventions aimed at reducing dental caries in low SES populations are advantageous from a public health standpoint2. Reducing the prevalence of caries in a population is cost effective and reduces the risk of future dental disease. Caries is a preventable disease and its occurrence can be reduced through a variety of ways. Early intervention, increased public awareness, patient education, nutritional counseling, frequent dental screenings, use of fluoride and application of dental sealants can all help to prevent caries3. For children specifically, school-based interventions have been shown to be effective at reducing the burden of oral disease4. Many states have instituted school-based sealant programs (SBSPs) that have improved access to dental care and ultimately lead to the reduction of caries. The states that will be profiled in this essay are Arizona, Georgia, Illinois, Kansas, Maryland, Michigan, Minnesota, New Mexico, Nevada, Ohio, Oregon and Wisconsin4-16. Pennsylvania has a documented need for a statewide school-based sealant program, but no such program has yet been devised. This essay will propose to develop a statewide schoolbased dental sealant manual for use by counties across Pennsylvania. 1 2.0 PUBLIC HEALTH SIGNIFICANCE OF DENTAL CARIES IN SCHOOL-AGED CHILDREN This section of the essay will explore the causes, effects, prevention methods, treatment options and cost implications of dental caries. School-based dental sealant programs will be introduced and basic needs assessment for a statewide SBSP in Pennsylvania will be discussed. 2.1 CAUSES AND EFFECTS OF DENTAL CARIES IN CHILDREN Dental caries is a chronic, multifactorial disease that has many adverse consequences. Genetics, diet, oral hygiene habits, SES, oral microflora, health beliefs, education level and access to dental treatment all affect the development and progression of dental caries. In children, other important factors affecting caries development in permanent teeth include maternal oral health habits, maternal oral microflora, existence of early childhood caries, food security and parental income17. Children are susceptible to dental caries in both primary and permanent teeth, and those who have carious lesions in the primary teeth are more likely to develop carious lesions in the permanent teeth18. Caries can have numerous unfavorable consequences for children such as possible dental pain, negative experiences at the dental office, need for future dental treatment, 2 missed time from school for dental appointments, increased cost for dental care, and other psychosocial effects19. 2.2 PREVENTION, TREATMENT AND COST OF DENTAL CARIES As with most diseases, there are two primary avenues to address dental caries: prevention before the onset of caries or intervention after the initiation of caries. Prevention methods include nutritional counseling, oral hygiene instructions, regular dental visits, use of dental sealants, and application of fluoride dentifrices at home and at the dental office. Preventative interventions such as these have been shown to be effective at the population level to improve public health outcomes20. Once caries have begun to demineralize tooth structure to the point of surface cavitation, professional intervention is required. Prior to tooth surface cavitation, non-surgical methods such as application of fluoride, placement of a dental sealant over the incipient lesion, and diet modification can be effective at stopping the progression of caries21. At this stage, registered dental hygienists or dental assistants in many states can administer treatment and counseling. However, once the lesion has cavitated, surgical treatment is required. A licensed dentist must perform this treatment. Such treatment may initially include amalgam or composite restorations and could ultimately progress to involve endodontic and prosthodontic procedures if recurrent caries develops. Thus, there are different caries management pathways that dental providers should choose from in an attempt to preserve dental tissues22. Comparing a detailed cost effectiveness analysis of prevention strategies versus intervention strategies is multifaceted and beyond the scope of this essay. For simple comparison 3 purposes, the Pennsylvania medical assistance dental fee schedule for children under 21 (last updated Oct 13, 2014)23 is included in Table 1. Table 1. Pennsylvania Medical Assistance Dental Fee Schedule for Children under 2123 Procedure Code Terminology MA Fee D1351 Sealant- per tooth $25.00 D2140 Amalgam- one surface $45.00 D2391 Resin-based composite- one surface, posterior $50.00 D2751 Crown- porcelain fused to metal $500.00 D3330 Endodontic therapy- molar $500.00 In general, dental public health preventative methods have been proven to be cost effective24-26. One program rising in popularity is the non-operative caries treatment and prevention program (NOCTP). NOCTP is a conservative program that advocates the institution of preventative methods such as fluoride and sealants in high-risk populations due to their efficacy and cost-effectiveness27-28. In 2001, the National Institutes of Health released a consensus statement in support of early detection of incipient dental caries and subsequent nonsurgical treatment such as dental sealants29. Operative dentistry does not cure the disease of caries; it only treats the resulting lesion. Instituting preventative methods is highly encouraged because it helps to address the underlying causes of dental caries. Thus, treatment planning should include a focus on preventative measures30. The dental community has recently undergone a paradigm shift concerning dental treatment of pit and fissure carious lesions; 4 minimally invasive procedures are encouraged over surgical interventions from both a technical and financial standpoint31. 2.3 INTRODUCTION TO SBSPS Dental sealants have been show to reduce up to 81% of caries in sealed teeth as compared to non-sealed teeth after 2 years32. The Surgeon General and National Institute of Health advocate the use of school-based sealant programs to address oral health issues in America33. SBSPs have been show to be more cost effective than other universal, publically funded private practice models34. It has been estimated that instituting school sealant programs can more than double sealant prevalence in a given population35. The CDC along with the independent Task Force on Community Preventive Services recommended community water fluoridation and school sealant preventive programs as the most effective public health means to prevent tooth decay36-37. SBSPs are a proven and highly recommended strategy to prevent dental caries, particularly in low-income populations38-39. 