Gynecological Histor..
advertisement

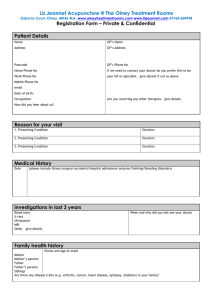
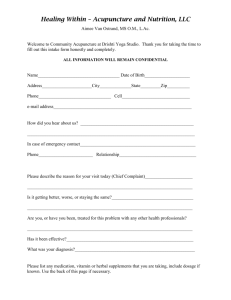
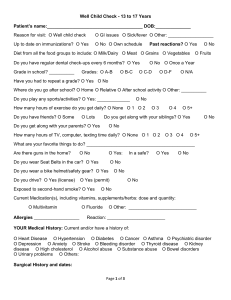
Gynecological History Taking Gynecological history taking involves a series of methodical questioning of a gynecological patient with the aim of developing a diagnosis or a differential diagnosis on which further management of the patient can be arranged. This further treatment may involve examination of the patient, further investigative testing or treatment of a diagnosed condition. There is a basic structure for all gynecological histories but this can differ slightly depending on the presenting complaint. When taking any history in medicine it is essential to understand what the presenting complaint means and what the possible causes (differential diagnosis) of the presenting complaint may be. After all, it is the aetiology of a symptom that guides the physician's questioning. Basic Structure of a Gynecological History Introduction Name of patient Age of patient Consent for questioning Presenting Complaint It is important to ask as open a question as possible in this part of the history and to ensure the complaint is understood as everything else follows on from here History of Presenting Complaint This will differ slightly depending on the presenting complaint but follows a vague structure: If pain is involved ascertain site, radiation (if any) and character Onset Periodicity Duration Recurrence? Aggravating & relieving factors Severity Menstrual History Menarche and menopause 1st day of last menstrual period Length of bleeding (days) Frequency Regularity Bleeding between periods Bleeding after intercourse Any post menopausal bleeding *Nature of periods Heavy? Clots? Flooding? Past Gynecological History Gynecological symptoms Gynecological diagnoses Gynecological surgery Date & result of cervical smears Contraception Past Obstetric History Gravidity and Parity Dates of deliveries Length of pregnancies Induction of labor/Spontaneous Normal Delivery? Weight of babies Sex of babies Complications before, during and after delivery Past Medical History Current or past illnesses Hospital admissions Past surgeries Drug History Prescribed medications Non-prescribed medications/herbal remedies Recreational drugs Any known drug allergies . Personal History Sleep *Appetite *Micturation *Defecation *Weight loss or gain *Addiction === Family History === Medical conditions Gynecological conditions Malignancies Consanguinity Social History Occupation Support network Smoking Alcohol marital status Ranking Diagnosis A differential diagnosis can be made after the history taking process. This is based upon a knowledge of the presenting complaints and the history of presenting complaints in relation to certain disease states. Although there is a general structure for history taking in gynecology, there are small differences in the approach depending on what the presenting complaint is. It is essential for a physician to know the causes of each symptom and the other manifestations of those causes before taking a history. Postcoital Bleeding This is bleeding after intercourse. Causes include: Cervical causes (common causes) Carcinoma Polyps Erosion Cervicitis Vaginal causes Vaginitis Carcinoma (very uncommon) Intermenstrual Bleeding This is vaginal bleeding between menstrual periods. Causes include: Cervical causes Carcinoma Ectropion Cervicitis Polyps Endometrial causes Carcinoma Polyps Endometritis Intrauterine Contraceptive Device Oral Contraceptive Pill or Contraceptive Injection Vaginal causes Atrophic vaginitis Infective vaginitis Carcinoma Ovarian causes Estrogen-secreting tumor Irregular Ovulation Fallopian tube causes Carcinoma Post-menopausal Bleeding This is vaginal bleeding more than 6 months after the menopause. Causes include: Vaginal causes Cervical causes Carcinoma