Student Catalog - Nature Coast EMS

NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
3876 W Country Hill Drive
Lecanto, Florida 34461
352-249-4750 www.naturecoastems.org
VOLUME NUMBER 9
Student Catalog
EFFECTIVE: November 25, 2014
Emergency Medical Technician
Emergency Medical Technician - Online
Paramedic
License Number 4158
Licensed by the Commission for Independent Education
325 W. Gaines Street, Suite 1414, Tallahassee, FL 32399-0400
(888) 224-6684
To be eligible for certification as a Florida EMT, an applicant must follow guidelines as outlined by the Florida Department of Health, Office of EMS and Medical Quality Assurance. For more information about EMT and Paramedic certification contact:
Florida Department of Health
Division of Medical Quality Assurance
EMT/Paramedic Certification Office
4052 Bald Cypress Way, Bin C85
Tallahassee, FL 32399-3285
Phone: (850) 488-0595
Fax: (850) 921-6365
Web: www.doh.state.fl.us/mqa/EMT-Paramedic
Page 1 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Table of Contents
Introduction
Staff Directory
State License and Affiliations
Mission and Vision
Tuition and Fees 7
Admissions Policy and Procedures 7
General Application Procedures 8
3
4
4
4
Transfer of Credits
International Students
Clock Hours
Program Hours
Admission Requirements
Course Curriculum Summary
Student Evaluation
8
8
8
9
9
10
10
Grading Policy
Incomplete Grade
12
13
Standards of Satisfactory Progress 13
Academic Probation 13
Overall Course Completion
Conduct
Attendance
Sick Call
Inclement Weather
Student to Instructor Ratio
13
14
16
16
16
17
Absences from Classroom
Absences during Lab Practical
Make Up Work
Prohibited Conduct
Patient Confidentiality
Dress Code
Equipment Policy
Telephone
Discipline Procedures
Administrative withdrawals
Student Appeal
Student withdrawal and
17
17
17
18
19
19
19
20
20
20
20
Refund Policy 21
Extended Enrollment Status 21
Reestablishing Eligibility Reentry 21
Financial Aid 22
Lost Property 22
Academic Advising and Tutoring 22
Description of Facilitites 23
Parking
Student Library
Discrimination Policy
Student Advocacy
Record Keeping
Job Placement Assistance
Indemnification
Introduction to
Paramedic Clinical
23
23
23
23
23
24
24
24
Paramedic Objectives and Description
Paramedic Hospital Clinical
Requirements
25
30
Paramedic Field Clinical
Requirements 37
EMT Objectives and Description 42
Introduction to EMT Clinical 46
EMT Hospital Clinical
Requirements 48
EMT Field Clinical Requirements 48
Textbooks and Resources 55
Holiday and Academic Calendar 55
Student Services 55
Sexual Harassment and
Discrimination
Accreditation Status
Equipment list
55
57
58
Page 2 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Introduction
Nature Coast Emergency Medical Institute is a school providing Emergency Medical Technician and Paramedic education. Nature Coast Emergency Medical Institute also conducts various
Basic Life Support (BLS) and Advanced Life Support (ALS) continuing education courses.
Purpose of the Nature Coast Emergency Management Institute:
To set the standard for EMS training in the Citrus County area and prepare clinically competent, technically proficient graduates for positions as entry-level EMTs or Paramedics in the municipal, voluntary, and private sectors.
We will accomplish this by:
Providing an environment that is conducive to learning and supportive to the student.
Providing students with the necessary support and guidance including counseling, remediation and tutoring.
Ensuring that students have equipment available to learn, practice, and perfect their skills and knowledge.
Hiring faculty who are experts in their field and knowledgeable in these disciplines.
Ensuring that the students have access to a wide variety of clinical experience through affiliation agreements for clinical rotations and field externships.
Helping students seek employment upon completion of program and certification.
Statement of Ownership:
Nature Coast EMI is a 501(c) (3) not-for-profit organization that reports to a Board of Directors that serves as the Corporate Officers. Board of Directors include: Daniel Griffin, James Finney,
Carole McHugh, Eloy Nunez and Bonnie Rybek.
Upon successful completion of the EMT and Paramedic program Nature Coast EMI issues each student a Florida Department of Health approved program diploma that complies with the professional education requirements for course completion of the State of Florida. Please note that successful completion of the State of Florida certification examination licenses the individual as an EMT or Paramedic.
The Nature Coast EMI School is not accredited. Students are not eligible for Title IV federal financial assistance or State of Florida student financial assistance.
Questions for the Commission for Independent Education can be addressed to:
Commission for Independent Education
325 West Gaines Street, Suite 1414
Tallahassee, FL 32399-0400
Phone: 888-224-6684 Fax: 245-3234 CIE Website: www.fldoe.org/cie
State License and Affiliations
Nature Coast Emergency Medical Institute is licensed by the Commission for independent
Education and the State of Florida Department of Health.
Page 3 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Mission of Nature Coast Emergency Medical Institute Education
Nature Coast Emergency Medical Institute provides a learning environment facilitated by
“hands-on” training and active participation.
Students will be proficient and competent in all knowledge and skills required by both the
State of Florida and the United States Department of Transportation paramedic.
Students will be prepared to successfully complete the National Registry of Emergency
Medical Technicians and State of Florida Paramedic examination.
Students will be instilled with the discipline to carry themselves as medical professionals and to provide competent and quality pre-hospital care.
We will use only competent and experienced instructors that provide up to date instruction.
The outcome of our program will be a cadre of competent, highly qualified entry-level EMS professionals to work within healthcare organizations.
Vision
Nature Coast Emergency Medical Institute is a state of the art pre-hospital care training center for Florida’s Nature Coast and will offer initial education, continuing education and specialty credentialing courses. Nature Coast Emergency Medical Institute is an accredited institution providing students the opportunity to successfully complete EMS related education.
Staff Directory
President/CEO
Office Phone: (352) 249-4700
Email: mikeh@naturecoastems.org
Mike Hall
The President/CEO is responsible for Nature Coast EMS’s mission and objectives and oversees operations and leadership programs. The President/CEO is responsible for developing all clinical locations to include hospitals, clinics, and pre-hospital care providers. The
President/CEO will be knowledgeable concerning current State of Florida and National Registry accreditation requirements for certification and licensure. The President/CEO will provide longrange planning and ongoing development of the Nature Coast Emergency Medical Institute programs. The President/CEO will be the direct liaison with the Medical Director and develop cooperative involvement with area departments and services. The President/CEO may delegate responsibility to other program faculty as appropriate.
Medical Director
Office Phone: (352) 249-4700
Mary Anne Kolar, D.O.
Email: makdo2@gmail.com
The Medical Director will review and approve all educational content of the programs offered by
Nature Coast EMS. The Medical Director will review and approve the content of medical instruction and the supervision and evaluation of students. The Medical Director will assure and
Page 4 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion attest to the competence of each graduate in the cognitive, psychomotor and affective domains.
The Medical Director will have experience and current knowledge of all EMS practices regarding acutely ill and injured patients. The Medical Director will be knowledgeable about the paramedic educational programs and the legislative/regulatory issues regarding educational programs for pre-hospital providers. The Medical Director will be an active member of the local
EMS community and occasionally facilitate lectures for the school.
Program Director
Office Phone: (352) 249-4751
Email: janeb@naturecoastems.org
Jane Bedford
Cell Phone: 352-302-8486
The Program Director is responsible for the daily operations of paramedic programs including continuing education programs. The Program Director will have the appropriate education, training and experience as an educator to fulfill the role. The Program Director will have field experience in the delivery of pre-hospital care. The Program Director shall be responsible for the effectiveness of the EMS programs. This will include classroom scheduling, instructor scheduling, AV presentation setup, student record handling and other assigned duties.
Paramedic Lead Instructor and Clinical Coordinator
Office Phone: (352) 249-4760
Email: ronaldb@naturecoastems.org
Ron Bray
Cell Phone: 352-400-1191
The Lead Instructor is responsible for managing all Nature Coast EMI offered Education
Programs including effective coordination between Education Director and education programs offered to internal and external students. Maintain compliance with standards, rules and regulations at all times. Function as the Lead Instructor responsible for coordinating and conducting the EMS Education Programs and maintain credentials to and teach any and all classes offered by Nature Coast EMS Education. The EMS Educator shall have at least equivalent academic training and preparation and hold all credentials for which the students are being prepared. The EMS Educator acts as the liaison between the students, Nature Coast EMS, the local medical community, and the state-level certifying agency. In addition, is responsible for assuring that the course goals and objectives set forth by the Department of Education and
Florida Office of EMS are met. The lead instructor may also serve as the Primary/Lead
Instructor responsible for the teaching of a specific lesson(s) of the EMT- Basic/Online or
Paramedic course. This individual shall be knowledgeable in all aspects of pre-hospital emergency care, in the techniques and methods of adult education, and managing resources and personnel. This individual shall be present at most, if not all, class sessions to assure program continuity and to be able to identify that the students have the cognitive, affective, and psychomotor skills necessary to function as an Emergency Medical Technician Basic or Paramedic.
