BGA_-_For_Patients_files/Preparing for your Colonoscopy
advertisement
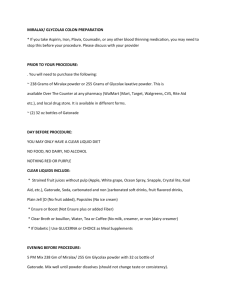
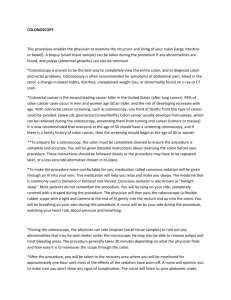
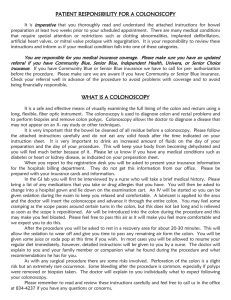
Preparing for your Colonoscopy HALFLYTELY ~ If you are on ASPIRIN, IRON, OR COUMADIN, OR OTHER BLOOD THINNERS you may need to STOP this 1 week before your procedure, or as otherwise directed by the provider. Please discuss with your provider ~If you take regular medications, please ask how to take them the day before your procedure and the day of your procedure. PLEASE FOLLOW THESE DIRECTIONS. DO NOT FOLLOW THE DIRECTIONS THAT COME WITH YOUR BOWEL PREP. THE DAY BEFORE YOUR PROCEDURE You will be on a CLEAR LIQUID diet all day. NO FOOD, NO DAIRY, NO ALCOHOL No Red or Purple CLEAR LIQUIDS INCLUDE: -Strained fruit juices without pulp (ex: apple, white grape, Ocean spray, Snapple, Crystal lite, Kool Aid, ect.) Water, Gatorade, carbonated and non-carbonated soft drinks, fruit flavored drinks, plain Jello (No fruit added), Ice popsicles (NO ice cream) - Ensure or Boost (NOT Ensure plus or with fiber) as meal supplements -Coffee or Tea (NO dairy, milk, non-dairy creamer) you can add sweeteners - Clear Broth or bouillon If Diabetic ] Use Glucerna or Choice as Meal Supplements Preparation of the Solution: Fill the container to the fill line with lukewarm water. Cover and shake to dissolve. All solutions are clear and colorless Please note that many patients prefer to drink the prep chilled but this can give you the chills. You can drink the prep at room temperature to avoid this. EVENING BEFORE PROCEDURE . 5 PM: Swallow 1 bisacodyl tablet with water (Do not chew or crush). . 7 PM: Start drinking your laxative solution (liquid). Drink one 8 oz glass every 10 minutes until the solution is gone. DRINK ALL THE SOLUTION BE NEAR A TOILET! You may experience bloating, some cramping, and definite diarrhea, loose and watery stools. This is normal and it may last for a few hours. * Please be aware that at some point during your prep you may become very nauseous, feel like you are going to vomit or even vomit. It is recommended that if this occurs or you feel very full, like you will vomit that you take a break from drinking the prep for 20 minutes to half an hour. Then resume the drinking of the prep again. If this happens again stop for 20 minutes to half an hour and then restart. DAY OF THE PROCEDURE . Do Not consume any food until after the procedure. . May drink a small quantity of water (up to 8 oz) prior to procedure unless you are also scheduled for an EGD. If you are scheduled for and EGD, Nothing by mouth 6 hours prior to procedure. Helpful Hints: You may find that it is helpful to use a hard candy between glasses of laxative prep. This can help get rid of the taste of the medication from your mouth. You may find that using a ginger hard candy is helpful as it also helps with nausea. Please feel free to use you favorite flavor hard candy as this can be very helpful!! Binghamton Gastroenterology Associates Call with any questions or concerns 607- 772 -0639 COLONOSCOPY This procedure enables the physician to examine the structure and lining of your colon (large intestine or bowel). A biopsy (small tissue sample) can be taken during the procedure if any abnormalities are found, and polyps (abnormal growths) can also be removed. *Colonoscopy is proven to be the best way to completely view the entire colon, and to diagnose colon and rectal problems. Colonoscopy is often recommended for symptoms of abdominal pain, blood in the stool, change in bowel habits, diarrhea, unexplained weight loss, or abnormality found on x-ray or CT scan. *Colorectal cancer is the second leading cancer killer in the United States (after lung cancer). 