Chilton Cantelo School Medical Policy
advertisement

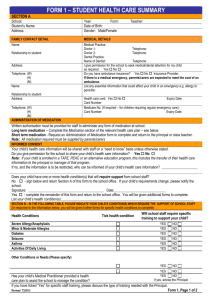
Chilton Cantelo School Medical Policy Introduction: Chilton Cantelo School (the School) is committed to encouraging and promoting good health and to dealing efficiently and effectively with illnesses and emergencies that may arise while children are in our care. This policy sets out the School’s commitment in respect of supporting pupils with their medical needs. The School implements appropriate policies for the care of day children and boarders who are unwell. These include: first aid, care of those with chronic conditions and disabilities, dealing with medical emergencies and the use of homely remedies. Reference should be made to the Medical Condition protocols and the attached Homely Remedies protocol. School Medical Officer: The School has nominated a School Medical Officer (SMO) to oversee the standards and deliverance of medical care. The day-to-day responsibility for the provision of this care is delegated by the SMO to the Headmistress and in turn to the staff in the Medical Room. The SMO is responsible for ensuring that policies and protocols for the deliverance of medical care are kept up-to-date in accordance with legal and legislative requirements and that they reflect best practice and cohesive working in the interests of all concerned. Assessing Medical Requirements: Medical Information Sheets (MIS), outlining significant past and current medical problems and treatment, known allergies and dates and details of all immunisations, are completed by parents or guardians of every child prior to their entry to the School. It is important that these details are received prior to a child’s start date, so that medical needs can be accurately assessed and contingencies put in place. These forms are reviewed by staff in the Medical Room, who takes the necessary steps to inform staff of any medical conditions or allergies of significance, including: asthma, eczema, travel sickness, hay fever and dietary allergies or needs. An Allergy & Medical Alert list together with a Severe Allergy / Medical Condition Alert showing a photographic representation of the child is published and posted at key points around the School. These include: the Medical Room, the Staff Room, the Kitchen, the Boarding Houses and each of the minibuses. If a child has a medical condition which the staff as a whole need to be aware of, this is also included on these lists and may be discussed in a wider staff forum. Confidentiality: Under the direction of the SMO discretion may be applied in order to strike a balance between the child’s right to privacy and confidentiality and the “need to know” requirement of School staff. In some cases it may be considered appropriate for a note to be sent to key personnel rather than a general notice. The SMO is consulted and has the final say on all matters of confidentiality and privacy and dictates the standards set across the School. Dietary Requirements: If a child has a specific dietary requirement, these needs are passed to the Head of Catering (Thomas Franks Ltd) who liaises with kitchen staff and the parents. Reviewed August 2015 To be reviewed August 2016 Page 1 Chilton Cantelo School Medical Policy Staffing / Training: The Medical Room is staffed from 8:15 to 5:45, Monday to Friday for all medical matters and during the evenings and at weekends House Parents are available in each of the Boarding Houses. All associated staff are suitably trained and all training is updated at least every 3 years. Staff in the Medical Room hold staff training records containing qualifications and renewal dates and the School office holds all information in the Central Register. Across the School there is always at least one suitably qualified person on site when children are present and in compliance with the Early Years’ Foundation Stage (EYFS) at least one suitably qualified person is present on EYFS outings. Access to Medical Care / First Aid: All age groups across the School have access to medical and first aid care throughout the day (and night for boarders). In addition, the School has an associated Registered GP and affiliated Practice in Sherborne, Dorset (Newlands Surgery). Boarding children are automatically registered at Newlands Surgery by the School and their parents may contact the Surgery directly at any time. The Registered GP (Dr Ruth Lawes) acts as the SMO and holds a clinic at the School for boarding children once a week, usually on Thursday. Children may request a Doctor of their own gender, if they prefer. At other times, children may be taken to the Newlands Surgery for appointments should the need arise and arrangements will be made by Medical Room staff. The SMO can be contacted at anytime throughout the week both by telephone and email for advice and guidance to staff and parents and is in regular contact with staff in the Medical Room. A child’s ability to consent to, or refuse medical or nursing treatment is acknowledged and their competency is based on awareness and skill, not on age. The confidentiality and rights of boarders as patients are appropriately respected, including the right to give or withhold consent for their own treatment. Likewise, boarders deemed sufficiently responsible to do so by the SMO are allowed to self medicate where appropriate. Other Healthcare Matters: Each new boarder is invited to undertake a School Medical during their first few weeks of term. For short term children (i.e. less than half a term) this is a chance for the SMO and staff in the Medical Room to meet them and ask general questions about their on-going health. For all other boarders a series of basic assessments will be made by the SMO, including heights, weights, a basic visual acuity test and a urine dip test. Children have access to a School Counsellor and a series of Independent Listeners and are all made aware of the arrangements to contact them. Sanatorium (“San”) Facilities: There are facilities available for the isolation of both boys and girls during periods of illness. A fixed call-bell system is in place to ensure that children are able to contact an appropriate adult at any time. If a child is admitted to the San: Parents and key members of staff, including Reception /admissions, will be contacted; Parents of day children will be asked to make arrangements to collect their child as soon as is practical within an appropriate time frame and Department of Health guidelines will be put in place for any necessary, ongoing exclusion period; Boarders will return to their houses overnight, if they are well enough to do so. Should a child require overnight care in the San, House Staff will make arrangements for an appropriate adult to remain with them or if their parent lives locally, they will be contacted and asked to collect their child. Reviewed August 2015 To be reviewed August 2016 Page 2 Chilton Cantelo School Medical Policy Medical Appointments: Children will be transported and escorted to/from the Surgery/Hospital by a suitable adult. If a child is under the age of 16, an appropriate member of staff (usually a member of staff from the Medical Room) will accompany them during their appointment. Records of all appointments and outcomes will be maintained in the child’s individual file held in the Medical Room and details will be passed to the parents as soon as is practical. . Over the Counter Medications (Homely Remedies): Parents/Guardians are made aware there is no contractual obligation for any member of staff trained in First Aid to administer medication and this is done on a purely voluntary basis. All staff follow the Homely Remedy protocol under guidance from the SMO when administering medication. Contained in the MIS for parents is the requirement to consent to the administration of Over the Counter medication (OTC) or “Homely Remedies”, such as paracetamol, should the need arise. If there is any question over consent, the child’s parents would be contacted before medication was administered. Children are not be dispensed any OTC medicine without prior parental permission and all medications administered are recorded. Any member of staff dispensing an OTC medicine must have knowledge of or refer to the appropriate home remedy protocol for guidance. Staff responsible for administering medication are