The Clinical Coordinator is responsible for scheduling of clinical time for students who require clinical rotations. The Clinical Coordinator will serve as the liaison for the clinical sites and will conduct random clinical site inspections to evaluate student and preceptor performance. The
Clinical Coordinator will assist the Program Director to ensure that all program clinical requirements are met.
Page 5 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
EMT Lead Instructor and Clinical Coordinator
Office Phone: (352) 249-4734
Email: lori.thompson@naturecoastems.org
Lori Thompson
Cell Phone: 352-601-7330
The Lead Instructor is responsible for managing all Nature Coast EMI offered Education
Programs including effective coordination between Education Director and education programs offered to internal and external students. Maintain compliance with standards, rules and regulations at all times. Function as the Lead Instructor responsible for coordinating and conducting the EMS Education Programs and maintain credentials to and teach any and all classes offered by Nature Coast EMS Education.
The EMS Educator shall have at least equivalent academic training and preparation and hold all credentials for which the students are being prepared. The EMS Educator acts as the liaison between the students, Nature Coast EMS, the local medical community, and the state-level certifying agency. In addition, is responsible for assuring that the course goals and objectives set forth by the Department of Education and Florida Office of EMS are met. The lead instructor may also serve as the Primary/Lead Instructor responsible for the teaching of a specific lesson(s) of the EMT-Basic/Online or Paramedic course. This individual shall be knowledgeable in all aspects of prehospital emergency care, in the techniques and methods of adult education, and managing resources and personnel. This individual shall be present at most, if not all, class sessions to assure program continuity and to be able to identify that the students have the cognitive, affective, and psychomotor skills necessary to function as an Emergency Medical Technician
Basic or Paramedic.
The Clinical Coordinator is responsible for scheduling of clinical time for students who require clinical rotations. The Clinical Coordinator will serve as the liaison for the clinical sites and will conduct random clinical site inspections to evaluate student and preceptor performance. The
Clinical Coordinator will assist the Program Director to ensure that all program clinical requirements are met.
Student Services Coordinator Jerri Regan
Office Phone: (352) 249-4725
Email: jerri.regan@naturecoastems.org
The Student Services Coordinator serves a resource person responding to question, triaging calls and assisting students with the application process.
FACULTY:
Jane Bedford Paramedic, EMT BA, Ashford University
Ronald Bray Paramedic, EMT AS, Orlando Medical Institute
Lori Thompson Paramedic, EMT AS, Orlando Medical Institute
Floyd Mead Paramedic, EMT AS, Ashford University
Page 6 of 60
Tuition and Fees
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Tuition and any other fees are to be paid in full prior to the first day of class. Acceptable payments are in the form of a Certified Check, Money Order or Credit Card. All payments are made payable to Nature Coast EMI and presented to the administration office during office hours (9:00 am – 5:00 pm) Monday through Friday.
Nature Coast EMI faculty is not authorized to accept any tuition or any form of payment.
Tuition reimbursement is calculated according to the date that the student drops a course or courses. Refund applications are available in the school office. In cases of Medical Leave of
Absence, the refund is computed according to the effective date of the leave. Non-instructional fees are non-refundable except if the program is cancelled by the school or the student enters the military. Non-instructional fees are clinical and computer base labs which are purchased for each student by the school.
Program Fees:
EMT Paramedic
Registration Fee: $ 150.00 $ 150.00
(Non-refundable and includes a drug screen and background check)
Tuition: $ 1,510.00 $ 5,020.00
Lab Fees: $ 55.00 $ 155.00
Books & Supplies: $ 385.00 $ 930.00
TOTAL: $ 2,100.00 $ 6,255.00
Please note that optional additional fees include:
EVOC $ 180.00
Exam Prep Class $ 80.00
Admissions Policy and Procedures
Nature Coast Emergency Medical Institute welcomes qualified applicants seeking a challenging and demanding pre-hospital course that will provide the skills and knowledge base to begin an exciting and rewarding career. A “rolling” admissions policy governs most of Nature Coast
Emergency Medical Institute programs and programs are scheduled throughout the calendar year.
Applicants must complete the Nature Coast Emergency Medical Institute application packet. Each prospective student must provide proof of high school graduation or GED.
Official transcripts must be provided prior to enrollment but no later than 30 days after
Page 7 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion the start of the initial term of enrollment. Transfer students must provide official transcripts prior to the beginning of any courses.
All applicants are required to successfully complete a standardized entrance examination.
The Program Director has the authority to waive the examination requirement of an applicant who has satisfactorily completed the minimum equivalent of an Associate’s
Degree at the post secondary level.
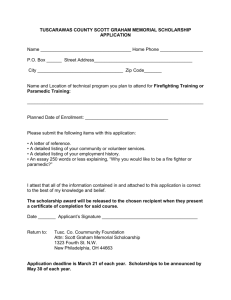
General Application Procedures
Complete an application, which can be downloaded from our web site www.naturecoastems.org
1.
Completed program application
2.
A non refundable registration fee of $150.00 due at time application is submitted.
3.
Must be at least 18 years of age for paramedic programs and 17 for EMT programs.
4.
Valid State of FL Drivers License and Social Security Card.
5.
High School Diploma or G.E.D.
6.
Documentation of annual physical exam with the last 12 months for EMT programs and 6 months for Paramedic programs, and you must currently be in good physical health.
7.
Documentation of current immunizations.
8.
Pass NCEMI authorized background check and drug screen.
9.
Pass a NCEMI entrance exam.
10.
Approval by Program Director to be enrolled into program after background check.
11.
Valid AHA Healthcare Provider CPR card.
Paramedic students must have Florida State EMT certification in good standing before completion of 382 hours of paramedic program.
Transfer of Credits: Nature Coast Emergency
Medical Institute is a diploma program and does not award credits or accept credits for transfer
Transferability to another institution will be at the receiving institution’s discretion.
International Students
International students wishing to enroll in Nature Coast Emergency Medical Institute programs must demonstrate legal immigration status and must demonstrate that they have graduated from a secondary school recognized by the Ministry of Education or equivalent entity. All international students must show proof of English language competency. Students must demonstrate that they are able to meet all costs of their education without any financial aid unless they are eligible noncitizens.
Page 8 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Clock Hours
A clock hour is defined as period of 60 minutes with a minimum of fifty minutes (50) of instruction in the presence of an instructor followed by a ten-minute (10) break.
Emergency Medical Technician 250 Clock Hours
Paramedic 1218 Clock Hours
EMT Program Hours
Classes are approximately four (4) hours per day and are held on a schedule that alternates from three to four days a week Evening classes are on Monday, Wednesday and Thursday from 6pm to 10pm. Skills lab will alternate days and will be on a first come first serve basis.
Paramedic Program Hours
Classes are approximately seven (7) hours per day and are held on a “shift friendly” schedule that alternates from one to two days a week. Day classes are routinely from 9am to 4pm.
Evening classes are routinely on Monday, Thursday and Friday from 6pm to 10pm. Class schedule is subject to change due to holidays and class needs. The class syllabus offers the official program schedule for each class.
Admission Requirements for the Paramedic Program
1.
Completed application
2.
$150 application fee (Non-refundable and includes background and drug screening)
3.
Must be at least 18 years of age.
4.
Florida State Drivers License and /or Identification card
5.
High School graduate or G.E.D.
6.
To be in good health with documentation of a physical exam within the last 12 months.
7.
Provide documentation of current immunizations
8.
Current AHA Healthcare Provider CPR Card
9.
Current Florida State EMT before completion of 382 paramedic program hours.
10.
Pass an entrance examination
11.
Interview with the Program Director and/or Designee
Applicants are selected based on grades on the screening exams, interview results, and other considerations such as background, education, and experience. The paramedic student must maintain both the CPR and the EMT certification throughout the paramedic program. In order to graduate, the paramedic student must successfully complete the AHA ACLS certification.
Admission Requirements for the EMT Basic
1.
Completed program application and a non refundable application fee of $150.00 due at time application is submitted.
2.
Must be at least 17 years of age and reach the age of 18 before taking Florida EMT Exam.
3.
Valid State of FL Drivers License and Social Security Card.
Page 9 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
4.
High School Diploma or G.E.D, or “Intent to graduate” for High School Seniors.
5.
To be in good physical health with documentation of physical exam within the last 12 months.
6.
Documentation of current immunizations including MMR and Hepatitis B (optional) and
TB test within the last 12 months.
7.
Pass NCEMI authorized background check and drug screen
8.
Pass a NCEMI basic aptitude test.
9.
Approval by Program Director to be enrolled into program after background check
10.
Valid AHA Healthcare Provider CPR card.
11.
Ability to lift 125 pounds
Course Curriculum
The curriculum includes classroom, online (EMT online program), laboratory sessions, and clinical externships. These courses will emphasize skills and knowledge needed for an entrylevel EMT or paramedic.
Student Evaluation
Students will be evaluated on their academic, psychomotor and effective performance in the program.
