Pancreatic Cancer
advertisement

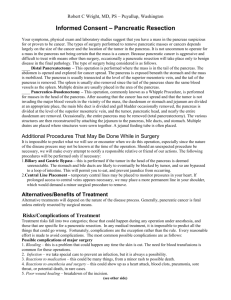
Pancreatic cancer Pancreatic cancer has one of the most serious outcomes of all cancers. It is the 5 th commonest cause of cancer death in Australia, similar to other countries despite its relative rarity. In Australia there were 2663 new cases of pancreatic cancer diagnosed in 2010, accounting for 2% of all cancer diagnoses. In 2011 pancreatic cancer contributed to 5% of all cancer deaths. Population based studies in the United States showed poor overall survival with 5 year survival rates of only 1.3% due in large part to the fact that only 10 – 20% of patients present with an early diagnosis allowing for curative treatment. Curability Once the diagnosis of pancreatic cancer has been made it is necessary to determine whether the tumour is removable by surgery and hence “resectable.” This means the tumour must be localised to the pancreas in order to be treated with curative intent. Operability or resectability is determined principally using computed tomography (CT) scanning with intravenous (IV) contrast. Current criteria for operability includes the absence of secondary disease to other organs, lack of involvement of major arteries and suitable segment of adjacent large veins (portal vein and superior mesenteric vein) to allow for venous reconstruction. Fitness for surgery In addition to operability determining a person’s fitness for surgery is vital for a favourable outcome. Both left and right sided pancreatic surgeries are major abdominal surgery. To be considered for pancreatic surgery a person needs to have a good performance status, adequate kidney and liver function, adequate blood parameters and a good cardiovascular system. Additional assessments of cardiac status including functional assessments are often indicated according to the individual person. Diabetes is commonly associated with pancreas cancer and good sugar control needs to be optimised prior to the surgical period. Jaundice Jaundice (a yellow tinge of the skin and conjunctiva) is a frequent presenting complaint for tumours on the right hand side (head) of the pancreas. Patients with jaundice have a number of changes that affect the kidney, liver, heart and immune system. There is considerable discussion regarding whether temporary relief of jaundice prior to major surgery is of benefit for an individual person and this would be discussed on an individual basis. Nutrition Nutritional assessment will be included in the pre-operative work up for someone being considered for pancreas surgery. Loss of appetite and weight loss are very common among patients with pancreas cancer. Weight loss of more than 10% of body weight or low blood protein levels are associated with an increased risk of complications. Surgical approaches Pancreaticoduodenectomy (Whipple procedure) This is the most commonly performed procedure for pancreatic cancer affecting the head or uncinate process of the pancreas (right sided lesions) the standard Whipple procedure includes removal of the head of the pancreas, the duodenum, the proximal small bowel (jejunum), the distal stomach, the gallbladder and the common bile duct as well as regional lymph nodes. Reconstruction of gastro-intestinal continuity requires joining the small bowel to the pancreas, the small bowel to the bile duct and the small bowel to the stomach. Of these the join between the small bowel and the pancreas (pancreaticojejunostomy) is the most prone to anastomotic leak leading to several technical modifications. Left sided or distal pancreatectomy Unfortunately less than 10% of pancreatic cancers on the left side of the pancreas are removable. For those that are confined to the pancreas a distal pancreatectomy involving removal of the left half of the pancreas along with removal of the spleen is the standard operation. Preservation of the spleen is not appropriate for cases of suspected pancreas cancer. Vascular resection Recent studies of pancreas surgery for pancreas cancer found that patients requiring removal of the portal or mesenteric vein did not have worse survival than those that did not require this extended surgery. Hence on an individual basis it may be appropriate to perform pancreas surgery in the context of involvement of the portal or mesenteric vein. This would be discussed on the individual basis. To date there is no clear evidence that removing major arteries for right sided pancreatic surgery will help a person’s survival. Such surgeries have increased risks of complications as well as perioperative death and are not recommended on a routine basis. Minimally invasive operations Laparoscopic distal pancreatectomy is a well-accepted alternative approach to open distal pancreatectomy in selected patients. The laparoscopic approach has slightly lower blood loss, shorter length of hospital stay and fewer post-operative complications compared with open surgery and may be appropriate for certain patients. Minimally invasive pancreaticoduodenectomy is not performed on a routine basis at the present time. Complications Both left and right sided pancreatic surgery are major operations that carry risk of post-operative complications and death. Complication (morbidity) rates following pancreatic surgery remain at 40 – 50%. The most frequent complication is a leak from the join between the pancreas and the small bowel, known as a pancreatic leak and this occurs in about 20% of patients. Bleeding following pancreatic surgery occurs in 5 – 6% of patients and delayed gastric function (delayed gastric emptying) can occur in around about 22% of patients also. Intra-abdominal abscess and biliary anastomotic leaks are less common complications. Survival The prognosis of patients with operable pancreatic cancer yields overall survival rates in the order of 20%. Post-operative chemotherapy with Gemcitabine or 5Fluorouracil have shown to improve survival. However more than 30% of patients are not fit for post-operative chemotherapy after pancreatic surgery. Hence there is a drive for pre-operative chemotherapy. In Australia we have recently demonstrated that pre-operative chemotherapy with Gemcitabine and Nab-Paclitaxel (Abraxane) can be safely delivered to patients with pancreatic cancer. Further studies will be undertaken to determine the operative timing and type of chemotherapy or chemoradiotherapy for pancreatic cancer in order to improve outcomes. Surgical Palliation A trial of surgery may be necessary in patients in whom there is uncertainty about resectability or operability. Patients’ tumours found not to be removable at surgery are candidates for palliative surgery. Palliative surgery for pancreatic cancer is directed at the relief of biliary (jaundice) and or gastro and duodenal (vomiting) obstruction, the relief of cancer related pain, and an improvement in a person’s quality of life. For most patients found to have inoperable pancreas cancer palliation can be achieved endoscopically with a stent being placed in the bile duct and or the duodenum to relieve biliary and duodenal obstruction respectively. These are robust procedures that occasionally require a second intervention. In individual person’s pancreas cancer is discussed carefully in a multidisciplinary fashion with our clinic and the treatment plan is tailored to the individual.