Polyps Endometrial causes Atrophic endometritis Carcinoma Polyps Hyperplasia Ovarian causes Atrophic vaginitis Estrogen-secreting tumor Other causes Ring Pessary Exogenous estrogens (HRT) Menorrhagia This is history of heavy cyclical blood loss over several consecutive menstrual cycles in the absence of any intermenstrual or postcoital bleeding. Causes include: Pelvic pathology Uterine fibroids Endometriosis and adenomyosis Pelvic inflammatory disease Endometrial polyps Endocrine causes Dysfunctional uterine bleeding Hypothyroidism Haematological causes Disorders of coagulation Thrombocytopena Leukaemia Oligomenorrhea and Amenorrhea Oligomenorrhoea is infrequent menstruation defined by a cycle length between 6 weeks and 6 months. Amenorrhoea is absent menstruation for at least 6 months. They both have the same list for causes with one exception - primary failure of elements of the hypothalamic/pituitary/ovarian axis cause complete amenorrhoea, not oligomenorrhoea. Causes include: Endocrine Causes Hypothalamic disorders Kallman's syndrome - hypogonadotrophic hypogonadism Psychogenic - stress/shift work Exercise Excessive weight gain/loss Tumours e.g. craniopharyngioma Post-oral contraceptive use Pituitary lesions Pituitary adenomas Sheehan's syndrome - infarction necrosis Granulomatous infiltration e.g. sarcoidosis Ovarian lesions Turner's syndrome - ovarian dysgenesis Polycystic ovarian syndrome Resistant ovary syndrome Premature ovarian failure Androgen-secreting ovarian tumours Other Primary hypothyroidism/hyperthyroidism Poorly controlled diabetes mellitus Cushing's syndrome Addison's disease Dysmenorrhea This is painful menstruation which can be primary (absence of pelvic pathology) or secondary (attributed to pelvic pathology).Causes include: Endometriosis Pelvic inflammatory disease Submucosal fibroids Endometrial polyps Pelvic congestion syndrome Intrauterine contraceptive device Ovarian cysts Adenomyosis Dyspareunia in females This is pain during intercourse. Causes include: Superficial Infection Vaginal atrophy Inadequate episiotomy repair Vaginal/rectal tumor Deep Pelvic inflammatory disease Endometriosis Adenomyosis Cervicitis The Complete History For each of the most common and life-threatening conditions, it is important for physicians and medical students to know the important aspects that will present in the different parts of the history. It is this knowledge, that will guide the further management of the patient. Cervical Carcinoma Age: This condition usually affects women between the ages of 35-55. Screening in UK has noticed a trend towards a younger age group and the disease presenting itself in the 25-35 age group. Clinical Features Postcoital bleeding Intermenstrual bleeding Postmenopausal bleeding Risk Factors Early age of first experience of intercourse High number of sexual partners of patient or patient's current or past sexual partners HPV infection Smoking Low socioeconomic status Endometrial Carcinoma Age >40 years Clinical Features Post-menopausal bleeding Risk Factors Obesity Nulliparity Late Menopause Unopposed oestrogen stimulation Diabetes Mellitus Endometrial Fibroids/myomer Age Women of child-bearing age Clinical Features Menorrhagia Abdominal swelling Frequency of micturation Pain Infertility Recurrent abortions Risk Factors Pregnancy Family History Endometriosis Age Women of child-bearing age Clinical Features Cyclical Pelvic Pain Dysmenorrhoea Dyspareunia Infertility Pelvic Inflammatory Disease Clinical Features Bilateral lower abdominal pain Fever Vaginal discharge Deep dyspareunia Risk Factors Multiple sexual partners History of pregnancy termination Polycystic Ovary Syndrome Clinical Features Oligomenorrhoea Amenorrhoea Hirsutism Infertility Acne Obesity References McCarthy, A & Hunter, B (2003) Master Medicine: Obstetrics and Gynaecology (2nd ed.) Philadelphia: Elsevier Saunder