Cognitive Evaluation
Didactic evaluation will consist of written examinations and quizzes and oral examinations. The written evaluation will contain a variety of question types including multiple choice, true/false, matching, situational, short answer and essay. Learning objectives are part of the instruction ensuring that students are aware of the focus/objectives for each examination. Those objectives will cover basic or online EMT/Paramedic skills/knowledge as well as advanced skills and knowledge. Material covered on quizzes/exams is based on:
Reading assignments
Lecture materials
Handouts
Practical Skills Sheets
Policies and Procedures
Any other material covered in the course
Assigned reading
An overall grade average of 80% or better must be maintained for successful completion of the course. If a student’s average falls below 80%, he/she will be placed on academic probation.
The student will then be required to bring his/her average up to 80% or higher on the next two
(2) written exams. If after two (2) written exams, the student’s average is above 80%, the student will be removed from academic probation. If, however, the student’s average is still below 80%, the student faces dismissal from the program. The student must have a class average of 80% or better to be eligible to take any certification examination (i.e. EMT-P). Passing the course final with an 80% or better is also required to pass the course. Failure of the final exam constitutes failure of the course. The student must pass the mid-term written exam with an 80%
Page 10 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion or better and the midterm oral examinations (2 out of 3 scenarios). Arrangements to take exams or quizzes missed for excused reasons must be made within one week of the exam. Permission to miss the exam must be obtained from the Instructor prior to the scheduled exam time. Students who miss any exam will have 10% deducted from their score on the make-up exam.
Psychomotor/Skills Evaluation
Practical skills examinations will be graded on a pass/fail basis, where all skills must be passed for the student to pass the practical exam. The student must pass interim skills evaluations using the current criteria of the Florida State Department of Health to continue in the program. Should a student fail any interim practical skills evaluation, he/she will be allowed to re-test a total of three (3) times with appropriate remediation in between. Failure of the same skill four (4) times is grounds for dismissal from the program. The time limit to complete any specific component of a practical skills evaluation is 15 minutes, unless otherwise noted. Basic skills as well as newly acquired advanced skills will be evaluated throughout the program. Students will be counseled on areas in need of improvement and suggested strategies for improving performance.
While there are many ways to perform a procedure and perform it correctly, only those variants sanctioned by the Program Medical Director and/or the Lead Instructor will be acceptable.
Successful completion of the final practical exam is required to sit for the State Certification
Examination.
Successful completion of the final practical exam is required to graduate the program and sit for the State Certification Examination. The Medical Director shall have the duty to and responsibility for certifying that graduates have successfully completed all phases of the education program and are proficient in BLS techniques for EMT and BLS and ALS techniques for Paramedic.
Affective Evaluation
Continuous evaluations in these areas of professional behavior will include the following:
Integrity
Examples of professional behavior include but are not limited to consistent honesty, being able to be trusted with the property of others, can be trusted with confidential information, complete and accurate documentation of patient care and learning activities.
Empathy
Examples of professional behavior include but are not limited to: showing compassion for others; responding appropriately to the emotional response of patients and family members; demonstrating respect for others; demonstrating a calm, compassionate and helpful demeanor toward those in need; being supportive and reassuring to others.
Self-motivation
Examples of professional behavior include but are not limited to: taking initiative to complete assignments; taking initiative to improve and/or correct behavior; taking on and following through on tasks without constant supervision; showing enthusiasm for learning and improvement; consistently striving for excellence in all aspects of patient care and professional activities; accepting constructive feedback in a positive manner; and taking advantage of learning opportunities.
Page 11 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Appearance and Personal Hygiene
Examples of professional behavior include but are not limited to: clothing and uniform is appropriate, neat, clean and well maintained; good personal hygiene and personal grooming.
Self-confidence
Examples of professional behavior include but are not limited to: Demonstrating ability to trust personal judgment; Demonstrating an awareness of strengths and limitations; exercising good personal judgment.
Communications
Examples of professional behavior include, but are not limited to: speaking clearly; writing legibly; listening actively; adjusting communication strategies to various situations.
Time Management
Examples of professional behavior include, but are not limited to: consistent punctuality, completing tasks and assignments on time.
Teamwork and Diplomacy
Examples of professional behavior include, but are not limited to: placing the success of the team above self-interest; not undermining the team; helping and supporting others; showing respect for all team members; remaining flexible and open to change; communicating with others to resolve problems.
Respect
Examples of professional behavior include, but are not limited to: being polite to others; not using derogatory or demeaning terms; behaving in a manner that brings credit to the profession.
Patient Advocacy
Examples of professional behavior include, but are not limited to: not allowing personal bias or feelings to interfere with patient care; placing the needs of patients above selfinterest; protecting and respecting patient confidentiality and dignity.
Careful Delivery of Service
Examples of professional behavior include, but are not limited to: mastering and refreshing skills; performing complete equipment checks; demonstrating careful and safe ambulance operations; following policies, procedures and protocols; following orders.
These professional behaviors will be assessed during classroom activities and practical lab sessions, clinical rotations and field internship rotations. Interactions between the student and other students, instructors, preceptors, patients and others the student has contact/interactions with will form the basis for evaluation in this area.
Areas in need of improvement will be discussed with the student in counseling sessions.
Documentation will include the areas in need of improvement as well as corrective actions that need to be taken. Continued problems in this area may lead to dismissal from the program.
Page 12 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Grading Policy
Grades during the didactic phase will be determined based on the following:
A 94-100% Excellent
B 87- 93% Above Average
C
F
80- 86%
0 - 79%
Average
Failure
Homework is graded pass or fail. Homework (workbook) is due according to the course syllabus.
Homework is required to be turned in prior to being eligible to take an exam or quiz. At the end of the course, the cumulative score of all required homework assignments will be compiled and the grade will be used to replace the lowest exam score the student incurred. The minimum passing score for quizzes is 80%. If a student misses a quiz due to an absence, they must take the quiz the following class. If a student fails a quiz, he or she will continue to take a quiz until successfully passed. The original score will stand in the grading. Module exams are given for every section covered in the course syllabus including the midterm and final. Each student must maintain an average of 80% to successfully complete the program. Any missed module exam must be taken by the next scheduled class date, either before class begins or after class. No exams will be available during the lunch hour. Missed module exams are not acceptable.
Exceptions are made on a case-by-case basis; otherwise missed module exams will be penalized one letter grade for unexcused absences. Module exams may have a lab skills practical portion based on the skills covered in the curriculum. The skills are a pass/fail objective. Failed skills will constitute a failure for the exam and will follow the same procedures as if the written was failed. Mid-term or Final exam failure is grounds for dismissal without further evaluation for continuation or graduation from the course. Grades will be given during the next convening class date.
Incomplete Grade
A student who receives an “I” (incomplete) grade is one who has not completed the required work to maintain a satisfactory progress. He or she has two weeks to complete the work. If it is not completed, the student may receive an “F” (failure) for the course.
Standards of Satisfactory Progress
Student evaluation will consist of didactic and clinical portions. Clinical evaluations are covered in the clinical portion of the EMT/Paramedic handbook. Didactic evaluations consist of the written examinations (module exams) and quizzes and various other learning methods, i.e.
(presentations, projects, research papers). The Module exams will contain a variety of question types including multiple choice, true/false, matching, situational short answer, fill in the blank, and essay. The student will always be made aware of the objectives being tested for in each examination. Material covered on the Module exams and quizzes are derived from reading assignments, lecture material, handouts, practical skill sheets and any other material covered in the program. Students enrolled at Nature Coast Emergency Medical Institute must be making measurable academic progress towards completing of his or her program of study. The school has established satisfactory academic progress standard minimum of a cumulative grade point average of 80% (3.0 GPA).
Page 13 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Academic Probation
Failure of a student to meet academic or skill performance standards will result in remedial action to address educational strategies. Such corrective action may include additional course work in the form of oral presentations, written assignments, and one on one coaching by the peers or staff.
The student or lecturer instructor may initiate remediation. Inability to resolve academic or skill performance deficiencies with remedial work and after the instructional staff have exhausted all the available resources, the student will be reevaluated for continuation in the program.
Overall Course Completion
An EMT student has completed his or her EMT education at Nature Coast EMI when the student has met the following conditions:
All financial obligations have been met and all property of Nature Coast EMI has been returned
1.
An overall average of 80% or pass has been achieved in all courses.
2.
An overall “meets standards” has been achieved in all lab skills*.
3.
An overall satisfactory grade has been achieved in clinical rotation*.
4.
An acceptable final Externship Evaluation has been received from the preceptor.
5.
The medical director attests to course completion.
6.
Students are required to pass a comprehensive written with a score of 80% and a comprehensive practical exam in order to successfully complete the training program The
Medical Director shall have the duty of and responsibility for certifying graduates have successfully completed all phases of the education program and are proficient in BLS techniques. Successful completion of the final practical exam is required to sit for the
State Certification Examination.
*Recorded as a “Pass” on the course record.
Upon successful completion a students will receive a course completion diploma within 14 days.
A student who has completed a course of instruction as an EMT is eligible to test for certification as an EMT in the State of Florida through the National Registry of Emergency Medical
Technicians provided that they meet the conditions set forth by both Florida State’s Department of Health (Section 401, F.S.)
A paramedic student has completed his or her paramedic education at Nature Coast Emergency
Medical Institute when the student has met the following conditions:
All financial obligations have been met and all property of Nature Coast Emergency Medical
Institute has been returned
7.
An overall average of 80% or pass has been achieved in all courses.