required to undertake training and guidance and must sign their acceptance and understanding of these protocols. The Medical Room is equipped with a locked cupboard which contains OTC medications used for the comfort and well being of the children. Prescription medicines for children are kept separate and clearly labelled and only issued to the child for whom it was prescribed. Prescription Medication: All medication is passed to the staff in the Medical Room by the parent upon arrival at school and collected from the Medical Room when the child leaves at the end of the day. Medication for boarders’ is delivered to and collected from the Medical Room by House Staff. No medication is given by staff without the correct parental consents. All medication brought into School from home is: Contained in the pharmacist’s original container clearly labelled with the contents, child’s name, dosage and timing of administration, date of issue and expiry. Parents are asked to complete a Medication from Home, Parental Consent Form if their child requires medication during the school day. Without this form, medication will not be administered. Every child’s file contains a Medication Administration Record and if applicable a Prescribed Regular Medication Administration form to record medications given. A separate form is completed for each medicine or subsequent bout of illness. If a pupil requires medication on a school trip, the lead teacher on the trip will hold the medicine and administer as required and an individual risk assessment considering the child’s medical needs, medication requirements, physical needs, emergency treatment etc will be conducted by the member of staff in charge. Prescriptions for boarding children: Prescriptions for boarders are monitored by the SMO and staff in the Medical Room ensure that each child registered with a prescription has enough medication for both term-time and throughout the holiday periods. A list of those boarding children with prescription medication is kept in the Medical Room. Reviewed August 2015 To be reviewed August 2016 Page 3 Chilton Cantelo School Medical Policy Self-Medication (boarding children): With exception of the items listed below, all prescription medication is held securely in the Medical Room or Boarding House: 1. Children with Salbutamol inhalers are allowed to carry their clearly marked inhaler on their person for use in cases of exacerbation. The children, in particular the boarders, are encouraged to report to the Medical Room when they have self-administered their inhaler. 2. Girls prescribed the combined oral contraceptive, whether for menstrual control or contraception, are allowed to keep their pills securely in their boarding houses. 3. Other medication, topical and oral, deemed appropriate by the SMO may be kept by an individual and an authorisation to Self-Administer will be kept on file. 4. Separate arrangements are made on an individual basis for those children (day and boarding) who require the use of medications for a serious allergy or medical condition). Controlled medication: All controlled medication must be kept in a separate locked medication cupboard. This cupboard will only store controlled drugs and the controlled medication book. The medication book must be signed every time the controlled medication is administered. All controlled medication must be signed by both the person dispensing and the person administering the controlled medication. On weekdays the drugs will be dispensed by the medical room. On Saturday and Sunday, this responsibility lies with a named houseparent, who will ensure the medication and book is kept safe in a separate lockable cupboard within the boarding house. The controlled medication will be audited every Monday morning and Friday evening. As with all medication, the SMO will have to give consent that the medication can be administered to the child. In order for consent to be given, clear written instructions must be obtained from the student’s parent regarding dose and timing of administration. Staff personal medication: Any staff member bringing medication to school must leave it locked away in their bag in the staff room. (No child is allowed to enter the staff room unsupervised). The only exception to this would be an asthma inhaler which must be kept securely by the member of staff to whom it belongs. Inhalers: Inhalers: Boarders’ with asthma are required to have a spare ‘reliever’ which is clearly labelled with their name. These are kept in an unlocked drawer in the Medical Room for ease of access should the children need them during the day. Every child that has asthma has an Individual Care Plan (ICP). This is kept in their medical notes and is readily available if needed. The ICP is updated annually in consultation with the parents and SMO. Under new Government guidelines, the school is now legally able to hold a spare inhaler for use, through a spacer device by any child that may require such treatment. This inhaler can be used if a child has misplaced or has no access to their own inhaler. All children diagnosed with asthma will need parental consent to use the schools spare inhaler. All children with asthma will require an asthma card that states their asthma medication and the symptoms they experience as a result of their condition. All staff that have completed their three day first aid at work will be shown how to use the school inhaler and the spacer. Parents will be informed if the school inhaler has been used, and for the purposes of infection control, the spacer device will be sent home with any child that has required its use. Reviewed August 2015 To be reviewed August 2016 Page 4 Chilton Cantelo School Medical Policy EpiPens: Children who have been prescribed an Epipen for possible anaphylactic reactions are required to leave two Epipens in school. These are stored in clearly labelled “medical kits”; kept in the Medical Room. The medical kit contains the whole treatment required in the case of anaphylaxis. Children with severe allergies to wasp/bee stings are encouraged to wear their Epipens at all times. All children who have allergies requiring an EpiPen are required to have an ICP that is reviewed annually. The ICP is formulated with the parent (in consultation with the SMO) and a signature is obtained for consent to administer the Epipen in an emergency. A copy of the ICP is kept in their emergency medical kit, the staff room health notice board, and in the child’s medical file. School Medical Records Medical Information Sheets (MIS) are completed by Parents/Guardians prior to the child’s entry to the School. This information is kept in the Medical Room. Detailed Medical Records for each child are held in locked filing cabinets in the Medical Room. Medical records are ‘archived’ once a pupil has left the School and shredded after the statutory period has ended in accordance with the School’s data protection policy. Newland Surgery hold medical records of boarding pupils registered with them. Day Book. Staff maintain records of pupils visiting the Medical Room. Relevant information relating to boarding pupils is transferred into their ‘House’ books and a verbal hand-over between Medical Room staff and House Parents occurs twice daily, morning and night. Arrangements for pupils with particular medical conditions Photographs of children with severe allergies and medical conditions are distributed electronically to staff and a hard copy located in the Staff Room. Children with allergies and medical conditions are detailed on the Alert Lists which are taken on school trips, kept in First Aid Kits, stored on mini-buses and available in every Boarding House. Drug List. A list of all drugs on-site is kept in the Medical Room with indications for use, contra-indications, dosages and side effects. Accident Book any accident, incident, disease or dangerous occurrence arising out of or in connection with work is recorded and reported in accordance with guidance from the Health & Safety Executive (HSE). Accident records are passed to the Bursar. All visits to the Medical Room are recorded. The date, time, reason for visit and treatment/advice given are documented and signed by the member of staff treating the child. If treatment or medication is given information is passed to parents, where necessary, as soon as