2.4 NEEDS ASSESSMENT FOR A SBSP IN PENNSYLVANIA Healthy People 2020 outlined several measureable objectives in order to address the high rate of dental caries in children. A key goal is increasing access to dental care through implementing school-based dental sealant programs. Objectives concerning SBSPs are OH-9.1 “increase the proportion of school-based health centers with an oral health component that includes dental sealants from 24.1% to 26.5%”, OH-12.2: “increase the proportion of children 5 aged 6 to 9 years who have received dental sealants on one or more of their permanent first molar teeth from 25.5% to 28.1%”40. The Pennsylvania Department of Health created an Oral Health Program under Act 87 in 1996. The Oral Health Program advocates the creation of school linked sealant programs for low-income populations41. Additionally, the Pennsylvania Department of Health released an Oral Health Strategic Plan in 2002 that included the creation of school-linked sealant programs as a primary way to improve the state of oral health in Pennsylvania42. Although Pennsylvania has a demonstrated need to create dental public health interventions, no such program has been developed for a statewide SBSP. As of 2013, Pennsylvania was one of only seven states to have no report of a SBSP in practice 43. Additionally, the Pew Center on the States issued Pennsylvania a grade of “D” in terms of dental sealant utilization44. The most recent data from the CDC indicate that only 26.1% of third graders in Pennsylvania have dental sealants and that 27.3% of third graders have untreated dental decay45. There are over twenty school districts in Allegheny County alone with greater than 50% of students on free or reduced lunch, indicating there is substantial need for intervention in just the greater Pittsburgh area46. Developing a manual for a statewide SBSP in Pennsylvania is an appropriate and necessary step towards meeting the Healthy People 2020 goals to increase dental sealant utilization and reduce dental decay. 6 3.0 DETAILED REVIEW OF SBSPS As of 2013, there are 43 states reporting at least one existing SBSP44. The structure of SBSPs can vary widely based on funding, available dental providers, state government infrastructure, regional differences, economic climate, and many other factors. Some SBSPs have been in practice since the early 1970s and many have shown profound success47. This section of the essay will highlight some existing SBSPs and examine the available resources for creating a SBSP. 3.1 3.1.1 REVIEW OF EXISTING SBSPS Literature Search of SBSPs A PubMed search was conducted using the search query “school based sealant program in America” for articles published in English. The search yielded 22 results. Article topics varied widely and included issues such as improving access to care, cost-effectiveness of sealants, retention rates of sealants, change in academic performance among students receiving sealants, and utilizing mid-level providers to staff SBSPs. One article detailed the effectiveness of a New York State Department of Health SBSP; after five years the number of decayed, missing and filled surfaces was 6.8 in the control group and only 2.2 in the sealant group. Best results seen in the lowest income schools. The sealant group experienced a 44% net cost savings as compared to the control group48. Another article described a SBSP managed by a Boston dental school; through this intervention the Healthy People 2010 objective of 50% of all children aged 8 years to have at least 1 dental sealant was realized for study participants49. One study examined retention rates for sealants placed at a SBSP in Alabama and found that 71% of sealants were retained after 1.6 years. Children with sealants were also found to have significant 7 protection from occlusal decay50. Another article examined how the state of Texas was able to create a SBSP and serve over 28,300 students in the first year alone51. 3.1.2 Best Practice Examples of SBSPs Due to the varied nature of journal articles published on SBSPs, it is perhaps more pertinent to examine current best practice examples for SBSPs. The Association of State and Territorial Dental Directors (ASTDD) released a report profiling eleven successful SBSPs4. Similarly, the Children’s Dental Health Project (CDHP) also released a Sealant Report that included a description of five selected states with sustainable and substantial SBSPs5. After reviewing the ASTDD and CDHP documents, twelve states were selected to profile in depth in Table 2. The twelve states were selected based on the potential for the state’s SBSP to be modified and applied to Pennsylvania. Knowledge gleaned from studying these twelve programs combined and adapted to create a statewide SBSP manual that is customized for Pennsylvania. The successful programs that will aid in creation of a statewide SBSP for Pennsylvania shared many commonalities such as funding sources, school selection criteria, student selection criteria and resources utilized. Many successful programs used the Basic Screening Survey (BSS)52 for the initial dental exam and the Sealant Efficiency Assessment for Locals and States (SEALS)53 for data analysis. The most variable elements among different states were recruiting and funding of dental providers. Some programs contracted outside dental providers, others directly employed dental providers, and several provided grants to a third party to then hire dental providers at their discretion. Additionally, some states attempted to calibrate providers by instituting mandatory training modules while others had minimal standardization. details the similarities and differences between programs. 