8.
An overall “meets standards” has been achieved in all lab skills*.
9.
An overall satisfactory grade has been achieved in clinical rotation*.
10.
An acceptable final Externship Evaluation has been received from the preceptor.
11.
Student has completed all required objectives for the course, including by not limited to assignments, clinical rotations and externship assignments.
12.
The medical director attests to course completion.
Page 14 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
A student who has completed a course of instruction as a paramedic is eligible to test for certification as a paramedic in the State of Florida provided that they meet the conditions set forth by both Florida State’s Department of Health (Section 401, F.S.).
*Recorded as a “Pass” on the course record.
Conduct
Students are expected to behave in a mature and professional manner on all clinical rotations and adhere to the code of conduct as outlined below. Student will not be subjected to call or duty during the training program in accordance with Florida Administrative Code.
EMT Code of Ethics (NAEMT)
Professional status as an Emergency Medical Technician and Emergency Medical Technician-
Paramedic is maintained and enriched by the willingness of the individual practitioner to accept and fulfill obligations to society, other medical professionals, and the profession of Emergency
Medical Technician. As an Emergency Medical Technician-Paramedic, I solemnly pledge myself to the following code of professional ethics:
A fundamental responsibility of the Emergency Medical Technician is to conserve life, to alleviate suffering, to promote health, to do no harm, and to encourage the quality and equal availability of emergency medical care.
The Emergency Medical Technician provides services based on human need, with respect for human dignity, unrestricted by consideration of nationality, race creed, color, or status.
The Emergency Medical Technician does not use professional knowledge and skills in any enterprise detrimental to the public well-being.
The Emergency Medical Technician respects and holds in confidence all information of a confidential nature obtained in the course of professional work unless required by law to divulge such information.
The Emergency Medical Technician, as a citizen, understands and upholds the law and performs the duties of citizenship; as a professional, the Emergency Medical Technician has the neverending responsibility to work with concerned citizens and other health care professionals in promoting a high standard of emergency medical care to all people.
The Emergency Medical Technician shall maintain professional competence and demonstrate concern for the competence of other members of the Emergency Medical Services health care team.
An Emergency Medical Technician assumes responsibility in defining and upholding standards of professional practice and education.
The Emergency Medical Technician assumes responsibility for individual professional actions
Page 15 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion and judgment, both in dependent and independent emergency functions, and knows and upholds the laws, which affect the practice of the Emergency Medical Technician.
An Emergency Medical Technician has the responsibility to be aware of and participate in matters of legislation affecting the Emergency Medical Service System.
The Emergency Medical Technician, or groups of Emergency Medical Technicians, who advertise professional service, does so in conformity with the dignity of the profession.
The Emergency Medical Technician has an obligation to protect the public by not delegating to a person less qualified, any service which requires the professional competence of an Emergency
Medical Technician
The Emergency Medical Technician will work harmoniously with and sustain confidence in
Emergency Medical Technicians, the nurses, the physicians, and other members of the
Emergency Medical Services health care team.
The Emergency Medical Technician refuses to participate in unethical procedures, and assumes the responsibility to expose incompetence or unethical conduct of others to the appropriate authority in a proper and professional manner.
Attendance
A total of two (2) absences from classroom, lab, and clinical or field externship per phase of class may result in dismissal from the program. Extraordinary circumstances will be handled on a case-by-case basis by following established policies and procedures. Should a student be unable to attend a scheduled clinical rotation, (s) he must contact the Lead Instructor or the
Program Clinical Coordinator. If a student is unable to attend a scheduled clinical rotation and notifies the office twenty-four (24) hours or more in advance, (s) he will not be assessed with an absence. Notification received in less than 24 hours will result in an absence is recorded and a charge of $25.00 to the student.
Sick Call
Working while you are ill helps no one. You create the risk of making yourself more ill and infecting your assigned crew, hospital staff, and patients. While no one wants to miss class or a field clinical, you should call in sick if you have one or more of the following:
Fever >101 degrees.
Frequent productive cough.
Nausea and vomiting.
Diarrhea.
Any infectious disease (strep throat, chicken pox, etc.), unless you are cleared to return to duty by a physician.
Any condition where you feel your illness will disrupt the function of the class, crew
(needing to leave early after you arrive, etc.) or disruptive to patient care.
Page 16 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Notify the Lead Instructor or the Program Clinical Coordinator if you are calling in sick for a scheduled clinical, preferably at least 2 hours before the scheduled start of the clinical. If you are unable to reach the Lead Instructor or the Program Clinical Coordinator leave a voice-mail or email. Preceptors may dismiss a student from the classroom or clinical site if the student appears ill, and/or is unable to complete his/her duties due to illness.
Inclement Weather
Due to the extreme fluctuations in Florida weather and especially during hurricane season, prehospital care providers are often classified as “essential” personnel. This does not apply to students. In the event of inclement weather, local radio stations will broadcast closing of federal, state, county, and local government offices to "non- essential" personnel. If the clinical site orders "non-essential" employees to stay home, students should also stay home.
Nature Coast Emergency Medical Institute follows the direction of Citrus County Schools when establishing "closed due to weather” status. If inclement weather occurs while the student is on clinical, reasonable efforts will be made to allow the student to safely return home or to facilitate sheltering in place.
Student to Instructor Ratio
The usual class size is listed below. Nature Coast Emergency Medical Institute will provide one instructor for every six (1:6) students in the lab and skill evaluation training.
Paramedic
EMT-Basic or Online
Class Size:
Class Size:
24
30
ACLS/PALS
PEPP
ITLS
Class Size: 30
Class Size: 30
Class Size: 24
Absences from classroom
A student will be allowed no more than two (2) absences with prior consent. Absences above this limit will result in further evaluation of the student’s commitment, to the program and possible removal from the program. An absence with prior notification means that the student has contacted the proper authority (Lead Instructor) at least one (1) hour prior to the scheduled start of class. If the Lead Instructor cannot be contacted, then leave an email with the Lead Instructor.
It is appropriate to contact the school’s administration and leave the pertinent information. After one (1) unexcused absence, the student will meet with the Program Director and may be placed on academic probation. No tardiness or early exits will be tolerated. A tardy is defined as arriving to the class after the scheduled start time. An early exit is defined as leaving more than
30 minutes prior to the end of program. A student may be granted up to three (3) early exits or late attendance due to unforeseen events. Afterward, the student will meet with the Program
Director to discuss the issue and plan a course of action, to include make up of the missing hours and/or removal from the course. Students are responsible for the material covered in ALL scheduled classes. Subject material cannot always be written as notes during classes; therefore, it is crucial to attend each session
Page 17 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
A leave of absence has no effect on the student’s standards of progress but will extend the program completion time.
Absences during Lab Practical and/or specialty courses
If a student’s absence coincides with any required practical lab evaluations/testing or core courses (ACLS, Paramedic) it is the student’s responsibility to reschedule the missed event on their own time.
Make Up Work
Students, who miss assignments, quizzes, module exams or any other required work due to absences, tardiness, or early exits, must make-up the work. The responsibility to complete the missed work will require the students to schedule, the event on their own time. Missed quizzes, module exams must be taken within 5 days from the student’s return to class. Failure to complete the required exam/quiz in the required time will result in the grade of “Failure”.
Prohibited Conduct
Submitting assignments, exams or other academic work that were furnished by another for the purpose of aiding another person to cheat.
Falsification or misuse of Nature Coast Emergency Medical Institute records permits or documents.
Exhibiting behavior, which is disruptive to the learning process or the academic/clinical environment.
Conviction of a crime before or after becoming a student.
Attending any Nature Coast Emergency Medical Institute educational offerings under the influence of drugs and/or alcohol or any substance that may impair one’s ability to perform required functions. It is inappropriate to be under the influence or have consumed within the last twelve (12) hours of any substance that would alter your state of mind and jeopardize patient care. If the student is suspected to be under the influence, the student will be dismissed from class/clinical rotation immediately.
Obstruction or disruption of teaching, administration, disciplinary proceedings, or other institutional activities will not be tolerated.
Detention or physical threat or abuse of any person on any Nature Coast Emergency
Medical Institute owned controlled property.
Malicious damage, misuse or theft of Nature Coast Emergency Medical Institute property, or clinical site.
Possesses or uses a firearm, explosives, or dangerous chemicals or other dangerous substances/weapons on Nature Coast Emergency Medical Institute property or affiliated site.
Unauthorized entry to or use of Nature Coast Emergency Medical Institute equipment and/or facilities.
Use of Nature Coast Emergency Medical Institute computers for any activities involving down loading programs, including music/video files and accessing, internet sites containing pornographic content.
Page 18 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Any person(s) who witness or has firsthand knowledge of misconduct described above is obligated to report the infraction. Failure to do so may lead to disciplinary action to include dismissal from the program.
Cell phones, pagers or other electronic communication devices should be turned off during class and lab time.
Any damage to equipment that involves a student must be reported to the Program
Director immediately. The student who breaks or disfigures any Nature Coast
Emergency Medical Institute property may be held responsible for its replacement or repair cost.
School equipment and property are not to be removed from the building. A student wishing to use the equipment may do so by scheduling a lab period.