possible. The School Homely Remedy protocol sets out the SMO’s requirements for the administration of medication to children. Staff are trained and signatures kept of every person authorised to administer medication, to aid recognition at a later date. If medication of any kind is given to a child (day or boarder) a record is kept of: the name of medication, dosage, time and date given, reason for medicine and signature of staff member who administered medicine. Regularly required prescription medication, e.g. antibiotics, is documented on a medication chart which lists the same details as above. These sheets are also kept in the appropriate files. Confidentiality: Any child over the age of 16 is entitled to confidential medical assessment and treatment and except in case pertaining to a perceived Child Protection issue, this would be upheld. Children will always be encouraged to discuss their medical needs with their parents. Reviewed August 2015 To be reviewed August 2016 Page 5 Chilton Cantelo School Medical Policy Accidents /Incidents and Emergencies: In the event of an accident/incident or emergency during the school day, a nominated First Aider would be immediately informed; this would usually be a member of staff from the Medical Room. During the evenings and at weekends, a House Parent would be contacted. If the Medical Room is un-manned during the day, for any reason, a deputy First Aider would be appointed. Minor injuries and illnesses are treated in the Medical Room; Medical attention is sought in the event of serious injury at Accident & Emergency, Yeovil or Newland Surgery, Sherborne as appropriate; Major accidents / incidents are recorded in the ‘Accident Book’ which is held in the Medical Room. This includes: all accidents and incidents involving visitors to the site and members of staff employed by the School. Only accidents and incidents involving pupils at the School reportable under guidance from the Health & Safety Executive will be recorded and reported in the Accident Book; for other minor accidents and incidents the Individual File Sheets will suffice. Parents are informed of accidents and incidents involving their child as soon as practical. Calling an Ambulance: If in the judgement of the First Aider in attendance there is serious risk to the injured person and adequate care cannot be provided by personnel on site, the emergency services would be summoned immediately. Any member of staff or appropriate adult may make this decision once injury and risk has been assessed. Where injury to head, neck or back has occurred or significant broken bone is suspected, contacting the emergency services is a priority. Any injury requiring attendance by the emergency services is recorded in the Accident Book. Transfer to Hospital: Serious traumas/major head injuries necessitate hospital transfer via an ambulance; Parents would be informed of the child’s condition and exact location of transfer; A member of staff would accompany the child to A&E and parents of day children are asked to meet and relieve staff at the hospital; A staff member would contact the school as soon as a diagnosis has been established; ensuring parents and key staff are kept up-to-date. Illness: If a child is ill and unable to attend school, the parents are responsible for contacting the School Office. If a child becomes ill during the school day, the following procedure is followed: The child is taken to the Medical Room where staff will make the decision as to whether the child’s parents should be contacted to take the (day) child home. Whilst parents are being contacted, the child will be made as comfortable as possible in the San. If the child is removed from the school day, either to lie down or to go home, the staff in the Medical Room will inform the office and relevant members of faculty staff. Observations and treatment are documented every 30 to 60 minutes until the child is collected by the parents/guardians. Sick Boarders Accommodation for boarders who are unwell is adequately staffed by appropriately qualified personnel. It is separate from other accommodation and divided for male and female boarders as necessary. During nights and at weekends, parents of casual boarders would be contacted and treatment initiated, after permission is granted, while the child is waiting for collection. Reviewed August 2015 To be reviewed August 2016 Page 6 Chilton Cantelo School Medical Policy Parents/guardians of a boarding child are contacted if their child has been taken ill. In addition, if a boarder needs to see the GP, parents are informed of all developments. Parents who live locally (or within a reasonable distance from the School) will be asked them to collect their child to avoid contamination and the spread of germs. Infectious Illnesses: If a day child is suspected of having an infectious illness, under the Department of Health Guidelines and direction of the SMO, parents are contacted immediately and asked to take the child home for the specified exclusion period. If a boarder’s parents live within a reasonable distance, they are contacted as above. However, if they reside overseas, they would be isolated in the San until the infectious period is over or sent to their guardian depending on the seriousness and risk of further contamination to others. The final decision as to whether a child remains a risk to others will be taken by the Headmistress in consultation with the SMO. Extended Absence: Parents are contacted the day after a child has gone home due to accident or illness, in order to enquire as to the pupil’s condition and progress. Weekly updates will continue until the pupil returns to school and a record kept in the medical files. Hygiene/Infection Control: All staff follow basic hygiene procedures and take precautions to avoid infection. Staff have access to disposable gloves, masks, aprons and hand washing facilities. If it is suspected that contamination with blood/other bodily fluids has occurred they would take appropriate action. Bodily Fluid Kits are maintained and located at various points around the School and these are the responsibility of the Cleaning Supervisor. The School has a clear policy for the disposal of bodily fluids contained in the Medical Condition protocols at the end of this document. Medical Supplies: It is the responsibility of staff in the Medical Room to order medical and first aid supplies; checking, updating and replenishing as necessary. All ‘out-of-date’ medication is returned to Newlands Surgery and out-of-date supplies are disposed of appropriately. The School has a registered “sharps” and clinic waste disposal system in place through an approved company and this is coordinated by the Cleaning Supervisor. First Aid Kits: Basic First Aid kits are available in all key areas of the School including: the office, science laboratories, home technology kitchen, woodwork area, maintenance department, school transport, Prep and Pre-Prep departments. They are easily identifiable and are kept in clean dry areas. First Aid kits are checked termly (or more frequently if required) by Medical Room staff to ensure contents are in place, in date and undamaged. A record is kept in the Medical Room of all First Aid Kits, their contents, expiry dates, location and the name of the person who has checked them and when. First Aid kits contain, as a minimum: 20 adhesive plasters of assorted sizes; 2 triangular bandages; 6 adhesive dressings of assorted sizes; 10 safety pins; 4 sterile dressings; 4 pairs of disposable gloves; 2 sterile eye patch; 1 guidance card and contents list plus: scissors, tape, eye bath, saline pods and wipes. Reviewed August 2015 To be reviewed August 2016 Page 7 Chilton Cantelo School Medical Policy They may be tailored to an individual department, e.g. blue plasters for HT and eye wash stations in science and DT. If an item is used it is replaced as soon as possible once the emergency is over. All staff have a duty to return the First Aid Kit to the Medical Room as soon as practical to facilitate this process. Portable First Aid kits are made available upon request to members of staff who are required to work away from the normal workplace. Away Fixtures/Outings: Medical bags are available for staff to collect in the event of an “away” sporting fixture or outing. If an incident were to