8 Table 2 Table 2 Summary of Successful Statewide SBSPs State Program AZ6 Est. 1987 GA7 Funding Admin Organization Arizona Dept of Health Services Office of Oral Health School Selection Georgia Oral Health Prevention Program (GOHPP) Illinois Department of Public Health (IDPH) Bureau of Oral Health >50% students on free/reduced lunch -CDC -CDC Cooperative Agreement -MCHBG -Delta Dental -HRSA -CDC -HRSA -MCHBG -AZ Medicaid -Private donors Est. 1984 -MCHBG -State general funds IL8 -MCHBG Est. 1985 KS9 Est. 2010 MD10 -HRSA -CDC -State grants -KS Medicaid -Delta Dental Foundation of Kansas Est. 2009 MI11 Est. 2007 MN12 Est. 2011 High proportion of students on free/reduced lunch program Student Selection Second and sixth grade students Dental Providers Resources Results Individually contracted and must complete training course -BSS In 2011-2012: -11,411 students screened -6,412 students received sealants -70% sealant retention rate Second grade students Dental sealant team employed by GOHPP -BSS -SEALS In 2011-2012: -71 schools visited -5337 screenings -7461 sealants >50% students on free/reduced lunch Second and sixth grade students Schools identified from online Screening Program “Smiles Across Kansas” as having unmet dental needs Not specified Individually contracted by applying for direct grant from IDPH Individually contracted and must complete calibration course -“Healthy Smiles” (oral health survey) -BSS -SEALs -“Smiles Across Kansas” (online screening program) Since inception: -72 counties served -1 million children screened -2 million sealants placed In 2011-2012: -46% of all KS public schools had participated with “Smiles Across Kansas” -355 schools visited -21,914 sealants placed -86.5% sealant retention rate Maryland Department of Health Office of Oral Health Known sealant rate, response rate free meal rate, caries rate Third grade students University of Maryland School of Dentistry students and faculty In 2009-2010: -Conducted state dental sealant demonstration project Michigan Department of Community Health >50% students on free/reduced lunch Third grade students Registered Dental Hygienists -Maryland public school children survey (oral health survey) -Released SBSP manual -SEALS Minnesota Department of Health (MDH) Oral Health Program >50% students on free/reduced lunch Not specified Individually contracted by applying for direct grant from MDH -BSS -SEALS -MN Oral health Statistics System -Released SBSP manual As of 2013: -64% of MN children estimated to have dental sealants -29% of high-risk schools in MN have SBSP 9 9 In 2012-2013: -138 schools visited -4724 students screened -16,731 sealants placed Table 2 continued: Summary of Successful Statewide SBSPs NM -State of New Mexico New Mexico Department of Health >50% students on free/reduced lunch Grades 1-3 in urban areas, Grades 1-6 in rural areas Dental Sealant Program State Staff -Oral Health America -HRSA -Private donors -NV Medicaid -MCHBG -HRSA Oral Health Workforce grant Future Smiles Southern Nevada Dental Hygiene Initiative Ohio Department of Health >50% students on free/reduced lunch Not specified Public Health Dental Hygienists; work on school premises or on mobile dental site -BSS -SEALS In 2012-2013: -3199 sealants placed -80% sealant retention rate -Improved academic performance High proportion of students on free/reduced lunch program Second and sixth graders -Released SBSP Manual -Funds 18 SBSPs across Ohio -State of Oregon Oregon Health Authority >50% students on free/reduced lunch First and second graders Grants awarded to local health departments, school systems, not-forprofit agencies and hospitals who hire dental staff Dental team employed by OHA -“Oregon Smile” (oral health survey) -SEALS In 2013-2014: -76.8% of eligible schools have active SBSP -7387 students screened -16,184 sealants placed -87% sealant retention rate -Wisconsin Department of Health Services -Delta Dental of Wisconsin Wisconsin Department of Health Services and Children’s Health Alliance of Wisconsin At the discretion of grant recipient At the discretion of grant recipient Grants awarded to local public health departments, community health centers, hospitals, school districts, dental schools and independent dentists -BSS -SEALs In 2012-2013: -60 counties served -42 SBSPs funded -33,000 children screened -92% sealant retention rate Est. 1978 NV13 Est. 2009 OH14 Est. 1984 OR15 Est. 2006 WI16 Est. 1999 In 2012-2013: -6254 students screened -19,075 sealants placed -85% sealant retention rate MCHBG: Maternal and Child Health Block Grant HRSA: Health Resources and Services Administration CDC: Centers for Disease Control and Prevention *Information in Table 2 was summarized from Association of State and Territorial Dental Directors Best Practices Report4, Children’s Dental Health Project (CDHP) Sealant Report5 and state specific administrative organization websites 6-16. 10 3.1.3 Existing SBSPs in Pennsylvania While Pennsylvania does not have a statewide SBSP, there are some existing SBSPs at the county level. Two such programs are in Allegheny County and Chester County. Allegheny County Health Department created a SBSP in 1996. From 1997-2000, the SBSP was in the pilot program phase and served 14 schools and 897 first grade students. Data analysis of the pilot program revealed that the program was successful and self-sustainable, so the program was expanded. Since its creation, over 60 elementary schools have been visited, 30,000 children have received oral health education, and 9,000 students have received dental sealants. The program consists of two parts: (1) oral health education to first and second grade students given by hygiene students from the University of Pittsburgh Dental Hygiene Program and (2) initial exam and sealant application done on-site at the qualified school by a dental team. The program has since been expanded to include fluoride varnish and now allows for the treatment of sixth grade students in addition to first grade students. Schools in Allegheny County are eligible to participate if at least 50% of students are on the free school lunch program54-56. Chester County Health Department also has an existing SBSP. In the fiscal year 2011/2012, 396 children aged 6-8 and 12-14 received dental sealants through the school program. The program is sponsored and funded by the PA Department of Health Oral Health Program. The program is run by the CCHD in partnership with the Coatesville Area School District57. A thorough dental sealant form was created for the program that includes information for parents about dental sealants and oral hygiene. Sealants and fluoride are applied at no cost to the parents. However, parents of students without insurance can be connected with resources such as medical assistance, CHIP and private insurers for other dental and medical issues58. 