Nature Coast Emergency Medical Institute is a smoke free campus, no smoking is allowed on the property, or during any clinical/field rotation.
Patient Confidentiality
Students will comply with patient confidentiality guidelines established by the Health Insurance
Portability and Accountability (HIPPA) of 1996. Student clinical forms and patient care forms should not have the patient’s private information or any other distinguishable information.
Patient care is not to be discussed with anyone not directly involved in that patient’s direct care.
Further information on HIPPA can be found online as a link on the Nature Coast Emergency
Medical Services web site.
Dress Code
NCEMS issued uniforms are to be worn at all times during classroom, clinical, and field internships. You are expected to keep a neat and clean appearance that reflects professionalism.
Additional expectations include the following:
Students are expected to wear school uniform during all instruction hours.
Students are expected to wear the approved program shirt with I.D badge.
Women may not wear a skirt at any time.
Black closed-toed shoes are required, boots are recommended.
Sandals or multi-color sneakers are not permitted.
Underclothing may not be visible, particularly T-shirts with printing.
The nametag of the student must be clearly visible on the uniform shirt.
If clothing should become soiled during clinical, the student should change into spare clothes; students are encouraged to bring a change of clothes to clinical.
Personal items like wallets and purses should be secured. The Program takes no responsibility for personal items that are lost or stolen. Students are encouraged to only bring the minimum that is needed.
Jewelry must not interfere with patient care. In general, post earrings are acceptable, while hoop earrings and the like are unsafe and therefore unacceptable. Body piercings must not be visible.
A stethoscope will be in hand for clinical, classroom, and labs as part of the uniform.
Stethoscopes are not provided.
Page 19 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Simulation Lab and Equipment Policy/ Procedures
During handling of the SIM-MAN and all the other simulation mannequins by the students and instructors, they will be required to wear gloves to ensure the cleanliness of the mannequins.
No one is allowed to operate SIM-MAN or any of the other technology without oversight by the Lead Instructor or designated staff member.
Only instructors are authorized to spray any silicone on the mannequins when required.
No student will be allowed to participate with any simulation operation without first completing the simulation orientation. A specific form is signed upon completion and is filed in the student’s record.
Designated wipes are used to wipe down the equipment after the training is completed.
Note: No other cleaning material is to be used.
All equipment will be checked out for use by the assigned Lab Instructor and will be returned in way that the equipment was checked out.
Telephone
Students are not permitted to use the telephones in the Nature Coast Emergency Medical Institute offices without permission of the instructor. The use of cell phones and pagers is not permitted during class sessions, and all ringers and audible alerts shall be disabled during class activities.
Discipline Procedures
Students who are counseled for any infractions will have the incident documented on a Student
Counseling Form, which will be filed in the students record and a copy kept in the Program
Director’s master file for each class. Any student for whom a recommendation for discipline/dismissal is considered will have received ample notification of unsatisfactory work.
A student who is required to see the Program Director for disciplinary action will be notified in writing, either by email, or by personal letter. The note will contain the violation with a time and date to meet with the Program Director. The violation of student policy and procedure will be addressed within three (3) working days of notification. The Program Director, Lead Instructor and the student will attend the disciplinary meeting to review the incident. This review will include:
Policies and Procedure relevant to the violation.
The student’s signed statement of agreement to Nature Coast Emergency Medical
Institute policies.
Any counseling form and any other related documentation.
Students record including: attendance, GPA, skills proficiency.
Student rebuttal
Page 20 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
The Program Director will provide the student with a written statement of action within 5 working days from the meeting date. Students may appeal a decision, in writing within five (5) working days from the disciplinary meeting.
Administrative Withdrawals
All students are expected to maintain a satisfactory level of academic achievement, to conduct themselves as respectable professional adults and attend classes regularly. Nature Coast
Emergency Medical Institute reserves the right to dismiss any student who:
1.
Fails to maintain satisfactory academic progress.
2.
Exhibits conduct the administration deems detrimental to the individual, other students or the school.
3.
Failure to meet attendance requirements
4.
Failure to meet financial obligations prior to completion of the program.
Student Appeal
A student may appeal a disciplinary decision in writing. The letter should contain the reason the student feels that the decision was not reasonable. The letter is to be submitted to the Program
Director via email or mailed letter. The Program Director or his designee shall schedule to meet with the student and the review the issue. The decision of the Program Director is final and may not be appealed. A student who feels that the appeal was not satisfactorily met may refer their grievance to the:
Executive Director, Commission for Independent Education
325 West Gaines Street, Tallahassee, FL 32399, Phone: 888-224-6684.
Cancellation and Refund Policy
Should a student’s enrollment be terminated or cancelled for any reason, all refunds will be made according to the following refund schedule:
1.
Cancellation can be made in person.
2.
All monies will be refunded if the school does not accept the applicant or if the student cancels within three (3) business days after signing the enrollment agreement and making initial payment.
3.
Cancellation after the third (3rd) business day, but before the first class, will result in a refund of all monies paid, with the exception of the registration fee (not to exceed
$150.00).
4.
Cancellation after attendance has begun, but prior to 40% completion of the program, will result in a Pro rata refund computed on the number of hours completed to the total program hours.
5.
Cancellation after completing 40% of the program will result in no refund.
6.
Termination date: When calculating the refund due to a student, the last date of actual attendance by the student is used in the calculation unless earlier written notice was received.
7.
Refunds will be made within 30 days of termination of the student’s enrollment or receipt
Page 21 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion of a Cancellation Notice from the student.
Extended Enrollment Status
Students not achieving the minimum standards of satisfactory academic progress or who fail to meet the minimum standards at the end of the academic probationary period will be terminated from Nature Coast EMI. The student may attempt to apply for extended enrollment if there is another program that is no more that 2 weeks behind the previous program to attempt to earn eligibility for reentry. Students approved in the extended enrollment status will be charged the appropriate tuition and fees during this period. While in this extended enrollment period status, students must attempt to correct their academic deficiencies. The extended enrollment status must be completed within the required maximum time frame. The student and the Program
Director will agree to the conditions for the extended enrollment, in writing.
Reestablishing Eligibility for Reentry
To reestablish reentry, a student must be in good standing while out of school (no delinquent debts), participate in a review of academic weaknesses, develop a tutoring program (if available), and demonstrate desire and motivation to continue. Upon the approval of the Program Director and upon the consent of the Medical Director, the student will be placed on Academic probation at the time of reentry. The student must successfully complete course material previously failed or upgrade the skills applicable to the student’s educational objectives. If at the end of the term, if the student has demonstrated improvement to the required minimum, he or she will be removed from probation. If the student has not reached the minimum requirement, the student will be academically dismissed and will not be eligible for readmission.
Financial Aid
Nature Coast Emergency Medical Institute can provide only limited assistance with completing financial aid documentation.
Lost Property
Nature Coast Emergency Medical Institute does not assume responsibility for the loss of books or other personal property left at our facilities/on our equipment.
Academic Advising and Tutoring
Students may request to meet with the Lead Instructor and Program Director to discuss their academic concerns. Students may initiate the academic probation program for themselves.
Students, who are not meeting the standard, will be recommended for academic probation when required. Academic probation consists of further requirements to complete additional quizzes, research papers, and computer labs, mentoring with an assigned instructor. Students wanting to meet with their Lead and or Program Director may do so at the Education Office or by contacting the Lead Instructor or Program Director via email.
Page 22 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Resources- Facilities
Nature Coast Emergency Medical Institute will provide adequate classroom, labs and other facilities located at 3876 W Country Hill Drive, Lecanto, Florida. Two large classrooms/labs, library and education offices are located at this location. The Emergency Medical Learning
Resource Center online bookstore is one resource that is open twenty-four hours a day and carries the required texts and supplies for the various programs provided.
Parking
Parking is available free of charge at Nature Coast Emergency Medical Institute facilities.
Student Library
An onsite library is available for student use during normal business hours (8 am until 5 pm) and during class hours. Additional textbooks, videos, and professional journals will be available to students throughout the course. Reference and other non-circulating materials must be used in the library during normal business hours.
Discrimination
Nature Coast Emergency Medical Institute is dedicated to a non-discriminatory environment and does not discriminate based on race, age, color, religion, sex, national origin, ancestry, marital status, sexual preference, disability, or any other status protected by applicable law.
Student Advocacy
The Nature Coast Emergency Medical Institute Team will assist and support our students in any administrative, education, and/or clinical matters and strive to be advocates for our students.
Timely notification of any significant incident or problem is required and should be communicated to the Program Director.
Record Keeping
Nature Coast Emergency Medical Institute maintains all student records. These records are available to students and authorized agencies upon request. All student records and private financial information are kept secured in locked file cabinets with limited access.
Student Records contain the following:
Student Application
Immunization record
Current Physical Exam
Financial Statement
Copies of exams, quizzes, clinical skill sheets
Attendance
Disciplinary actions
Certifications
Page 23 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
An official transcript is provided to any student who requests one in writing. Confidentiality of student records is maintained according to the Family Education Rights and Privacy Act of 1974
(Buckley Amendment). Student records are kept electronically onsite permanently from course completion date.
