Confidential Healthcare for Adolescents and Teens
advertisement

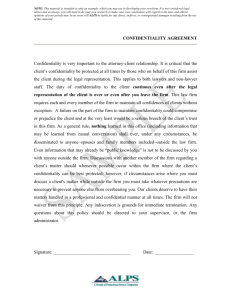
Confidential Healthcare for Adolescents and Teens The management of healthcare information is strictly regulated by the federal Privacy Act of 1974 and provisions under this act such as the Health Insurance Portability and Accountability Act (HIPPA) of 1996. Some of these provisions, such as HIPPA, are meant to protect the patient’s right to privacy and uphold physician-patient confidentiality as well as the confidentiality of medical records and personal medical information. However, this wealth of legislature concerning healthcare confidentiality only completely applies to adults and does not protect the privacy of minors from their legal guardians or healthcare decision-makers. This failure of federal law to protect adolescent’s medical privacy creates an ethical dilemma for the physicians attending these patients who can choose to uphold patient confidentiality and face possible liability issues, or forego confidentiality and risk losing the trust of the patient. According to the Arizona Medical Association on Consent and Confidentiality in Adolescent Health Care, “There is no single Arizona statute that deals specifically with the confidentiality of a minor’s medical records” (Birkholz 12). The responsibility of sustaining an adolescent patient’s right to privacy and confidentiality falls on the discretion of the physician and is constrained by their offices’ management of medical records and its billing procedure. Although not dictated by law, adolescents, like adults, have an innate human right to privacy and confidentiality, especially in the sensitive area of health care. It is often the physician’s professional judgment that determines a minor’s ability to consent to medical care and whether or not that care should remain confidential. Although a physician may elect to uphold an adolescent’s confidentiality, the release of medical records and insurance billing charges to a legal guardian can hinder these efforts and violate this privacy. Certain Title-X funded clinics such as Planned Parenthood exist with offices, records, and billing procedure designed to support a more confidential system of care than a primary physician’s office. However, until the general practice of healthcare record keeping and insurance billing is updated, adolescents will be at a constant risk for a breach of confidentiality. Confidentiality, specifically for teen adolescents, offers a sense of autonomy that encourages these patients to seek out the necessary treatment or preventative care that they would otherwise forego out of embarrassment or fear. Treatment for diseases considered taboo such as STI/STDs, HIV, depression, and family planning services such as birth control and abortion, if shared with a minor’s guardian, could result in violence, shame, and family tension. According to the Guttmacher Institute, “In two large nationally representative surveys, approximately a quarter of middle and high school students reported having foregone health care they needed” and a third of these students stated their reason as “not wanting to tell their parents” ( English vol 36 ). Lack of medical treatment not only endangers the adolescent patient, but also creates a public safety issue. A patient who, fearing a breach of confidentiality, waives treatment or testing for STDs can inadvertently spread the disease to other adolescents and a minor who cannot obtain parental consent or a judicial waiver for abortion services may seek a dangerous “back-alley” abortion. Attitudes towards adolescent confidentiality differ between physicians, and adolescent patients do not always have an explicit understanding of how their confidentiality may be handled. Depending on their situation, it is important for minor patients to open a discussion with their physician on the confidentiality of their medical information. This is an action all adolescents can take to ensure they understand the physician’s stance on adolescent patient privacy and the limitations to the confidentiality of their information. Although state laws allow for the confidentiality of STD testing, HIV, mental health, and family planning services to be upheld for consenting adolescent patients, insurance billing is still a major logistical obstacle in providing completely confidential care and it is still the physician’s judgment to determine the ability of a minor to consent. Future physicians and policy-makers need to determine guidelines for a minor’s capacity to consent to confidential health care, and physicians’ offices’ methods of record-keeping and charting should be updated to account for adolescent confidentiality. The privacy laws currently in effect also need to be updated to view consenting minors as autonomous from their legal guardians in regards to medical information and treatment. If adolescent healthcare is to improve, to become safer, and more effective, confidentiality for minors must be supported by policy, physicians, and even parents. Works Cited Birkholz, Karla. "Issues of Confidentiality." Consent and Confidentiality in Adolescent Healthcare: A Guide for the Arizona Health Care Practitioner. 3rd ed. Phoenix: Arizona Medical Association, 2011. 31. Print. English, Abigail. "The HIPAA Privacy Rule and Adolescents: Legal Questions and Clinical Challenges." Perspectives on Sexual and Reproductive Health. 2nd ed. Vol. 36. Chapel Hill: Guttmacher Institute, 2004. Print.