11 3.2 AVAILABLE RESOURCES TO CREATE A STATEWIDE SBSP MANUAL There are numerous resources available to aid in creating a statewide SBSP manual. Some of these resources are outlined below. Seal America: The Prevention Intervention59: The National Maternal and Child Oral Health Resource Center published an online guide to creating a school-based dental sealant program. This guide includes 10 key steps: (1) getting started, (2) gaining and maintaining community support (3) staffing (4) purchasing dental equipment and supplies (5) funding (6) developing forms and records, tracking students, and collecting and analyzing data (7) preparing to launch (8) implementing the program (9) referral and follow-up (10) program evaluation. The guide is very general and can be applied to SBSPs of any size and in any state. The CDC, ADA, CDHP and ASTDD all reference Seal America as a thorough, useful tool for the creation of SBSPs. Promoting Oral Health in Schools: A Resource Guide60: This comprehensive manual was also released by the National Maternal and Child Oral Health Resource Center; it outlines school-based interventions such as basic dental screenings, placing dental sealants, topical fluoride application, injury prevention and community education. There is also a comprehensive list of existing programs and resources concerning school programs. This resource provides an extensive summary and contact list for public health interventions across America. Ohio Department of Health SBSP Manual61: In this comprehensive manual, the Ohio Department of Health (ODH) describes all pertinent details to their successful SBSP programs. 12 Important issues such as regulatory compliance, clinical methods, Medicaid billing and collection, health professional enrollment and reporting are explained in detail. The manual is intended for agencies applying for a SBSP grant from the ODH. The information base is extensive and helps ODH SBSP grant recipients in Ohio to meet all requirements and expectations of the program. While targeted at providers and agencies within Ohio, the manual has a wealth of useful information about creating a comprehensive SBSP that can be used as a beginning template for other states to create their own SBSP manual. Ohio Dental Clinics Online Module62: As an adjunct to the SBSP Manual, the ODH released a mandatory online training module for all ODH SBSP grant recipients. The five-part module is targeted at calibrating SBSP staff to the basic procedures involved in sealant placement. The technical knowledge should be purely review for dental providers, but the modules allow for standardization and continuity within the program. Similar to the ODH SBSP Manual, this resource is aimed at ODH SBSP grant recipients, but can be generalized to providers in all states. The module was created by ODH in conjunction with the National Maternal and Child Oral Health Resource Center, the creators of Seal America. Minnesota Department of Health SBSP Manual63: This manual is published for programs interested in starting or standardizing SBSPs in Minnesota. This may include local public health departments, public schools, community health centers, safety net dental providers, dental schools and non-profit organizations. The manual is thorough and outlines how to create, execute, analyze and sustain a SBSP. Maryland Office of Oral Health Dental Sealant Guidelines and Operations Manual64: This manual analyzes the current state of SBSPs in Maryland and provides a framework to modify and standardize programs. The manual discusses all relevant information about SBSPs 13 including but not limited to protocols, community needs assessment, staffing, reports and site reviews. The manual also contains suggestions for health education programs, information about technical assistance, and offers flexible ideas for SBSPs such as mobile dental programs and hybrid programs. 3.3 DISCUSSION AND APPLICATIONS FOR PENNSYLVANIA The existing resources on creating statewide SBSPs have some variability, but there is also a significant amount of overlap of necessary information. Universal elements include creating a purpose statement, conducting a needs assessment, discussing strategic partners, securing adequate funding, identifying qualified schools, selecting patients, acquiring informed consent from parents, recruiting dental personnel, purchasing equipment, establishing technical protocols for sealant application, assuring regulatory compliance and infection control, creating a referral network for patients needing more advanced treatment, involving school personnel, filing insurance claims, conducting retention checks and/or quality assurance site visits, analyzing program data and discussing program sustainability. These elements must be incorporated into even the simplest SBSP to assure the proper standard of care is maintained. Creation of a statewide SBSP requires a thorough analysis of numerous economic, political, legal and environmental factors. There is a wealth of information available concerning SBSPs such as published case studies, best practice examples, and state specific SBSP manuals. Pennsylvania has no such state specific SBSP manual or guide published. Publishing a SBSP manual for Pennsylvania would help facilitate the implementation of SBSPs across the state by eliminating guesswork and streamlining the creation of local programs. 14 4.0 PROPOSAL FOR STATEWIDE SBSP MANUAL IN PENNSYLVANIA The following proposal is for the creation of a statewide SBSP manual in Pennsylvania. The program goals, program outline, strategic partners, program participants, program personnel, necessary supplies, program timeline, and program evaluation will be described. 4.1 GOALS AND AIMS Program manual design will be centered on best practice criteria for existing SBSPs. The primary goals will be to create a program with (1) demonstrated impact and effectiveness (2) maximum efficiency with both time and finances (3) sustainability (4) collaboration and integration with other existing SPSPs (5) adaptable objectives4. 4.2 MANUAL OUTLINE The outline for this manual is intended to serve as a framework for future SBSPs in Pennsylvania and can be adapted to meet the needs of many different populations. 