Job Placement Assistance
Nature Coast Emergency Medical Institute will provide, when available, information pertaining to job fairs and employment in area prehospital care services. Nature Coast Emergency Medical
Institute does not and cannot guarantee employment to any student or graduate of our programs.
Indemnification
The student releases and holds harmless Nature Coast Emergency Medical Institute, its employees, its agents, and representatives from and against all liabilities, damages, and other expenses which may be imposed upon, incurred by, or asserted against it or them by reason of bodily injury or property damage which may be suffered by the student from any cause, while enrolled as a student in the institution. When students are permitted to participate in individual or group tests, training, or demonstration or ability, techniques, commodities, equipment or procedures relating to course or intramural activities under the auspices of the school, the student and parties executing the student enrollment contract, authorize participation by the student and releases the institution, and its officers, agents and employees from any and all responsibility for injury and damage to person or property.
Introduction to Paramedic Clinical
Clinical education represents the most important component of paramedic education since this is where the student learns to synthesize cognitive and psychomotor skills. To be effective, clinical education should integrate and reinforce the didactic and skills laboratory components of the program. Clinical instruction should follow sound educational principles, be logically sequenced to proceed from simple to complex tasks, have specific objectives, and be closely supervised and evaluated. Students should not arrive in the clinical environments with poorly planned activities; they should know what they must accomplish. This manual serves to provide that structure and a mechanism to track progress. The ability to serve in the capacity of an entry-level or novice paramedic requires experience with actual patients. This process enables the paramedic student to build a database of patient experiences that serves as a matrix to help in clinical decisionmaking and pattern recognition; i.e. building on experiences of the past to facilitate critical thinking skills. Time is no longer used as the criteria to determine the quantity of clinical education. More than any other phase of paramedic education, minimum amounts of patient contacts and frequency of skills performed must be established for clinical education. It is acceptable to use a time-based system to help in program planning, but a system must be used to assure that every student satisfies each and every clinical objective. To this end there is a minimum competency requirement for each clinical area, in both skills and patient categories, and for the entire clinical aspect of the paramedic program. Typically, clinical education for the paramedic takes place in both the hospital and field environments.
Page 24 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Tardiness for all clinical sites
Students are expected to arrive promptly for clinical. Failure to do so will result in the student being assessed a late arrival. Three late arrivals constitute an absence from clinical. It is a privilege to have preceptors to work with our students and we do not want to abuse this. If at any time a student has a problem with clinical scheduling, he/she should discuss the matter with the
Clinical Coordinator. Due to the unpredictable nature of emergency medical services, punctuality is important. Arriving on time is important for students. Showing up even a few minutes late may mean missing your mentor for up to several hours depending on call volume and unit availability. Most importantly it displays a lack of professionalism and commitment to the Paramedic Program. You are required to report for your shift 15 minutes prior to the start of shift. Chronic tardiness will affect your grade and standing in the paramedic program.
Unexcused absences/tardiness will not be tolerated. The field clinical instructor will determine whether an absence/lateness is excused.
The following action will be taken when a student is late or absent from a scheduled shift without excuse:
First Offense: Verbal Warning
Second Offense: Written Warning
Third Offense: Student, Instructor, and Program Director will meet to discuss and resolve the issue.
Fourth Offense: Action as determined by the Clinical Coordinator and Program
Director. This action may include dismissal from the paramedic program.
If you do find yourself in a situation where you will be late for a shift, you should first notify the
Lead Instructor or Clinical Coordinator by phone and if unsuccessful leave a message on voicemail or e-mail. Tardiness or absences that are not reported to the instructor in a timely manner will be considered unexcused. All episodes of tardiness and absence will be reported.
Paramedic Program Objectives and Description
OBJECTIVES:
1.
To develop in the graduate paramedic, an understanding of Emergency medical Systems and the practice of pre-hospital medicine as it applies to the roles and responsibilities of the Paramedic.
2.
To prepare the graduate Paramedic to provide quality care and to function competently and effectively in the pre-hospital system of healthcare. The graduate Paramedic will be able to demonstrate advanced skills and knowledge in his patient encounters.
3.
To prepare the graduate Paramedic to successfully complete the Florida State and/or
National Paramedic Certificate Examination.
To assist the graduate Paramedic in their understanding of the need to continue their education and be aware of the requirements of their certification/license.
Page 25 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
DESCRIPTION:
The Paramedic functions as the highest level of prehospital care provider in the prehospital care team. As a member of the allied health professions the paramedic is highly regarded by society and recognized in their role as an authority in prehospital medicine.
The primary role of the paramedic is to provide emergency medical care in an out-of-hospital environment. The paramedic will use their advanced training and equipment to extend the care of the emergency physician to the patient in the field. However, the paramedic will also need to use accurate independent judgment in the care and treatment of patients.
Students will be prepared to take the Florida State Paramedic exam and the National Registry of
EMTs Paramedic Certification.
Course
Number
PM201
Paramedic
•
•
•
•
Course Introduction and Overview
• Policies and Procedures
Review of the Student Manual
Course Objectives
Clinical Sites, Course breakdown, and Paperwork
Familiarize with Florida Statutes
PM202
PM 203
•
•
•
•
•
Introduction
• Introduction to Advanced Prehospital Care
Well-Being of the Paramedic
EMS Systems/Ethics in Advanced Care
Roles/Responsibilities of the Paramedics
Illness/Injury Prevention
Medical Legal in Prehospital Medicine
Four Hours HIV/AIDS Awareness
Medical Terminology
PM204
•
•
•
•
Anatomy & Physiology
• Cellular Physiology
Central Nervous System
The structure of the body systems
Pathophysiology
Practical skill labs as well as lectures.
Fluids and Shock
•
•
Types and functions of fluids
Types and effects of shock
• Management of patient during critical situation in prehospital setting
• Shock trauma management
IV skills
Medication administration skill
PM205 Introduction
•
•
Therapeutic Communications
Life Span Development
PM206 Pharmacology
•
•
•
•
Proper use, calculations and administration of medications
Use of these medications in the pre-hospital setting
Contraindications for use of medications
How to use injections needles and intravenous catheters
• Drug Calculation
IV infusions
Hours Location
4
7
71
60
3
47
Classroom
Classroom
Classroom
Classroom
Classroom
Classroom
Page 26 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Drug administration
PM207 Patient Assessment
•
•
•
Basic components of a complete health history
How to effectively conduct an interview
Communicating with difficult patient, hostile patients, and patients with language barriers
•
• and physical exams
•
•
•
Techniques of conducting a comprehensive physical exam
Practical approach to conducting problem-oriented history
Basic steps for making clinical decisions
How to think critically in emergency situations
Communications and Documentation
PM208 Respiratory and Airway
•
•
•
•
Respiratory System Management – Basic and Advance
Respiratory Emergencies
Review respiratory system
Nasal and end tracheal intubations
•
•
Rapid Sequence Intubations
Mechanical Ventilator Management
• Proper administration of medications that will help manage respiratory emergencies
• Practical skills and lecture
PM209 Cardiology
Review of Cardiovascular System
Arrhythmia Recognition and Treatment
AHA Advance Cardiac Life Support
12-lead EKG Interpretatio
•
•
•
•
PM210 Neurology
•
•
Review of the Nervous Systems
Recognition and Management of neurological emergencies
PM211 Endocrinology
•
•
Review of Endocrine System
Recognition and Management of endocrine emergencies, with emphasis on diabetic emergencies
PM212 Allergic Reaction and Anaphylaxis
•
•
Review of the Immune System
Recognition and Management of allergic reaction and anaphylactic reaction emergencies
PM213 Gastroenterology
•
•
Review of Gastrointestinal System
Recognition and Management of Gastrointestinal emergencies
PM214 Urology and Nephrology
•
•
Review of genitourinary System
Recognition and Management of the urinary system emergencies in males and females, and male reproductive systems emergencies
PM215 Toxicology and Substance Abuse
• Discuss basic toxicology and both common and uncommon cause of poisoning
• Discuss Overdose and Substance abuse, including drugs and
12
36
38
8
6
4
6
6
6
Classroom
Classroom
Classroom
Classroom
Classroom
Classroom
Classroom
Classroom
Classroom
Page 27 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion alcohol
• Discuss recognition and management of poisoning, overdose, and substance abuse emergencies
PM216 Hematology
• Discuss the anatomy, physiology. and pathophysiology of the blood-forming organs, organs, and the reticuloendothelial
• Recognition and Management of hematological emergencies
PM217 Environmental Emergencies
• Details the impact of the environment on the body, emphasizing physical, chemical , and biological aspects
• Recognition and Management of heat disorders, cold disorders, drowning and near-drowning emergencies, diving emergencies, high-altitude emergencies, and radiation emergencies
PM218 Infectious Disease
•
•
Addressess specific disease and modes of transmission
Emphasize prevention of disease transmission, especially the protection of prehospital personnel
• Recognition and Management of specific infectious disease
PM219 Psychiatric and Behavioral Disorders
• An Overview of psychiatric disorders and behavioral problems
• Recognition and Management of psychiatric and behavioral emergencies
PM220 Obstetrics and Gynecology
•
•
•
•
Discuss female reproductive system
Discuss the anatomy and physiology of pregnancy
How to assisst in the delivery of a newborn
Recognition and management of obstetric and gynecological emergencies