occur, medical treatment is sought from the visiting school or venue in the first instance. If accident or injury occurs, parents would be contacted and the child/ren taken to nearest Accident & Emergency Department by a member of staff; treatment and after-care would be followed up at school. Incidents would be reported and recorded by the accompanying member of staff for the medical files and an account given to Medical Room staff. The child’s parents should be contacted by the accompanying member of staff as soon as practical to inform them of the situation together with the Headmistress who would be informed immediately of any off-site incident. School Minibuses: All the School’s minibuses have a prominently marked First Aid box, Allergy/Medical Alert and Severe Allergy/Medical Condition Alert List, readily available for use and maintained in a good condition. The First Aid box is stocked in accordance with Part II of Schedule 7 of the Road Vehicles (Construction and Use) Regulations 1986. List of qualified First Aid personnel: The main duties of First Aiders are to give immediate First Aid to pupils, staff or visitors when needed and to ensure that professional medical help is called upon when necessary. Staff in the Medical Room ensure that qualifications of First Aiders are appropriate and kept up-to-date through liaison with the Bursar. First Aiders will undergo training at least every three years and a list of qualified First Aid Personnel is kept in the Medical Room. Reporting to the Health and Safety Executive (HSE): (Incident reporting in schools (accidents, disease and dangerous occurrences) – Guidance for employers – HSE Information Sheet) The School has a legal duty under the Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 1995 (RIDDOR) to report and record major work-related accidents; including dangerous occurrences, to the HSE, Incident Contact Centre (ICC): 0845 300 99 23. Injuries to pupils who are involved in an accident at school or on an activity organised by the school are only reportable under RIDDOR if the accident results in: the death of the person and arose out of or in connection with a work related activity; or an injury that arose out of or in connection with a work activity and the pupil is taken directly from the scene of the accident to hospital for treatment (examination and diagnostic tests do not constitute treatment). If a pupil injured in an incident remains at school, is taken home or is simply absent from school for a number of days, the incident is not reportable. Not all sports injuries to pupils are reportable under RIDDOR, as organised sports activities can lead to sports injuries that are not connected with how schools manage the risks from the activity. The essential test is whether the accident was caused by the condition, design or maintenance of Reviewed August 2015 To be reviewed August 2016 Page 8 Chilton Cantelo School Medical Policy the premises or equipment, or because of inadequate arrangements for supervision of an activity. If an accident that results in an injury arises because of the normal rough and tumble of a game, the accident and resulting injury would not be reportable. Most playground accidents due to collisions, slips, trips and falls are not normally reportable. Incidents are only reportable where the injury results in a pupil either being killed or taken directly to hospital for treatment. Either is only reportable if they were caused by an accident that happened from or in connection with a work activity: the condition of the premises or equipment was poor, e.g. badly maintained play equipment; or the school has not provided adequate supervision e.g. where particular risks were identified, but no action was taken to provide suitable supervision. Reportable injuries from or in connection with a work activity include: o Fractures, other than to fingers, thumbs and toes; o Amputations; o Any injury likely to lead to permanent loss of sight or reduction in sight; o Any crush injury to the head or torso causing damage to teh brain or internal organs; o Serious burns (including scalding) which cover more than 10% of the body or cause significant damage to the eyes, respiratory system or other vital organs; o Any scalping requiring hospital treatment; o Any loss of consciousness caused by head injury or asphyxia. If a child went missing and subsequently sustains an injury, this would be considered a Child Protection issue and the reporting procedure and follow up would be carried out by the nominated officer in line with the School’s Safeguarding practice. Reviewed August 2015 To be reviewed August 2016 Page 9 Chilton Cantelo School Medical Policy ILLNESSES THAT REQUIRE SPECIAL CARE EPILEPSY o o o o o Keep calm. Continually reassure the patient. Protect the person from injury (removing harmful objects nearby). Safeguard airway but do not restrain the patient in any way. If possible place in recovery position as soon as is possible Seek medical assistance but DO NOT LEAVE PATIENT UNATTENDED! Signs & Symptoms 1. 2. 3. 4. 5. Loss of consciousness, body stiffens and falls to the floor. Jerking movements Blue tinge around mouth area. Loss of bladder and/or bowel control may occur. After a minute or so the jerking movements decrease and slowly consciousness returns. ANAPHYLACTIC SHOCK A moderate to severe allergic raction USE OF EPI-PEN THE CHILD MAY COMPLAIN OF : A red rash Feeling hot & flushed Raising anxiety Weakness & giddiness Difficulty in breathing May collapse High voice Feeling floppy Swelling of throat & tongue Difficulty in swallowing Increased heart rate IF THIS OCCURS, EXPLAIN TO THE CHILD THAT A REACTION IS OCCURRING AND YOU CAN TREAT IT. IMMEDIATE TREATMENT REQUIRED. ► Lay the child down flat with feet slightly raised, or if conscious and breathing problems, sit child on floor. ► Read instructions on Epi-Pen carefully – you have time to do this. ► Give adrenaline via the Epi-Pen into outer thigh. Can be given through clothes (not jeans or thick material) ► Call for an ambulance by dialling 999 or 112 and explain that the patient has had an anaphylactic shock. ► Stay with the patient and reassure them. ► Give used Epi-Pen to ambulance crew. ► Inform parents. ► Make a record of medication and time given. Reviewed August 2015 To be reviewed August 2016 Page 10 Chilton Cantelo School Medical Policy SCHOOL STAFF SHOULD PREVIOUSLY HAVE DISCUSSED WITH PARENTS THE USUAL SYMPTOMS EXPERIENCED BY THEIR CHILD. DIABETES – HYPOS DIABETES – MANAGING HYPOS A ‘hypo’ is when the blood glucose level falls below normal. HYPOS MAY OCCUR BECAUSE OF TOO LITTLE FOOD, EXTRA ACTIVITY OR TOO MUCH INSULIN A child with diabetes will usually recognise their own early warning signs, which will vary from person to person, but may include: HUNGER SWEATING DROWSINESS PALLOR SHAKING LACK OF CONCENTRATION ODD BEHAVIOUR Fast-acting sugar should be taken immediately, and should be readily available at all times – example are : SUGARY DRINK (NOT DIET) GLUCOSE TABLETS (X3) MINI CHOCOLATE BAR FRESH FRUIT JUICE HYPO STOP If no better in 5 minutes – take some more. Hypos should never be ignored – if in doubt, give some sugar, it is better to err on the side of caution. Never allow the student to leave the classroom alone for help, symptoms may develop rapidly. You may need to be quite insistent to make sure sugar is taken if the student is trying to refuse your help. When feeling better, a meal or snack should be eaten to prevent the glucose level from falling again. Some people may feel nauseous, tired or have a headache after a hypo and need some quiet time to recover fully. IF THE HYPO IS SEVERE AND THE CHILD IS UNCONSCIOUS (OR UNABLE TO SWALLOW) PLACE THEM IN THE RECOVERY POSITION AND CALL FOR AN AMBULANCE. THEY SHOULD NOT COME TO ANY IMMEDIATE HARM Reviewed August 2015 To be reviewed August 2016 Page 11 Chilton Cantelo School Medical Policy ASTHMA COMMON SIGNS OF AN ASTHMA ATTACK COUGHING SHORTNESS OF BREATH WHEEZING FEELING TIGHT IN THE CHEST BEING UNUSUALLY QUIET DIFFICULTY SPEAKING IN FULL SENTENCES TUMMY ACHE (SOMETIMES IN YOUNGER CHILDREN) What to do Keep calm Encourage the child or young person to sit up and slightly forward - do not hug or lie them down. Make sure the child or young person takes two puffs of reliever (blue) inhaler immediately (preferably through a spacer) Loosen tight