Histology Practical 24) Lymph node 25) Thymus 26) Spleen 27
advertisement

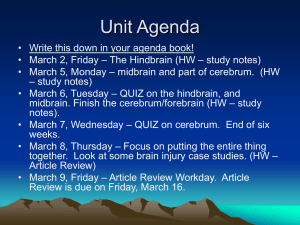
Histology Practical 24) Lymph node 25) Thymus 26) Spleen 27) Palatine Tonsil 28) Root of Tounge General Information about lymphatic tissue: Red bone marrow Thymus Primary Lymphatic organs. All others are secondary. What is the stroma of the Network? Reticular fibers! Native lymphocytes are released from primary lymphatic organs but have to be immune competent Only secondary lymphatic Organs posses lymphatic follicles B-Cells = immunoglobines require B-Cell Receptors (BCR) therefore lymphatic follicles occur function: keeping the own antigen environment, eliminating the foreign substances/antigens lymphoid tissue lymphoid organs: primary (red bone marrow, thymus): development of lymphocytes secondrary(lymph node, spleen, tonsils, Peyer s patches, appendix): mature lymphocytes can be found here basic tissue: lymphoreticular- reticular connective tissue, reticular fibers, reticular cells; thymus: epithelial reticular cells main cell types: lymphocytes, macrophages, dendritic cells, endothelial cells Lymphoid follicles unit of the lymphoid tissue round, oval structure, many lymphocytes primary: dark, ruond, little lymphocytes, intrauterine secondary: bigger (200-400 m), originating from the primary, in the middle: light area- germinal center (centroblasts, centrocytes, FDC), peripheral: cap zone 24) Lymph node Mantle zone Lymphatic follicles Cortex (inner / outer zone) Anastomosing network of lymphoids Medulla: o Medullary cord (dark) o Medullary sinuses (pale) Cortex: inner B-Cell Zone Medulla: B-Cell zone along the course of lymphatic vessels bean-shaped, encapsulated organs afferent lymphatic vessels efferent lymphatic vessels Copyright by Matthias Heyner Based on the Histology practical from E. Dobo et. al at the University of Szeged videos by WashingtonDeceit (www.youtube.com/user/WashingtonDecit) connective tissue capsule trabeculae hilus among trabeculae: reticular connective tissue cortex: lymphoid follicles (B dep. zone) paracortex: no lymphoid nodules (T dep. zone) medulla: medullary lymphoid sinuses, medullary cords marginal sinus intermediate sinus medullary sinus efferent lymphatic vessels (hilus) Lymph node: Lymph node Reticulin fibers: Copyright by Matthias Heyner Based on the Histology practical from E. Dobo et. al at the University of Szeged videos by WashingtonDeceit (www.youtube.com/user/WashingtonDecit) CD (cluster differentiation) marker: CD19 & CD20: B-Cells CD3: all CD4: helper CD8: cytotoxic 25) Thymus Lobulated organ, it has septa which separate the lobules Cortex is darker Medulla is paler Lymphocytes wander from cortex to medulla In the Medulla there are larger cells No incoming just outgoing. Hassals corpuscle o Pinkish mass in center o Can only be found in Medulla o Has no function for thymus epithelial, lymphatic, adipose form during life 2 lobes+ capsule lobules cortex: peripheral, darker, thymocytes, macrophages, epithelial reticulum cells medulla: central, lighter, more epithelial reticulum cells, Hassal-corpuscules (eosinophil,concentrically arranged,flattened epithelial cells with keratohyalingranules), neuroendocrine cells, myoid (Hammar)cells no lymph follicles function: mature and differentiation of T lymphocytes blood-thymus barrier: pericytes, capillary basal lamina, basal lamina of the epithelial reticular cell, cells of the endothelium, epithelial reticular cells Copyright by Matthias Heyner Based on the Histology practical from E. Dobo et. al at the University of Szeged videos by WashingtonDeceit (www.youtube.com/user/WashingtonDecit) Copyright by Matthias Heyner Based on the Histology practical from E. Dobo et. al at the University of Szeged videos by WashingtonDeceit (www.youtube.com/user/WashingtonDecit) 26) Spleen Main color pinkish because of the erythrocytes but there are also small bluish spots intraperitoneal organ connective tissue capsule trabeculae parenchyma (pulp) red pulp (80%), white pulp (20%) reticular connective tissue, reticulum cells, reticular fibers red pulp: Billroth s cords, sinuses white pulp: PALS (A. centralis- T dep. zone), lymhoid follicles Malpighi (B dependent), marginal zone open and closed circulation Copyright by Matthias Heyner Based on the Histology practical from E. Dobo et. al at the University of Szeged videos by WashingtonDeceit (www.youtube.com/user/WashingtonDecit) Copyright by Matthias Heyner Based on the Histology practical from E. Dobo et. al at the University of Szeged videos by WashingtonDeceit (www.youtube.com/user/WashingtonDecit) 27) Palatine tonsil lymhoid tissue in the mucosa Waldeyer s lymphatic ring: o pharyngeal tonsils o palatine tonsils o tubal tonsils o lingual tonsils tonsillary epithelium+ lymhoid tissue (lymphoreticular connective tissue) tubal and pharyngeal t.: ciliated pseudostratified epithelium with goblet cells lingual and palatine t.: stratified squamos nonkeratinized epithelium epithelium crypts: lingual t.- shallow, wide// palatine t.: narrow, deep lingual t.: seromucous glands crypts, strited muscle fibers follicles (B dep.), interfollicular area (T dep.) epithelium is often infiltrated with lymphocytes Palatine tonsil Copyright by Matthias Heyner Based on the Histology practical from E. Dobo et. al at the University of Szeged videos by WashingtonDeceit (www.youtube.com/user/WashingtonDecit) Pharyngeal tonsil Lingual tonsil Copyright by Matthias Heyner Based on the Histology practical from E. Dobo et. al at the University of Szeged videos by WashingtonDeceit (www.youtube.com/user/WashingtonDecit) Copyright by Matthias Heyner Based on the Histology practical from E. Dobo et. al at the University of Szeged videos by WashingtonDeceit (www.youtube.com/user/WashingtonDecit) Copyright by Matthias Heyner Based on the Histology practical from E. Dobo et. al at the University of Szeged videos by WashingtonDeceit (www.youtube.com/user/WashingtonDecit)