Job description - East Midlands Deanery
advertisement

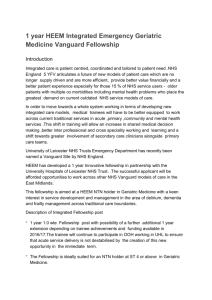
HEEM Integrated Fellowship in Paediatric Respiratory Medicine (1.0 WTE) Introduction Integrated care offers patients highly coordinated and tailored care based on individual need, regardless of complexity. NHS England ‘5YFV’ articulates a future of new models of patient care; which improve patient experience, are financially efficient and enhance the care of those with long term conditions. The development and acceptance of integrated care models require current medical trainees to train across current traditional services in Acute, Primary, Secondary, Community and Mental Health. This shift in training experience will enhance shared medical decision-making and improve cross specialty and inter professional working, learning and job satisfaction. Primary Care experts will work within specialist networks and alongside secondary care expert teams. In 2015, NHS England invested £200 million in the development of 29 vanguard geographies; 4 of these ‘game-changing’ care models have been established in the East Midlands; with one of the multi-speciality Community Provider sites being based at the large Lakeside Surgery, in Corby, Northamptonshire. The Paediatric Fellowship This 1 year innovative Fellowship has been developed to support the future service and workforce requirements in Paediatrics and Child Health, in the East Midlands. The Fellowship is aimed at a level 3 trainee in Paediatrics [ST6 or above] who holds a HEEM National Training Number. It would be highly desirable if the trainee is or was committed to grid training in Paediatric Respiratory Medicine. Asthma is the commonest chronic condition in childhood affecting approximately 1 million children in the UK. The vast majority of children with asthma are managed in Primary care and only those patients with severe and complex asthma require specialist input. Exacerbation rates in children with asthma have remained high over the last decade and this is a considerable burden for the NHS budget. Acute and complex presentations frequently require hospital admission and are associated with a significant mortality highlighted in the NRAD report published in 2014. Part of the problem is that objective tests to diagnose and monitor asthma are not usually available in primary care and this has been highlighted in a recent NICE guideline on the diagnosis and management of asthma, currently published in draft format. The project associated with the Fellowship will evaluate the training and capacity requirements in primary care to deliver the NICE asthma diagnostic guidance in children and to evaluate the impact of implementing the guidance on processes and outcomes of care. This Fellowship will afford an opportunity to a senior trainee in Paediatrics to develop enhanced management and leadership skills by working in collaboration with Primary Care and Tertiary specialists, to improve outcomes for this patient group. The Fellow will have the opportunity to work, learn and teach across traditional acute and community boundaries, acquiring new skills and developing new systems for local and national care. The Fellow will lead the implementation of the project under the supervision of Dr Erol Gaillard, Consultant Paediatrician/Senior Lecturer at Leicester University and supported by a senior Primary Care Physician. The project will be implemented across a number of GP practices across Leicestershire and the NHS Vanguard site in Corby. The project will be supported for a further 12 months depending on resources availability and satisfactory progression of the trainee. This would allow the applicant an opportunity to complete a Masters level qualification in Leadership and Management (funded within the fellowship). The trainee will be OOPE for the duration of the Fellowship. Proposed Timetable [12 months] - 0.8 WTE to support the academic project and to support 60 credits of a higher qualification in Leadership and Management - Up to 0.2 WTE to support experiential learning at the Vanguard site. - On call duties for Paediatrics at UHL are TBC with the clinical service lead Governance of the Fellowship The Fellow will be employed by University Hospitals of Leicester, NHS Trust for the duration of the fellowship and hold an honorary contract with any partnership host NHS organisation for the duration of the fellowship where the Fellow will be working and training (Lakeside Surgery). The final clinical timetable and outcomes for the Fellowship will be agreed between the Fellow, UHL NHS Trust and Lakeside Surgery. The Associate Postgraduate Dean responsible for HEEM Fellowship development will sign off the clinical job plan before the start of the Fellowship. Academic supervision will be provided by Dr Gaillaird, assisted by an identified GP Supervisor at Lakeside. Dr James Whitelaw (TPD for Paediatrics and Consultant at UHL) will provide additional specialist mentoring for the Fellow. This arrangement should ensure all opportunities for personal and professional development, in a novel learning environment, will be identified and supported. The newly appointed NHS Vanguard site at Corby will provide specific opportunities for Fellows to acquire both clinical and non-clinical capabilities in rapidly emerging new models of care and allow the Fellow to contribute to service development. The Fellow will have agreed SMART objectives for the Fellowship. These objectives will be signed off within 2 weeks of the start of the Fellowship by all partners and will form the basis of the Fellows learning agreement with HEEM.