clothing Reassure the child If there is no immediate improvement Continue to make sure the child takes one puff of reliever inhaler every minute for five minutes or until their symptoms improve. Call 999 or a doctor urgently if: The child or young person’s symptoms do not improve in 5-10 minutes The child or young person is too breathless or exhausted to talk The child or young person’s lips are blue Or if you are in doubt Continue to give the child one puff of their reliever inhaler every minute until the ambulance or doctor arrives. After a minor asthma attack Minor attacks should not interrupt the involvement of a pupil with asthma in school When the pupil feels better they can return to school activities. The parents/carers must always be told if their child has had an asthma attack. Important things to remember in an asthma attack Never leave a pupil having an asthma attack. If the pupil does not have their inhaler and/or spacer with them, send another teacher or pupil to get their spare inhaler (if one is held in the Medical Room). In an emergency situation school staff are required under common law, duty of care, to act like any reasonably prudent parent. Reliever medicine is very safe. During an asthma attack do not worry about a pupil overdosing. Send another pupil to get the Nurse if an ambulance needs to be called. Contact the pupil’s parents or carers immediately after calling the ambulance/doctor. Generally staff should not take pupils to hospital in their own car. However in some situations it may be the best course of action. Another adult should always accompany anyone driving a pupil having an asthma attack to emergency services Reviewed August 2015 To be reviewed August 2016 Page 12 Chilton Cantelo School Medical Policy Appendix A Diarrhoea/Vomiting Management Policy Aims & Objectives To assess and safely manage a child with diarrhoea and/or vomiting; preventing dehydration in the ill child and containing a possible infection, avoiding the spread of disease and ruling out other symptoms that could be attributed to Meningitis. Gastroenteritis virus, food poisoning, side effects of medications. Causes Assess Diarrhoea could also be caused by constipation and is a common early sign of meningococcal meningitis or septicaemia – See Appendix C. * * * * * duration: severity: blood present: fever: dehydration: preceding constipation? number of episodes in last 24hr (red or black) in motion/vomit treat if present dry tongue/mouth, skin not re-shaping after soft pinch, dry eyes: no tears, not reflecting light. * * * * adequate urine output contact with similar symptoms suspect meals new medication (antibiotics/NSAID) Small, frequent sips of clear fluids for up to 12 hrs; squash, water, dioralyte. Flat cold cola is good for vomiting children. Instruct child to always wash hands after using toilet. Actions to take After 6-12hrs, progress to high calorie, low fibre, milk-free diet: jelly, clear soup, bread & spread, rice, potatoes. To remain off school for 48hrs after last episode. Medication Can use paracetamol for stomach cramps - recommended liquid paracetamol. Refer to GP * * * * * Notification If food poisoning strongly suspected, notify Public Health Department with details. Department of Health Exclusion from School for 48 hours immediately following the last episode of vomiting or diarrhoea. If blood (red or black) is present in stools, or (red or brown) in vomit. If severe diarrhoea and general malaise. If severely ill/dehydrated. If symptoms are side effects of a medication which needs to be changing. If child has diabetes, diverticular disease, ulcerative colitis or Crohn’s Disease. Reviewed August 2015 To be reviewed August 2016 Page 13 Chilton Cantelo School Medical Policy Appendix B Fever Management Policy Aims & Objectives To strive to maintain child’s body temperature within normal limits while they are unwell, keeping the child comfortable and hydrated whilst preventing adverse reactions of high fever i.e. convulsions, heart murmur and ruling out other symptoms that could be attributed to meningitis. Infection: bacterial or viral, including upper respiratory infection, ear infection, urinary tract infection and appendicitis. Causes Most serious cause: meningitis or septicaemia. See Appendix C. * Tympanic thermometer (Temp > 37C = fever). * Other symptoms: sore throat/cold, swollen glands in neck, cough, vomiting/diarrhoea, painful or frequent urination. Assess * Look for symptoms of Meningitis: rash, photophobia, neck stiffness, lethargy or drowsiness. Dress lightly, encourage the child to drink water or squash and eat small/frequent meals as regularly as tolerable. Actions to take Isolate the child in separate room and check and document temperature at least every 4-6 hours. The child should remain off school until a normal temperature is maintained without medication for 24hrs and is eating normally. Once the return to school, the child should stay off games for 2-3 days. Medication Paracetamol (syrup or tablets). Give maximum single dose based on child’s age and do not give over maximum dose in 24hrs. Re-medicate every 4-6 hrs as required. Refer to GP * If the fever persists for more than 48 hours, in spite of regular medication. * If the child has a persistent or productive cough with coloured sputum or appears very unwell * If the child has any symptoms of Meningitis: lethargy, photophobia, stiff neck, rash, nausea/vomiting, headache. Notification Notify the Department of Health if Meningitis is diagnosed. Reviewed August 2015 To be reviewed August 2016 Page 14 Chilton Cantelo School Medical Policy Appendix C Meningitis and Septicaemia Meningitis is swelling of the lining around the brain and spinal cord caused by an infection. Septicaemia is blood poisoning caused by the same germs. Meningitis and septicaemia can be hard to recognise at first and can occur together or separately; they are very dangerous and can kill in hours. People who are faced with meningitis and septicaemia have to act fast to save a life. Symptoms may appear in any order, but the first symptoms are usually fever, vomiting, headache and feeling unwell, just like in many mild illnesses. Not everyone will get all of the symptoms and some do not usually present themselves or are more difficult to detect in young children e.g. stiff neck and dislike of bright lights The 'red flag' symptoms are often the first indicators and with Septicaemia will appear earlier than those for meningitis such as neck stiffness and dislike of light, and before the more serious symptoms The darker pictures indicate serious symptoms Septicaemia Meningitis Fever/vomiting Fever/vomiting Limb / joint / muscle pain Severe headache Cold hands and feet / shivering Stiff neck Pale or mottled skin Dislike of bright lights Breathing fast / breathless Sleepy, vacant, difficult to wake Rash which does not disappear when pressed with a clear glass Confused / delirious Sleepy, vacant, difficult to wake Rash which does not disappear when pressed with a clear glass (Less common in young children) (Less common in young children) (Not present in all cases) Confused / delirious Seizures In all cases of suspected meningitis and septicaemia contacting the emergency services must be a priority before contacting parents. Reviewed August 2015 To be reviewed August 2016 Page 15 Chilton Cantelo School Medical Policy Appendix D Convulsions Management Policy Aims & Objectives To protect a child from harm while fitting and assess and manage their airway, breathing and circulation after the fit. Epilepsy - unusual neurological patterns in the brain. Some epileptics experience auras before a fit; a certain smell, taste or visual signals. * Causes Very high fevers in young children – Febrile Convulsions. * Signs of a convulsion: violent muscle twitching, breath-holding, drooling at the mouth, loss of or impaired consciousness. * Once fitting stops, the muscles will relax and child will slowly regain consciousness, but may be very drowsy. * Common for vomiting to follow. Ensure child is lying in the Recovery position. Assess Protect child from injury: clear away nearby objects, surround the child with soft padding, including under their head if possible and loosen tight clothing around neck to help breathing. Actions to take Do not use force to restrain the child. Note the time and duration