93% of colon cancer cases occur in men and women age 50 an older, and the risk of developing increases with age. With colorectal cancer screening, such as colonoscopy, one third of deaths from this type of cancer could be avoided. (www.cdc.gov/cancer/screenforlife) Colon cancer usually develops from polyps, which can be removed during the colonoscopy, preventing them from turning into cancer (tumors or masses). It is now recommended that everyone at the age of 50 should have a screening colonoscopy, and if there is a family history of colon cancer, then the screening should begin at the age of 40 or sooner. **To prepare for a colonoscopy, the colon must be completely cleaned to ensure the procedure is complete and accurate. You will be given detailed instructions about cleansing the colon before your procedure. These instructions should be followed closely or the procedure may have to be repeated later, or a less accurate alternative chosen in its place. *To make the procedure more comfortable for you, medication called conscious sedation will be given through an IV into your vein. This medication will help you relax and make you sleepy. The medicine that is commonly used is Demerol or fentanyl and Versed. Conscious sedation is also known as "twilight sleep". Most patients do not remember the procedure. You will be lying on your side, completely covered with a draped during the procedure. The physician will then pass the colonoscope (a flexible rubber scope with a light and camera at the end of it) gently into the rectum and up into the colon. You will be breathing on your own during this procedure. A nurse will be by your side during the procedure, watching your heart rate, blood pressure and breathing. *During the colonoscopy, the physician can take biopsies (small tissue samples) to rule out any abnormalities that may be seen better under the microscope. He may also be able to remove polyps and treat bleeding areas. The procedure generally takes 30 minutes depending on what the physician finds and how easy it is to maneuver the scope through the colon. *After the procedure, you will be taken to the recovery area where you will be monitored for approximately one hour until most of the effects of the sedation have worn off. A nurse will monitor you to make sure you don't show any signs of complication. The nurse will listen to your abdomen, make sure you can tolerate fluids, and pass gas before you are discharged from the hospital. You will be able to resume your usual diet and take your routine medication after the procedure, unless otherwise instructed by a physician. **Because of the sedation used during the procedure, it is illegal to drive home! YOU MUST MAKE ARRANGEMENTS FOR A RIDE. No driving or operating heavy machinery or equipment for 24 hours. *Complications are uncommon. Bleeding can occur at a biopsy site, or where a polyp was removed. It is usually minimal, and rarely requires follow up. Other potential risks include reaction to the conscious sedation, and perforation (a tear) through the colon wall that could require surgery. Irritation to the vein that medication is given is uncommon, but may cause a tender area or lump that may last several days. Warm, moist towels will help with this discomfort. You may have some feelings of fullness, bloating, or cramping after the procedure, because of air introduced into the colon during the examination. This discomfort should resolve after you pass gas. **Please contact your physician if you notice any signs of complications such as difficulty tolerating fluids, persistent nausea or vomiting, worsening chest pain, severe abdominal pain, fever or chills. *The physician can discuss the findings of the colonoscopy with who ever came with you, or he can write this down, as you may not remember the conversation directly after the procedure as a result of the sedation. Results from the laboratory take at least 2 weeks. The physician or his assistant will call you with these results, and discuss follow up treatment. A copy of the report and procedure will be sent to your primary care physician. **If you have any questions, or if you require additional information regarding your procedure please contact our office. Binghamton Gastroenterology 40 Mitchell Avenue, 3rd Floor Binghamton, NY 13903-1678 Phone: 607-772-0639 Fax: 607-722-4610