PM221 Neonatology and Pediatrics
•
•
Recognition of common clinical problems
AHA Pediatric Advance Life Support (PALS)
• Providing appropriate careand treatment for pediatric patients in an array of medical and trauma emergencies
• Two hour SIDS Training
PM222 Geriatrics
•
•
Review the anatomy and physiology
Discuss the assessment and treatment of emergencies commonly seen in the elderly
• Providing appropriate care
PM223 Trauma
•
• patient
•
Trauma management
Understand and recognize signs and symptoms of trauma in
Administer proper and vital treatment
Understanding the kinematics of trauma
State of Florida Trauma Alert Criteria
•
•
AEMT- Pre-hospital Trauma Life Support (PHTLS)
Two hours instruction in the trauma scorecard methodology
3
6
2
6
18
20
9
38
Classroom
Classroom
Classroom
Classroom
Classroom
Classroom
Classroom
Classroom
Page 28 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
PM224 Special Considerations/Operations
•
•
•
•
•
•
•
Abuse and Assault
The Challenged Patient
Management of the Central Line and PICC
Acute Interventions for the Chronic Care Patient
Assessment-Based Management
Ambulance Operations
Medical Incident Command
PM225 Special Considerations/Operations
•
•
•
•
•
•
Haz-Mat Awareness
Multiple Casualty Incident
Rural EMS
Crime Scene Awareness
Medical Incident Command
Responding to Terrorist Acts
PM226 Clinical Externship
•
•
•
•
•
PM227 PM213 - Field Externship
Emergency Department - 14 - 12 hour shifts
OB/GYN – 24 hours
ER Physician 12 hours
MIHP –Community Paramedic – 8 hours
Pediatric – 24 hours
• Advance Life Support Ambulance 31 12 hour shifts
( Capstone Phase 4 11 shifts )
LAB Laboratory SKILLS 25/7 hour labs
TOTAL:
9
10
236
372
175
1218
Paramedic Hospital Clinical Requirements
Classroom
Classroom
Clinical
Clinical
LAB
Because of the unpredictable nature of emergency medicine, the hospital environment offers two advantages in paramedic education: volume and specificity. In the hospital setting, the paramedic student can see many more patients than is possible in the field. This is a very important component in building up a “library” of patient care experiences to draw upon in clinical decision-making. The use of multiple departments within the hospital enables the student to see an adequate distribution of patient situations. In addition to emergency departments, which most closely approximate the types of patients that paramedics should see, clinical education should take advantage of critical care units, OB/GYN, operating rooms/anesthesia, recovery, pediatrics, psychiatric, etc. This will help assure a variety of patient presentations and complaints. These also provide a more holistic view of health care and an appreciation for the care that their patients will undergo throughout their recovery. This places emergency care within context.
Paramedic programs throughout the country have created clinical learning experiences in many environments. There is application to emergency medical care in almost any patient care setting,
Nature Coast Emergency Medical Institute is constantly seeking out and soliciting new clinical experiences for its students. Students are expected to perform assessments and skills on patients, following the standards taught in class. Students are furthermore expected to document those assessments and skills utilizing the documentation standards distributed in class. Finally, the student is expected to electronically enter the documentation of patient assessments for review and comment.
Page 29 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
During the hospital clinical, the student can expect the clinical adjunct to orient the student to the unit and to the hospital, and introduce the student to the staff. The student can expect the clinical preceptor to ask the student to demonstrate his or her skills, venipuncture for example.
Paramedic students may only perform those skills that they have successfully passed in during lab. All skills performed by students in the hospital must first be demonstrated to adjunct faculty member in lab who can attest that the student has achieved minimal competency at said skill.
During the hospital clinical, the student can expect to meet the Clinical Coordinator and give a
“verbal report” of his or her assessments, presumptive diagnosis and possible treatment. The
Clinical Coordinator will treat these verbal reports like a radio report to medical control and ask questions of the student about the patient, the assessment findings, the condition and/or the treatment. In the hospital clinical, the student is expected to submit his or her documentation of patient assessments electronically and/or to the Clinical Coordinator. The Clinical Coordinator, using regional quality improvement standards, will review the documentation. The Clinical
Coordinator then will return the documentation to the student with comments.
It is the responsibility of the student to enter all assessments and skills performed in the field or in the hospital into patient care reports and turned in within one week (7 days) of the completion of rotation.
Clinical Goals
Nature Coast Emergency Medical Institute has established several goals for our paramedic students during clinical:
An educated paramedic should be exposed to a broad variety of patient care environments (clinic, emergency, in-patient, aero-medical, pre-hospital, home healthcare, and wilderness.)
An educated paramedic should have achieved a sufficient depth of knowledge to be said to be competent as a novice paramedic provider.
An educated paramedic should be able to express him or herself clearly, completely, and accurately in all forms of communications, written, printed, or spoken.
An educated paramedic should be able to relate computational skills to the practice of medicine in the field.
An educated paramedic should be able to identify problems during clinical and to find efficient solutions to similar problems found in the field.
An educated paramedic should develop the skills to understand, accept, and relate to people of different backgrounds and beliefs.
An educated paramedic should be expected to have some understanding of and experience in thinking about moral and ethical problems.
Page 30 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
An educated paramedic should have conceptual ability: i.e. the ability to think rationally, to develop informed opinions, and to comprehend new ideas.
Although specific clinical objectives will vary from unit to unit, there are general considerations, which apply to all student activities while in the clinical areas. These include the ability to:
1. Accurately relate patient complaints to pathophysiology or pharmacologic effects, and to discuss appropriate therapeutic interventions based on the patient’s condition and diagnosis.
2. Obtain patient history from the patient or his/her chart in a systematic fashion.
3. Conduct a thorough and appropriate patient assessment noting signs, symptoms, and other pertinent findings.
4. Describe the anticipated effects of therapeutic interventions, including possible side effects and untoward reactions.
5. Safely and appropriately perform all skills listed on the clinical checklist of psychomotor skills as permitted.
6. Explain procedures to the patient in a manner in which the patient can understand.
7. Demonstrate professional behavior and genuine concern whenever dealing with patients, family, or other staff members.
8. Accurately and concisely document assessment findings and therapeutic interventions.
Hospital Preceptor
The Hospital Preceptor is a member of the hospital staff that has agreed to help Paramedic students gain a more meaningful experience. These Hospital Preceptors may be Registered
Nurses, Physician Assistants, Advanced Nurse Providers (i.e. Nurse Midwife) or even Physicians
(Attending Physicians and Residents).
The Hospital Preceptor’s primary responsibility is to their patients and to their employer and it is a privilege for a Paramedic Student to be permitted to participate in patient care. While teaching is an important aspect of professional conduct, there are times when patient care takes priority and the Paramedic Student is asked to step aside or even leave the unit.
Student Responsibilities
Be prompt in reporting for scheduled rotations. If a student knows that he/she will be late for a given rotation, then they must contact the Clinical Coordinator and/or
Lead Instructor. Please leave a message with your name, class, the clinical you are attending and the reason you are late.
Page 31 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Review the rules and operating procedures of the given unit with the clinical adjunct instructor at the beginning of the rotation. This will help clarify the student’s role in the unit.
Review clinical objectives for the rotation with the hospital preceptor, and discuss those activities and skills that the student may perform under the supervision of the hospital preceptor. Students may only perform those skills for which they have been properly trained and authorized by the Program Medical Director and signed off on the lab skills performance sheet. The student must have the lab skills performance sheet with them at all times.
Observe and participate in unit activities as directed by the hospital preceptor. The student should remember that the more willing he/she is to assist, the more likely they would be asked to participate.
Review relevant patient records to review the patient’s past medical history, physician’s/nurse’s assessments, diagnosis and in-hospital care. It must be clearly understood that all information contained in a patient’s record must remain confidential. Violation of this confidentiality will result in dismissal from the program.
Complete all documentation required for each clinical rotation. The student must have all required forms completed and signed at the end of the particular rotation.
Unexcused missed clinical will not be tolerated.
Location of Clinical
All clinical experiences will be obtained at those locations approved by Nature Coast Emergency
Medical Institute. Eight (8) to twelve (12) hours of clinical experiences are scheduled each week. The clinical rotations will begin immediately and conclude two weeks prior to the end of class.
Clinical Assignment
Once a student has been scheduled for a clinical rotation, the responsibility rests with him/her for satisfying the clinical rotation. Students are scheduled for a clinical rotation by the Program
Director or a designate (the Clinical Coordinator). Unless otherwise noted, students may request dates via the online clinical schedule himself/herself for any clinical rotation, but may not attend a clinical rotation until approved.
No more than two students are scheduled in one clinical area at a time. Students will stay with their designated preceptor in the assigned clinical unit. Students may not float to other clinical areas without permission of the clinical adjunct. Preceptors are assigned to students in many of the areas. In other units, the resident physician will serve as the preceptor/supervisor. Students may be permitted to assist other unit staff members with various activities at the discretion of their Clinical Preceptor.