of fit. After fitting ceases, place child in recovery position and monitor airway and breathing and until fully recovered. Medication None. Do not attempt to give anything to drink until fully conscious and speaking. Medical assistance Dial 999 for an ambulance if the pupil is unconscious for more than 10 minutes, is having repeated fits or it is his/her first fit. State: “Convulsions - Child”. Notification Contact parents as soon as possible (after the emergency services) to collect the child once they have recovered. A child must not remain at School once an episode has occurred. Additional Children registered as Epileptic will have an Individual Care Plan (ICP) detailing causes and actions and will appear on the Medical Conditions List. Reviewed August 2015 To be reviewed August 2016 Page 16 Chilton Cantelo School Medical Policy Appendix E Asthma Management Policy Aims & Objectives To restore child’s airway during an asthma attack. Causes Asthmatic children can suffer an attack due to the common cold, chest infections exposure to allergens like dust, pollen or food or exercising in cold air and anxiety. Assess * Symptoms include: Cough, wheezing, shortness of breath or tightness in the chest. * Severe attack symptoms may also include: difficulty and noisy breathing, difficulty speaking, grey-blue skin, blue lips and tongue, drowsiness. Help the child into a comfortable position to assist breathing: usually sitting slightly forward is best. Tell them to try to take slow, deep breaths. Send someone for help – DO NOT leave the child. Assist the child to take two puffs of their inhaler (if available make sure they use the “spacer” – or send someone to get one from the Medical Room). They can breathe shallowly at first and then take deeper breaths while their mouth is attached firmly to spacer device. If it is a mild attack, and pupil able to take fairly deep breaths, the spacer device is not required. Repeat TWO puffs, EVERY minute, for UP TO 5 minutes (10 puffs) if necessary. Actions to take Once the attack eases usually within 5 minutes, encourage the pupil to take another TWO puffs from their inhaler and rest in sitting position until feeling comfortable. If after 5 minutes/10puffs of reliever inhaler there is no improvement, call for an ambulance: 999. State “Asthma Attack - Child” Repeat TWO puffs every minute, making a note of the number of puffs they are taking. If the child falls unconscious, check breathing and pulse prepare to resuscitate. Medication All asthmatics should carry their own prescribed medication on them. Refer to GP If an asthma attack occurs, with or without ambulance assistance, the child will need to have a medications review. Notification Contact parents. The child will need to be collected to go home and rest or visit the GP. In cases requiring hospitalisation parents should be contacted AFTER the emergency services. Additional Children registered as Asthmatic will have a dedicated Individual Care Plan (ICP) detailing causes and actions and will appear on the Medical Conditions List. Reviewed August 2015 To be reviewed August 2016 Page 17 Chilton Cantelo School Medical Policy Appendix F Fainting Management Policy Aims & Objectives To improve blood flow to child’s brain and reassure child as he/she recovers and make her comfortable. Causes A faint (also known as syncope) is a brief loss of consciousness that is caused by a temporary reduction of blood flow to the brain. It can be a reaction to pain or fright, or the result of an emotional upset, exhaustion or lack of food. It is more common however, after long periods of physical inactivity, such as standing still, especially in a warm atmosphere. The inactivity causes blood to pool in the lower part of the body, reducing the amount of oxygen available to brain. Assess * Brief loss of consciousness causing the child to fall to the floor. * Skin is pale, cold and sweating. * Pulse is slow. Assist child to the ground, lie on back, raising and support legs. Ensure there is plenty of fresh air; open a window if possible. Actions to take As they recover reassure them and help them to sit up gradually. There can be muscle twitching upon gaining consciousness. Look for and treat any injuries that have been sustained from falling. Medication None. Do not offer anything to drink until fully recovered. Medical assistance If consciousness is not regained quickly, open airway and check for breathing; be prepared to resuscitate if necessary. Have a second member of staff call 999 for ambulance. State: “Unconscious breathing/not breathing child”. Notification Parents should be notified after event to collect child from school, if necessary. Reviewed August 2015 To be reviewed August 2016 Page 18 Chilton Cantelo School Medical Policy Appendix G Head Injury Management Policy Aims & Objectives To be aware of the dangers and maintain a child’s safety following a concussion. Assessing the signs/symptoms of a serious head injury and ensuring immediate hospitalisation is provided for anyone suffering from a serious head injury. Causes Any blow to the head occurring during sports or accidents with a hard object including doors, walls, stairs, etc. If the blow is significant, a child can suffer from a severe concussion. The main risk of is a brain haemorrhage, which can lead to permanent damage if medical attention is not sought immediately. It can take up to 48 hours to develop severe head injury symptoms. * Assess Swelling, skin integrity and a state of confusion, memory loss, inability or vagueness relating to events before injury, dizziness, blurred vision, nausea, vomiting, and headache. * Strength and movement in extremities, equal and swift reaction of eyes to light. * Loss of consciousness even for a few seconds. * Straw-coloured fluid or watery blood from nose or ear indicates a skull fracture requiring immediate medical attention. 1. Headache, slight bump or swelling at the sight of injury, normal Actions to take neurological assessments and no other symptoms: Mild Concussion – no more sport that day, regular assessment/review of symptoms for 48 hours. Can remain in school – note sent home to parents/House Staff. 2. More symptoms present: Concussion – refrain from contact sports and physical activities for 3 weeks. Parents should collect child from school (whilst waiting for parents – monitor every 15 minutes) – close observation at home for new or progressing symptoms for 48 hours. Immediate medical attention to be sought symptoms progress. If there is loss of consciousness, even for a few seconds, with or without other symptoms, immediate medical assessment must be sought at A&E. Call ambulance if the child remains unconscious and/or symptoms of skull fracture as listed above. Parents should receive a Head Injury Advice following any kind of head injury. Medication Paracetamol for headache– if there are no other symptoms. Medical assistance Ambulance for symptoms of skull fracture and/or temporary loss of consciousness, or continued unconsciousness. For an unconscious child the ABC of emergency first aid should be followed. General Always contact parents. If a number of symptoms present the child must be collected from school. Reviewed August 2015 To be reviewed August 2016 Page 19 Chilton Cantelo School Medical Policy Head Injuries Minor head injury and knocks to the head are common, particularly in children. Following the injury, if the person is conscious (awake), and there is no deep cut or severe head damage, it is unusual for there to be any damage to the brain. However, symptoms of damage or bleeding may not develop for some hours, or even days, after a knock to the head. In rare cases, symptoms from a slow bleed can develop even weeks after a head injury. After a knock to the head, children will often cry, be distressed and then settle. It is then quite common for them to want to sleep for a short while. This is normal. However, it will appear to be a normal 'peaceful' sleep, and they wake fully. It is also normal after a knock to the head to have a mild headache. Sometimes there is also tenderness over bruising or mild swelling of the scalp. Paracetamol will help. A headache that becomes worse and worse is of more concern. Concussion is an injury to the brain occurring after a blow to the head. A blow to the head can cause the brain to move slightly