4.2.1 Strategic Partners There are several important organizations that will be crucial to the development and execution of a functional statewide SBSP manual. The Allegheny County Health Department will be an important resource concerning state specific demographic information, integration 15 with existing school health programs, state funding opportunities and administrative experience. The Chester County Health Department will be similarly helpful by describing their existing SBSP, evaluating strengths and weaknesses and determining potential obstacles to expanding and integrating the program to other counties. The Pennsylvania Department of Health could provide important information about health departments across the state and give valuable administrative advice concerning public health programs. The Pennsylvania Dental Association could be helpful in identifying different possible dental providers. The officials at the school districts and elementary schools in Pennsylvania will be key to the implementation of SBSPs. The school officials will serve as an intermediary between SBSP program personnel and the parents of program participants, so qualifying schools must have administrative staff that is willing and able to support the SBSP. 4.2.2 Participants Elementary schools in Pennsylvania will be eligible to participate with the SBSP if greater than 50% of students are eligible for free or reduced lunch. This information can be found via the National health and Nutrition Examination Survey65 for each county in Pennsylvania. All students enrolled in the second grade at schools participating with the SBSP will be screened for dental sealants, regardless of insurance status. If funds and personnel are available, then students enrolled in the sixth grade can also be screened. Students with an established dental home will be encouraged to pursue treatment with their personal dentist in an effort to maintain professional decorum. 16 Inclusion criteria for sealant placement include fully erupted first permanent molars without caries or with incipient caries on second grade students and fully erupted second permanent molars without caries or with incipient caries on sixth grade students. Exclusion criteria for sealant placement includes non-erupted or partially erupted permanent molars or fully erupted permanent molars with cavitated lesions. 4.2.3 Personnel A program director for the statewide SBSP must be recruited and hired to organize and facilitate the administrative aspects of the pilot program. A program assistant would also be valuable for completing miscellaneous tasks. Staffing to provide the dental treatment at various schools can be secured in different ways. Dental personnel can be recruited through the Pennsylvania Dental Association, Pennsylvania Dental Hygienists’ Association and Public Health Council, Public Health Dental Hygiene Practitioners’ Association, Expanded Function Dental Assistants’ Association, local health departments, community health clinics, federally qualified health centers, dental schools, dental hygiene schools and private dental offices. A minimum of two providers should be present at each SBSP. These providers can be licensed dentists, public health dental hygiene practitioners (PHDHP), expanded function dental assistants (EFDA), dental hygienists, dental students and dental hygiene students. PHDHPs would be ideal providers since they can place dental sealants without direct supervision from a dentist66. EFDAs, dental hygienists, dental students and dental hygiene students all require direct supervision from a dentist in Pennsylvania67. In order to standardize the providers, all clinical program personnel will be required to complete the Ohio Dental Clinics Online Module62 prior to performing dental treatment. 17 4.2.4 Equipment and Supplies Equipment and supplies may be purchased by each individual health department or SBSP. Alternatively, equipment and supplies may be purchased by the Program Director and then loaned to health departments of SBSP. Final decisions on procuring equipment and supplies will depend heavily on funding. Start-up Costs: Starting a SBSP requires the purchase of portable dental equipment. This equipment includes a portable dental unit, air compressor, dental chair, dental light, dental hygienist stool, assistant stool, sterilizer, ultrasonic cleaner and dental tools. Seal America estimates that start-up costs for this equipment can range from $7,621.00 to $17,746.00 for the initial operatory. Each additional operatory can cost from $4,811.00 to $11,92059. Operating Costs: Other supplies will also be necessary such as gowns, masks, gloves, bibs, disposable plastic covers, air-and-water syringe tips, high-volume suction tips, low-volume suction tips, cotton rolls, dry angles, gauze, disposable bite blocks, incentives for students, toothbrushes, etch gel, prime and bond, resin-based sealant material, dental trays, antibacterial gel, sterilizer backs, sterilizer cleaner, surface disinfectant, ultrasonic cleaner solution, vacuum system cleaner, trash cans, trash can liners, light bulbs, first aid kit, electrical equipment, tool kit and general office supplies59. These costs will recur throughout the duration of the SBSP. Salary and Wages: Additional costs include a salary for the Program Director, hourly compensation for the Program Assistant, transportation to and from school sites, fee to access the Basic Screening Survey, cost of SEALS software, purchase of two laptops for Program Director and Program Assistant. Consultant fees may also be required for project design and/or data analysis. 18 4.2.5 Timeline Table 3: Tentative Program Timeline Prior to 1st visit to school Tentative Timeline 12 months prior 7-11 months prior Identify and hire program director Create appropriate forms to be distributed to parents, schools, and dental personnel Formalize agreement with dental providers Introduce program to school officials Secure additional project funding Purchase equipment and supplies 6 months prior Determine school’s eligibility (>50% free/reduced lunch) Contact school to determine interest level in SBSP 3 months prior Discuss details of program with school officials Establish date of 1st visit 2 months prior Distribute permission forms for students to give to parents Identify student’s insurance status (uninsured, Medicaid, private) 1 month prior 1st visit to school 1 month 2nd visit after initial to school school visit rd 3 visit 1 year after initial to school school visit Program analysis Description of Activities 12-18 months after initial school visit Collect permission forms from students Determine final estimate of student participants Order necessary dental materials Schedule dental personnel for school visits Initial exam using Basic Screening Survey Sealant placement Short-term retention check to verify sealant application was satisfactory Long-term retention check to verify sealants are still properly sealed Limited dental exam to check for development of caries on teeth where dental sealants were placed Data analysis