within your skull, momentarily disrupting the electrical activity within some of the cells in the brain so that the brain stops working properly for a short period of time - this disruption can lead to the symptoms of concussion. Classically, someone with concussion has a headache, appears confused, and has loss of memory around the time of their head injury. They may also have lost consciousness briefly after the head injury (but not always). Vomiting and some temporary disturbance of vision can also be symptoms of concussion. Most people with concussion make a full and quick recovery and do not need any treatment. In most cases, concussion does not lead to any long-term problems. However, it is important to note that everyone who has had a head injury, however minor, does need close monitoring for a few days afterwards. This is because perceived symptoms of concussion could also be symptoms of a more serious problem such as bleeding within the brain. What you should not worry about: These symptoms should have disappeared over the two weeks following a head injury: Mild headache; Feeling sick (without vomiting) or decreased appetite; Difficulty concentrating; Increased tiredness which might make you irritable or anxious. General advice for anyone who has sustained a head injury: Rest for at least three days. Try to avoid stressful situations as these can make any symptoms worse. Do not return to your normal every day activity until you feel completely recovered. Do not work on a computer or play computer games until you have completely recovered. Do not drink alcohol until you are completely recovered. Do not play any contact sports for at least 3 weeks without consulting your doctor PROTOCOL: 1. A child sustaining a head injury during sports should be removed from the game; 2. Use CHECKLIST ONE to determine if the injured child has any symptoms that require the emergency services to be called and/or CHECKLIST TWO to determine if the injured child should be assessed by a medical practitioner in Accident & Emergency. 3. Apply cold pack for AT LEAST 20 minutes, repeat after 4 hours if necessary; 4. Give an age appropriate dose of paracetamol if required for headache; 5. Monitor for signs and symptoms for 48 hours after the injury; 6. If new symptoms develop seek advice according to checklists; 7. Follow the general advice and use the ‘Return to play protocol’ if applicable. Reviewed August 2015 To be reviewed August 2016 Page 20 Chilton Cantelo School Medical Policy CHECKLIST ONE Call the Emergency Services (999): Unconsciousness or lack of full consciousness; Difficulty understanding, speaking, reading or writing; Loss of feeling in part of the body; Problems balancing, general weakness, difficulty walking; Any changes in eyesight; Clear fluid running from the ears or nose; Black eye with no associated damage around the eyes; Bleeding or deafness in one or both ears; Bruising behind one or both ears; Penetrating injury, visible trauma to scalp or skull; Any seizure (‘convulsion or fit’); High impact injury, e.g. a fall of greater than one metre or more than 5 stairs CHECKLIST TWO Refer to an Emergency Department: Brief loss of consciousness (‘knocked out’) as a result of the injury from which the injured person has now recovered; Amnesia/confusion for events before or after injury; Persistent headache; Any vomiting episodes; Any previous brain surgery; History of bleeding or clotting disorder; Suspicion of non accidental injury; Irritability or altered behaviour (easily distracted, not themselves, no concentration, no interest in things around them). Adapted from McCrory et al (2005) 49 The majority of sport-related injuries will be simple concussions that will recover spontaneously over several days. In these situations, it is expected that rapid progress will be made through the step-wise return to play protocol. In the first few days following an injury, it is important to emphasis that physical and cognitive rest is required. Activities that require concentration and attention may exacerbate the symptoms and as a result delay recovery. The return to play following a concussion follows a step-wise process: Advice for Gradual Return to Sport After a Head Injury Step-wise return to play protocol to allow safe return. Symptoms have completely cleared at each exercise level for at least 24 hours before progressing to the next level. Symptoms such as: mild headache, dizziness, memory problems, poor concentration, irritability, tiredness or sleep disruption. Contact GP if symptoms are not improving. No return to any full sporting activity in less than one week. If unconscious or significant memory loss: no full contact activity (Level 5) within three weeks. Ask GP for advice before return to full contact activity. RETURN TO PLAY PROTOCOL LEVEL 1 No physical activity / complete rest LEVEL 2 Low levels of physical activity e.g. walking, light jogging LEVEL 3 Sport specific training or moderate levels of physical activity with body/head movement e.g. running in football, moderate jogging, brief running LEVEL 4 Heavy non-contact physical activity / training drills e.g. sprinting/running, routine non-contact sport-specific drills LEVEL 5 Full contact in controlled training / practice LEVEL 6 Full contact in games / return to competition Reviewed August 2015 To be reviewed August 2016 Page 21 Chilton Cantelo School Medical Policy Symptom free at each level for 24 hours before progressing. Reviewed August 2015 To be reviewed August 2016 Page 22 Chilton Cantelo School Medical Policy Appendix H Anaphylaxis Management Policy Aims & Objectives Causes To assist with the administration of emergency medicine in the event of an anaphylaxis reaction. In most cases allergic reactions are not always life threatening and can cause itchy, watery eyes and sneezing etc. as in hay fever. Mild reactions to food allergies or insect stings, medications or latex can cause a localised rash, itching/tingling of throat or tongue. These symptoms can be managed easily with oral antihistamines. However, some people are vulnerable to the most severe allergic reactions, known as anaphylaxis, which could result in death. Assess Anaphylaxis symptoms include (but not all may be present): Flushed, red face/neck, hives (nettle rash) anywhere on the body, itching and swelling, tightness in the chest, hoarse voice or swelling of the throat, abdominal pain, nausea or vomiting, dizziness or feeling faint, impending sense of doom, anxiety, unconsciousness and collapse. Open the emergency kit and follow the Individualised Care Plan. Actions to take How to use EpiPen: * Remove outer protective case, remove grey safety cap, hold EpiPen firmly and place the black tip at right angles to the outer thigh. Do not remove clothing. * While steadying the leg with your other hand, press the black tip firmly against thigh until a loud click is heard (the auto-injector mechanism is functioning and needle is now in the pupil’s leg muscle). * Hold the pen in place for 10 seconds (count slowly) while the adrenaline is being automatically injected into the pupil. * Remove the pen and massage the area. * Note the time of administration and keep pen safe to give to paramedics. After administration of EpiPen, stay with the child until ambulance arrives and help child into easy breathing position (leaning over slightly), loosen clothing and be prepared to place in recovery position if child becomes unconscious and resuscitate if necessary. If pupil has not shown any signs of improvement after 5 minutes, staff may administer a second Epipen IF AVAILABLE. Medication Only medication listed in the Individual Care Medical assistance Call 999 for the ambulance State “Anaphylaxis - Child”. Notification Parents’ to be called AFTER the ambulance is contacted. Reviewed August 2015 To be reviewed August 2016 Page 1 Chilton Cantelo School Medical Policy Appendix I Head Lice Policy General: Head lice are transmitted by direct, prolonged head to head contact. Most school will have a few children who have an active infection of head lice. This is often between 0% and 5%, rarely more – despite perception; there is rarely a “break-out”. An informed, sensible approach will help to limit, although not eradicate the problem. What to look for: • • • • • • • A head louse is a tiny six legged insect, which is between the size of a pinhead and a sesame seed. It is greyish brown in colour but can change colour to match the hair colour of the host, making detection difficult. The adult louse lives for about one month. Each leg ends with a claw, which grasps the hair, enabling swift movement close to the scalp. It does not walk on the scalp, cannot jump or fly and struggles on flat surfaces. It feeds only on human blood, approximately five times per day. The biting is not painful. Females out-number males in the ratio 4:1 and lay 6-8 eggs daily. Eggs are firmly glued to the strands of the hair, close to the scalp, preferring a temperature of 30-31 degrees, which is favourable to incubation. The incubation period is 7-8 days and within 10 days of hatching, the louse becomes an adult and begins to mate. Nits are empty egg cases. After an egg has hatched the egg case becomes white. If you have nits it does not always mean that you have head lice. Nits stay stuck to the hair and grow out as the hair grows, at a rate of 1cm per month. You only have head lice if you can find a living moving louse (not a nit). Facts about head lice: • • • • • • Lice will live on hair that is dirty or clean, short or long, adult or child. Short hair may make it easier for them to get from one head to another. High standards of personal hygiene do not necessarily prevent head lice. The main method of transmission is walking from head to head. The hairs must touch for duration of at least one minute. Head lice are not very infectious, taking time to spread through a population. They are less infectious than some other infections in children, such as chicken pox and impetigo. Lice cannot hop, jump, fly or be drowned. Should a louse be found on a hat, collar, pillow, chair back etc it will either be a dead louse or a damaged louse, too weak to hang on to the hair. Adult lice can live apart from humans for only a few days. It is unusual for infection to be caught in this way and it is very unlikely. Lice do not keep still and move very rapidly when disturbed. Most head louse infections are asymptomatic, but about one third of cases experience itching. The itching is due to sensitisation. For a first infection, it can take up to eight weeks for itching to start. With subsequent infections itching will occur sooner. Sometimes the appearance of a rash at the back of the neck is the first indication. Prevention and Detection: • • • • • All family members should brush/comb their hair twice a day. When hair is washed, damaged lice will float on the surface of the water. A black powder on the pillow in the morning may indicate the presence of lice, this is a mixture of black faecal powder and skin casts that can also make collars become dirty more quickly than normal. Children should have their own brush and be encouraged to adopt good grooming habits. Weekly detection combing of children is recommended but especially important when you know that head to head contact with an infected person has occurred or when members of the household have been named as contacts. The use of louse repellents should be discouraged, as they do not deal with the control of lice in the population, and they do not treat existing infection. Reviewed August 2015 To be reviewed August 2016 Page 2 Chilton Cantelo School Medical Policy Insecticides: Insecticide lotions are recommended for the treatment of head lice. Advice about which lotion to use can be obtained from: o The family doctor o The infection control nurse o The pharmacist A single treatment is considered as two applications one week apart. Insecticide shampoos are not recommended for two reasons: o They are susceptible to consumer abuse. o They have low efficiency in killing the eggs which form the resistance. Contact Tracing: Contact tracing means telling anyone who has had head to head contact with the infected person for more than one minute about the head lice infection, so that they can do detection combing and treat as necessary. Contact tracing is the responsibility of the family and not the school. All contacts with living moving lice should be treated at the same time. Action to be taken in School: If a member of the school staff suspects that a child has head lice they will ask for confirmation from the staff in the Medical Room/Boarding House. o The class teacher, or senior member of staff, will ask the parent to assess their child as soon as practicable to confirm the diagnosis. Parents who report cases of head lice to the school will be advised to contact the staff in the medical room for advice and support. All reported cases would be kept Confidential. Exclusion of children from school is not necessary as long as treatment is being undertaken. The school will collaborate with the staff in the Medical Room in the provision of educational information to parents/ carers and children about head lice. Detection Combing You need: warm water, towel, detection comb, good lighting, and ordinary brush/comb. 1. 2. 3. 4. Wet the hair, and then dry it with a towel. The hair should be damp, not dripping. Make sure there is good light, daylight is best. Comb the hair with an ordinary comb. Start with the teeth of the detection comb touching the skin of the scalp at the top of the head. Draw the comb carefully towards the edge of the hair. - Look carefully at the comb in good light. Do this over and over again from the top of the head to the edge of the hair in all directions, working around the head. It takes 10-15 minutes to do it properly for each head. 5. 6. 7. If there are lice, you will find one or more lice on the teeth of the comb. It may help to rub a handful of conditioner into the hair. If you do, you will need to wipe it off the comb with tissue paper and look for more lice. Head lice are little insects with moving legs. They are often not much bigger than a pinhead, but may be as big as a sesame seed. Clean the comb under the tap. A nailbrush will help to do this. If you find something and are not sure what it is, stick it on a piece of paper with sticky tape and show it to your School Nurse or doctor. There can be other things in the hair which are not head lice. Reviewed August 2015 To be reviewed August 2016 Page 3 Chilton Cantelo School Medical Policy Appendix J Policy for the Safe Disposal and Clearing of Vomit Location of Bodily Fluid kits: Preparatory department; Prep-Preparatory department; Laundry; Medical room; Boarding Houses. Bodily Fluid kits contain: Vomit bags or bowls, scraper, coagulant powder, gloves, apron, mask, yellow sealable bag, disposable cloths, disinfectant, wipes and alcohol hand gel. When a child is ill (during the School day): 1. Contact the Medical Room – a member of staff will remove and clean up the child; 2. Contact the domestic team who will arrive to clean up bodily fluids; Bodily Fluids are removed by: o o o o o o o Sprinkling the coagulant powder over the area, congealing any fluid into lumps. Wearing gloves, mask and apron; removing and disposing of the congealed fluid in the yellow “clinical waste” bag. Disinfecting the surfaces. Discarding any used items into the yellow bag. Sealing and disposing of all waste in a Clinical Waste bin. Used Bodily Fluids kits should be returned to the cleaning supervisor who will restock and replace. All staff members are asked to thoroughly wash their hands and use alcohol hand gel. When a child is ill at night time: o o o o If a child is ill with vomiting or diarrhoea at night in the boarding house, they should, wherever possible be isolated from the other children to prevent the spread of germs. Any bodily fluids should be cleaned up as per the guidelines above. Soiled bedding should be taken to the laundry as soon as possible the following morning. Any child who has been sick, or who has diarrhoea must be excluded from school for a period of 48 hours from the last episode. For boarding children who live locally – contact the parents and ask them to collect their child. For overseas boarders or those who live too far away, isolate them in the Sanatorium during the day (Mon to Fri). If they are unable to return to their boarding house at night, House Staff will arrange for a suitable adult to provide supervision and care. Return the used bodily fluid kit to the Cleaning Supervisor for restock and replacement. Reviewed August 2015 To be reviewed August 2016 Page 4