using SEALS Create report on pilot program Evaluate successes and failures of pilot program Adapt and expand program where necessary 19 4.2.6 Forms There are several forms that are crucial to the SBSP: 1) Interest letter for qualified elementary schools 2) Informed consent letter to parents of second grade students 3) Information on dental sealants and SBSP for distribution to parents and teachers 4) Certification of completion of online training module for dental providers 5) Basic Screening Survey for initial dental exam 6) Reimbursement form for Medicaid, CHIP and private dental insurance 7) Referral form to UPSDM for more advanced dental treatment 4.2.7 Evaluation The CDC’s Sealant Efficiency Assessment for Locals and States (SEALS) will be used to evaluate program inputs, dental treatment administered, outputs and outcomes. Key indicators will be the number of students treated, prevalence of one or more dental sealants before and after pilot program, DMFS/DMFT scores of students before and after pilot program. Data will be used to determine if program goals and Healthy People 2020 goals were achieved. It will also serve to analyze the total costs of the program and ultimate treatment benefits. Information may then be submitted to the National Oral Health Surveillance System, if appropriate. If necessary, site visits could be helpful to evaluate the program, determine the level of standardization of dental providers and to assess quality control. 20 4.3 DISCUSSION 4.3.1 Intended Public Health Outcomes The intent of creating a statewide SBSP manual is to increase the number functioning SBSPs in Pennsylvania. A comprehensive manual will facilitate the creation of local programs and ensure standard of care is maintained. Each SBSP aims to increase the number of children in Pennsylvania with dental sealants, decrease the number of children with untreated dental decay, and improve access to dental care for children from low-income families by eliminating some barriers to care. Community preventative services such as SBSPs are an attempt to connect people with health care resources, particularly in at-risk populations. There are numerous potential benefits on the population and individual level. Effectively implemented SBSPs with the guidance of a statewide SBSP manual can ultimately be cost saving for government agencies. 4.3.2 Anticipated Obstacles Creating a statewide SBSP manual also comes with many potential obstacles. The first and largest obstacle is funding. The documented success of other statewide SBSP manual helps to justify the cost. Once the SBSP manual is created, disseminating that information could also be challenging. Sending the manual to all county health departments in Pennsylvania would be a good first step to raising awareness about the manual and for ultimately creating SBSPs. Other obstacles include challenges specific to SBSPs. One potential issue is recruiting elementary schools that are willing and able to support a SBSP. In an attempt to overcome this issue, interest letters will be sent to all qualified elementary schools. Officials that are motivated to respond to the inquiry are more likely to be helpful in facilitating the SBSP. Another documented issue is the return rate of consent forms from parents of qualified students. To 21 combat this issue, the Program Director can opt to hold an evening meeting for parents of students for the SBSP. However, parents that are not compliant in returning consent forms are unlikely to attend an evening meeting, so the effect may be minimal. Another potential obstacle will be recruiting dental providers. Targeting PHDHPs, EFDAs, and dental staff at health departments, community health clinics and federally qualified health centers may be a good starting point. In Pennsylvania, PHDHPs are the only mid-level dental provider that can apply dental sealants without direct supervision from a licensed dentist. Thus, PHDHPs are the ideal provider for SBSPs in Pennsylvania since they are able to work independently. Providing financial incentives may also help to attract providers if necessary. Further complications may arise from utilizing a large number of different dental providers to administer treatment. Thus, standardization through a free online training module56 will be required prior to administering treatment. There are many other potential issues that may arise throughout the planning and execution of the SBSP. The program director, health department, school district officials, elementary school administration and attending dentists should work together to resolve any obstacles affiliated with the SBSP. 4.3.3 Sustainability In order for a SBSP to be sustainable, one primary goal is to secure substantial funding. Billing Medicaid, CHIP and private insurance companies for services rendered will also be a necessity. Another critical goal is the establishment of a permanent position at a state agency for development of the program. The Pennsylvania Department of Health Oral Health Program could be approached about creating this position. 22 4.3.4 Funding Sources There is a wealth of potential funding for SBSPs. The first and most substantial is the Title V Maternal and Child Health Services Block Grant. This grant funds a majority of successful statewide SBSPs in excess of $300,000.00 annually, per state. Delta Dental has also provided grants for SBSPs in many different states. HRSA currently funds SBSPs through the Bureau of Health Profession’s State Oral Health Workforce Grants. The CDC sponsors StateBased Oral Disease Prevention Program grants for oral health community programs. Oral Health America’s National Sealant Alliance donates dental sealant materials to qualified SBSPs. Additionally, the Pennsylvania Department of Health Oral Health Program may allocate some funds for SBSPs. 5.0 CONCLUSION School based-sealant programs are an effective means of preventing dental caries in highrisk populations. There are many states with successful programs in place and a vast array of available resources for designing SBSPs. Pennsylvania would greatly benefit from the creation of a statewide SBSP manual. By developing a clear and useful manual, counties across Pennsylvania could begin to institute SBSPs and ultimately reduce the burden of oral disease for children in Pennsylvania. 23 BIBLIOGRAPHY 1. Costa SM, Martins CC, Bonfim Mde L, Zina LG, Paiva SM, Pordeus IA, Abreu MH. A systematic review of socioeconomic indicators and dental caries in adults. Int J Environ Res Public Health. 2012 Oct 10;9(10):3540-74. 2. Winter J, Glaser M, Heinzel-Gutenbrunner M, Pieper K. Association of caries increment in preschool children with nutritional and preventive variables. Clin Oral Investig. 2015 Feb 13. 3. Davies RM, Blinkhorn AS. Preventing Dental Caries: Part 1 the scientific rationale for preventive advice. Dent Update. 2013 Nov;40(9):719-20, 722, 724-6. Review. 4. Association of State and Territorial Dental Directors. Best Practice Approach Reports: School-Based Dental Sealant Programs. Jun 2003. Available at [http://www.astdd.org/bestpractices/bpar-sealants-update-08-20-2014.pdf]. Accessed 1 Nov 2014. 5. Children’s Dental Health Project. Dental Sealants: Proven to Prevent Tooth Decay. Washington, DC: Centers for Disease Control and Prevention. May 2014. 6. Arizona Department of Health Services Office of Oral Health. Arizona School-Based Sealant Program. 2009. Available at [http://www.azdhs.gov/phs/owch/oral-health/dentalprograms/sealant.htm]. Accessed 21 Feb 2015. 7. Georgia Oral Health Coalition. State Office Projects. 2015. Available at [http://www.gaohcoalition.org/projects/state-office.aspx]. Accessed 21 Feb 2015. 8. Illinois Department of Public Health. Dental Sealant Grant Program. 2015. Available at [http://www.idph.state.il.us/grant_rfps/FY12/DSGP_RFA_FY12.pdf]. Accessed 21 Feb 2015. 9. Kansas Department of Health and Environment. School Sealant Program. 2015. Available at [http://www.kdheks.gov/ohi/sealant_program.htm]. Accessed 21 Feb 2015. 10. Maryland Department of Health and Mental Hygiene’s Office of Oral Health. State Dental Sealant Demonstration Project. 2010. Available at 24 [http://phpa.dhmh.maryland.gov/oralhealth/docs1/MT_final_document_08022010.pdf]. Accessed 21 Feb 2015. 11. Michigan Department of Community Health. Seal! Michigan Program. 2014. Available at [http://www.michigan.gov/mdch/0,4612,7-132-2942_4911_4912_6226-279800-,00.html]. Accessed 21 Feb 2015. 12. Minneosta Department of Health. School-based Dental Sealant Program. Jan 2015. Available at [http://www.health.state.mn.us/oralhealth/sealant.html]. Accessed 21 Feb 2015. 13. Nevada State Health Division Bureau of Child, Family and Community Wellness. Sealant Plan. 2012. Available at [http://health.nv.gov/Cancer/2011SealantPlan.pdf]. Accessed 21 Feb 2015. 14. Ohio Department of Health. School-based Dental Sealant Program Grants. Feb 2015. Available at [http://www.odh.ohio.gov/odhprograms/ohs/oral/grantfunds/sbds.aspx]. Accessed 21 Feb 2015. 15. Oregon Health Authority. Oregon School-based Dental Sealant Program. 2014. Available at [https://public.health.oregon.gov/PreventionWellness/oralhealth/School/Pages/SchoolDe ntalSealantProgram.aspx]. Accessed 21 Feb 2015. 16. Children’s Health Alliance of Wisconsin. Oral Health: Wisconsin Seal-A-Smile Program. 2015. Available at [http://chawisconsin.org/oral-health.php?pg=31]. Accessed 21 Feb 2015. 17. Chi DL, Masterson EE, Carle AC, Mancl LA, Coldwell SE. Socioeconomic status, food security, and dental caries in US children: mediation analyses of data from the National Health and Nutrition Examination Survey, 2007-2008. Am J Public Health. 2014 May;104(5):860-4. 18. Masood M, Yusof N, Hassan MI, Jaafar N. Assessment of dental caries predictors in 6-yearold school children - results from 5-year retrospective cohort study. BMC Public Health. 2012 Nov 16;12:989. 19. Roberts MW. Dental health of children: where we are today and remaining challenges. J Clin Pediatr Dent. 2008 Spring;32(3):231-4. 20. Vermaire JH, van Loveren C, Brouwer WB, Krol M. Value for money: economic evaluation of two different caries prevention programmes compared with standard care in a randomized controlled trial. Caries Res. 2014;48(3):244-53. 21. Frencken JE, Peters MC, Manton DJ, Leal SC, Gordan VV, Eden E. Minimal intervention dentistry for managing dental caries - a review: report of a FDI task group. Int Dent J. 2012 Oct;62(5):223-43. 25 22. Ismail AI, Tellez M, Pitts NB, Ekstrand KR, Ricketts D, Longbottom C, Eggertsson H, Deery C, Fisher J, Young DA, Featherstone JD, Evans W, Zeller GG, Zero D, Martignon S, Fontana M, Zandona A. Caries management pathways preserve dental tissues and promote oral health. Community Dent Oral Epidemiol. 2013 Feb;41(1):e12-40. 23. Pennsylvania Department of Human Services. Medical assistance program dental fee schedule. 13 Oct 2014. Available at [http://www.dhs.state.pa.us/provider/doingbusinesswithdhs/dentalcareproviderinformatio n/index.htm]. Accessed 21 Feb 2014. 24. Mariño RJ, Khan AR, Morgan M. Systematic review of publications on economic evaluations of caries prevention programs. Caries Res. 2013;47(4):265-72 25. Neusser S, Krauth C, Hussein R, Bitzer EM. Clinical effectiveness and cost-effectiveness of fissure sealants in children and adolescents with a high caries risk. GMS Health Technol Assess. 2014 Oct 1;10:Doc02. 26. Goldman AS, Chen X, Fan M, Frencken JE. Methods and preliminary findings of a costeffectiveness study of glass-ionomer-based and composite resin sealant materials after 2 yr. Eur J Oral Sci. 2014 Jun;122(3):230-7. 27. Vermaire JH, van Loveren C, Brouwer WB, Krol M. Value for money: economic evaluation of two different caries prevention programmes compared with standard care in a randomized controlled trial. Caries Res. 2014;48(3):244-53. 28. Allen Y, Duane B. Risk-based caries prevention may be more effective in children. Evid Based Dent. 2014 Jun;15(2):41-2. 29. National Institutes of Health (U.S.). Diagnosis and management of dental caries throughout life. NIH Consens Statement. 2001 Mar 26-28;18(1):1-23. 30. Yip K, Smales R. Oral diagnosis and treatment planning: part 5. Preventive and treatment planning for dental caries. Br Dent J. 2012 Sep;213(5):211-20. 31. Schwendicke F, Jäger AM, Paris S, Hsu LY, Tu YK. Treating Pit-and-Fissure Caries: A Systematic Review and Network Meta-analysis. J Dent Res. 2015 Feb 20. 32. Ahovuo-Saloranta A, Forss H, Walsh T, Hiiri A, Nordblad A, Mäkelä M, Worthington HV. Sealants for preventing dental decay in the permanent teeth. Cochrane Database Syst Rev. 2013 Mar 28;3:CD001830. 33. Oral health in America: a report of the Surgeon General. J Calif Dent Assoc. 2000 Sep;28(9):685-95. 34. Bertrand E, Mallis M, Bui NM, Reinharz D. Cost-effectiveness simulation of a universal publicly funded sealants application program. J Public Health Dent. 2011 Winter;71(1):38-45. 26 35. Griffin SO, Jones KA, Lockwood S, Mosca NG, Honoré PA. Impact of increasing Medicaid dental reimbursement and implementing school sealant programs on sealant prevalence. J Public Health Manag Pract. 2007 Mar-Apr;13(2):202-6. 36. Gooch BF, Truman BI, Griffin SO, Kohn WG, Sulemana I, Gift HC, Horowitz AM, Evans CA Jr. A comparison of selected evidence reviews and recommendations on interventions to prevent dental caries, oral and pharyngeal cancers, and sports-related craniofacial injuries. Am J Prev Med. 2002 Jul;23(1 Suppl):55-80. 37. The Guide to Community Preventive Services. Preventing Dental Caries: School‐ Based Dental Sealant Delivery Programs. Accessed at: http://www.thecommunityguide.org/oral/schoolsealants.html. Last updated May 2014. 38. U.S. Department of Health and Human Services. A National Call to Action to Promote Oral Health. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institutes of Health, National Institute of Dental and Craniofacial Research. NIH Publication No. 03-5303, May 2003. 39. Muller-Bolla M, Lupi-Pégurier L, Bardakjian H, Velly AM. Effectiveness of school-based dental sealant programs among children from low-income backgrounds in France: a pragmatic randomized clinical trial. Community Dent Oral Epidemiol. 2013 Jun;41(3):232-41. 40. U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020. Washington, DC. Available at [http://www.healthypeople.gov/2020/topics-objectives/topic/oral-health]. Accessed 1 Nov 2014. 41. Pennsylvania Department of Health. Healthy Living: Oral Health. 2015. Available at [http://www.portal.state.pa.us/portal/server.pt/community/oral_health/14180]. Accessed 3 March 2015. 42. Pennsylvania Department of Health. Oral Health Strategic Plan for Pennsylvania. Nov 2002. Available at [http://www.dsf.health.state.pa.us/health/lib/health/oralhealth/FinalStrategicPlan.pdf]. Accessed 1 Nov 2014. 43. Centers for Disease Control and Prevention. States with Programs for Dental Sealants. 2 Apr 2010. Available at [http://apps.nccd.cdc.gov/synopses/ProgramDataV.asp?ProgramID=6]. Accessed 1 Nov 2014. 44. Pew Center on the States. Falling Short: Most States Lag on Dental Sealants. Jan 2013. Available at [http://www.pewtrusts.org/~/media/legacy/uploadedfiles/pcs_assets/2013/Pewdentalseala ntsreportpdf.pdf]]. Accessed 1 Nov 2014. 27 45. Centers for Disease Control and Prevention. State Oral Health Profile. 2009. Available at [http://apps.nccd.cdc.gov/nohss/bystate.asp?stateid=42]. Accessed 1 Nov 2014. 46. Pennsylvania Budget and Policy Center. Education Facts: Student Poverty Concentration. 2012. Available at [http://pennbpc.org/sites/pennbpc.org/files/School-Poverty-Data-bySchool-District.pdf]. Accessed 1 Nov 2014. 47. Children’s Dental Health Project. Dental Sealants: Proven to Prevent Tooth Decay. Washington, DC: Centers for Disease Control and Prevention. May 2014. 48. Zabos GP, Glied SA, Tobin JN, Amato E, Turgeon L, Mootabar RN, Nolon AK. Costeffectiveness analysis of a school-based dental sealant program for low-socioeconomicstatus children: a practice-based report. J Health Care Poor Underserved. 2002 Feb;13(1):38-48. 49. Devlin D, Henshaw M. Improving access to preventive dental services through a schoolbased dental sealant program. J Dent Hyg. 2011 Summer;85(3):211-9. 50. Dorantes C, Childers NK, Makhija SK, Elliott R, Chafin T, Dasanayake AP. Assessment of retention rates and clinical benefits of a community sealant program. Pediatr Dent. 2005 May-Jun;27(3):212-6. 51. Devine B. Reaching the Texas dental goals of healthy people 2010. Tex Dent J. 2011 Dec;128(12):1255-9. 52. Association of State and Territorial Dental Directors. Basic Screening Surveys. Available at [http://www.astdd.org/basic-screening-survey-tool/]. Accessed 1 Nov 2014. 53. Centers for Disease Control and Prevention. Sealant Efficiency Assessment for Locals and States (SEALS). 10 July 2013. Available at [http://www.cdc.gov/oralhealth/state_programs/infrastructure/seals.htm]. Accessed 1 Nov 2014. 54. Allegheny County Health Department. Dental Sealant Program. 2009. Available at [file:///C:/Users/kmb208.PITT/Downloads/Scan001.PDF]. Accessed 24 Mar 2015. 55. Allegheny County Health Department. Pediatric Dental Program. 2015. Available at [http://www.achd.net/dental/]. Accessed 24 Mar 2015. 56. Allegheny County Health Department. Dental Sealant Program. 2015. Available at [http://www.achd.net/dental/sealants1.html]. Accessed 24 Mar 2015. 57. Chester County Health Department. Dental Sealant Program. [http://chesco.org/index.aspx?NID=994]. Accessed 24 Mar 2015. 2015. Available at 58. Chester County Health Department. Dental Sealant Program Form. 2013. Available at [http://northbrandywine.net/upload/Nurse/dental_sealant_form.pdf]. Accessed 24 Mar 2015. 28 59. Carter NL, with the American Association for Community Dental Programs and the National Maternal and Child Oral Health Resource Center. 2011. Seal America: The Prevention Invention (2nd ed., rev.). Washington, DC: National Maternal and Child Oral Health Resource Center. 60. Bertness J, Holt K, eds. 2010. Dental Sealants: A Resource Guide (3rd ed.). Washington, DC: National Maternal and Child Oral Health Resource Center. 61. Ohio Department of Health Bureau of Community Health Services and Patient-Centered Primary Care. School-based Dental Sealant Program Manual. 2012. Available at [http://www.odh.ohio.gov/~/media/ODH/ASSETS/Files/ohs/oral%20health/Dental%20S ealant%20Manual%202012.ashx]. Accessed 1 Nov 2014. 62. Ohio Safety Net Dental Clinics. School-Based Dental Sealant Programs. 2009. Available at [http://ohiodentalclinics.com/curricula/sealant/index.html]. Accessed 1 Nov 2014. 63. Minnesota Department of health. Minnesota School-Based Dental Sealant Program Manual. 1 Jan 2013. Available at [http://www.health.state.mn.us/divs/hpcd/chp/oralhealth/pdfs/SealantProgramManual201 3.pdf]. Accessed 1 Nov 2014. 64. Maryland Department of Health and Mental Hygiene Office of Oral Health. Dental Sealant Guidelines and Operations Manual. 2012. Available at [http://phpa.dhmh.maryland.gov/oralhealth/docs1/Dental-Sealant-Guidelines-OperationsManual.pdf]. Accessed 1 Nov 2014. 65. Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. 20 Mar 2015. Available at [http://www.cdc.gov/nchs/nhanes.htm]. Accessed 24 Mar 2015. 66. The Pennsylvania Code. Practice as a Public Health Dental Hygiene Practitioner. Available at [http://www.pacode.com/secure/data/049/chapter33/s33.205b.html]. Accessed 24 Mar 2015. 67. Dental Assisting National Board, Inc. Pennsylvania State Requirements. 2015. Available at [http://www.danb.org/Meet-State-Requirements/State-SpecificInformation/Pennsylvania.aspx]. Accessed 24 Mar 2015. 29