Page 32 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
When you arrive on the unit, introduce yourself to the charge nurse. Inform the charge nurse of the length of time that you will be on the unit and show him/her your clinical check sheet. Ask to meet with your preceptor.
Health Assessment
Before any patient contact, every student is expected to have a health assessment completed and on-file. The pre-clinical health assessment includes a record of current immunizations as well as laboratory work. The health assessment ensures that our patient’s are protected as well as the student or faculty. The cost of the health assessment is the student’s responsibility. The health assessment must be completed on the form provided by the school and submitted before any patient contact is allowed. Students are strongly encouraged to get the flu shot, and must wear protective mask with patient care if they cannot provide documentation of a flu shot annually.
Physical Forms for Health Status
Physical exam reports must be turned in no later than the end of the first week of class or the student may NOT begin his/her clinical rotations. These forms are turned in to the Clinical
Coordinator.
Health and Liability Insurance
While as a student at Nature Coast EMS’s Paramedic Program, the student is covered by a general liability policy for acts committed in the course of their instruction as a student. Students are encouraged to consider obtaining additional malpractice insurance at minimal cost that is available from a number of insurance companies. For more information, please contact the program director.
While health insurance is not mandatory, it is highly recommended. Students are responsible for all expenses associated with healthcare while a student including but not limited to needle stick incidents, falls, and other illness/injuries that might occur in the course of the class.
Clinical Attire
Students are expected to wear appropriate attire for clinical.
Students are expected to wear the approved program shirt with I.D badge.
Women may not wear a skirt at any time during the clinical period.
Black closed-toed shoes are required.
Sandals or multi-color sneakers are not permitted.
Underclothing may not be visible, particularly T-shirts with printing.
The nametag of the student must be clearly visible on the uniform shirt.
If clothing should become soiled during clinical, the student should change into spare clothes; students are encouraged to bring a change of clothes to clinical.
Personal items like wallets and purses should be secured. The Program takes no responsibility for personal items that are lost or stolen. Students are encouraged to only bring the minimum that is needed.
Page 33 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Jewelry must not interfere with patient care. In general, post earrings are acceptable, while hoop earrings and the like are unsafe and therefore unacceptable. Body piercings must not be visible.
Special Unit Attire
Students will do rotations on special units such as the operating room and childbirth center may have special uniform requirements. Students are expected to comply with the unit’s dress policy.
Clothes are to be left in lockers provided by the unit. Students are reminded not to leave valuables in those lockers.
Infection Control
Students must wear personal protective equipment any time they are in contact with a patient
(i.e. practice standard precautions). The following rules must be adhered to at all times:
1.
Exposure to blood should be minimized. When the possibility of exposure to blood or other body fluid exists, gloves are recommended. During extrication, or when broken glass is present, leather gloves or fire fighter gloves should be used. If hands accidentally become contaminated with blood, they should be washed thoroughly as soon as possible.
When there is a risk of eye or mouth contamination (for example, the patient is vomiting bloody material or there is arterial bleeding), protective eyewear and masks are recommended.
2.
Needles and other sharp objects should be considered as potentially infective and be handled with extraordinary care. Needles should not be recapped. If it is necessary to recap a needle, use the appropriate technique (shoe holding the cap to the floor).
Needles, syringes and broken vials should be immediately placed in a puncture-proof
“sharps” container after use.
3.
Pocket masks with one-way valves or bag valve masks should be used for artificial respiration.
4.
Masks should be worn by the EMT or patient for those infectious agents known to be transmitted by the airborne route (i.e., tuberculosis, chicken pox, measles, etc.).
Sufficient information should be obtained to determine the presence of respiratory illness.
5.
Equipment should be thoroughly cleaned after each use. Disposable equipment should be considered for use whenever appropriate.
In the event of significant exposure, an instructor should be notified and an incident report filed.
Significant exposure is defined as the following:
Any puncture of the skin by a needle or other sharp object that has had contact with patient’s blood or body fluids or with fluids infused into the patient.
Blood spattered onto mucous membranes (e.g. mouth) or eyes.
Contamination of open skin (cuts, abrasions, blisters, open dermatitis) with blood, vomit, saliva, amniotic fluid or urine. A bite wound to providers would be included in this category.
Page 34 of 60
Conflict of Interest
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
To prevent the potential for a claim of conflict of interest students are not allowed to perform clinical rotations in the hospital units in which they are employed, or have relatives/significant others’ as clinical adjuncts, hospital preceptors, Preceptors or field preceptors.
Clinical Scheduling Policies
Each student will request to be scheduled for clinical rotations based upon his or her work schedule and rotation request. Unless otherwise noted, all scheduling is accomplished via electronic program. Final scheduling rests with the Program Director or designates (Clinical
Coordinator).
AT NO TIME IS A STUDENT TO ARRANGE HIS/HER OWN CLINICAL ROTATIONS.
Failure to comply will result in disciplinary action and may result in dismissal from the program.
Cancellation of clinical rotations due to illness or injury must be made at least one (1) hour in advance of the scheduled rotation. Failure to comply will result in disciplinary review and may result in dismissal from the program. In case of emergency, advance notification may be waived.
Please note that all time missed from clinical shifts, regardless of reason, must be made up.
Paramedic Clinical Skills
Skills may be performed only if:
1.
You have received instruction in the classroom and/or practical sessions
2.
You have observed the skill
3.
You are under the direct supervision of the preceptor or designated individual
4.
The skill falls within the realm of paramedic practice
5.
If administering medications, the medication is one with which you are familiar or you have had time to research thoroughly (through available resources on the unit) medication parameters including actions, indications, contraindications, side effects, and dosages.
The student will honor requests for assistance from the hospital staff while on rotation in a clinical area only if he or she has been trained and is competent to perform the task. The Clinical
Coordinator should be notified if any questions or conflicts arise. Needles, syringes, IV materials, or any other medical supplies will not be removed from the clinical area or skills laboratories. You are not expected to sit idly through your clinical rotation without the ability to practice. You will get out of the clinical rotations only what you put into them. Every effort should be made to avoid conflicts with the staff during the clinical rotations. Telephone calls will be limited to emergency calls ONLY. No personal calls are to be made while in the clinical area.
Regulation and Control
Failure to abide by the above listed rules may result in the student be asked to leave Clinical or
Externship by the hospital preceptor, clinical adjunct, Preceptor, or the externship preceptor.
Ejection will result in an absence recorded in attendance. Students may be asked to leave a unit
Page 35 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion or agency at any time by a member of the staff of the facility or agency. The student shall immediately comply, without comment, with the request and report the situation to the clinical coordinator.
Clinical Evaluations
Students can expect periodic evaluations about their clinical. These evaluations are intended to inform the student of their progress or lack of progress. When a student does not progress, then the adjunct faculty member will develop a plan of remediation, and the student will be asked to comply. If the student continues to not progress then a report shall be made to the clinical coordinator and a plan of action discussed with the medical director and the program director.
There is an interim clinical evaluation that is completed by the clinical faculty at the mid-point of the clinical. This mid-term evaluation must be completed and submitted to the clinical coordinator during the Mid-term examination. The final clinical evaluation is completed by the clinical faculty, and by the Preceptor. The final clinical evaluation attests that the student has achieved minimal competency at paramedic skills, radio report (verbal report) and documentation. The final clinical evaluation must be submitted to the clinical coordinator during the final examination. The student is expected to submit copies of all documented patient assessments as well as the final clinical evaluation to the clinical coordinator at the end of that clinical.
Completion of Clinical
Any student not completing their clinical requirements for the phase by the beginning of Finals
Week for that respective phase will be given a grade of incomplete for the section. Any student receiving a grade of “incomplete” must meet with the Clinical Coordinator prior to the end of the semester to resolve the matter. The Clinical Coordinator, in consultation with the Program
Director, may allow up to thirty (30) days for the student to complete the clinical requirements.
Students not completing the clinical requirements during the thirty-day extension will receive a grade of “Fail” for the semester and may not enroll in the next semester Paramedic Program classes.
Clinical Areas
Required forms for each rotation:
1.
Clinical Skills Checklist
2.
Patient Assessment Form
3.
ECG Mounting Form as needed
4.
Daily Hospital Clinical Evaluation Form
5.
Mid-Clinical and Final Clinical Evaluation Forms as necessary.
Paramedic Field Clinical
It is unreasonable to expect students to derive benefit from being placed into a field environment and performing. Field clinical rotations represent the phase of instruction where the student learns how to apply cognitive knowledge and the skills developed in skills laboratory and
Page 36 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion hospital clinical to the field environment. In most cases, field clinical should be held concurrently with didactic and hospital clinical instruction.
In this program, the field rotation experience begins early in class and continues through until the end of the program. The major concentration for the field clinical rotation begins in the 3rd phase, when the bulk of didactic and laboratory instruction has been completed and the student has sound knowledge and skills based on both laboratory and in-hospital clinical experience.
Field instruction, as well as hospital clinical, follows a logical progression. In general, students progress from observer to participant to team leader.
The amount of time that a student will have to spend in each phase will be variable and depend on many individual factors. One of the largest factors will be the amount and quality of previous emergency care experience.
With the trend toward less and less EMT experience prior to paramedic education, the amount of field experience may be adjusted to the experience of the students. Clinical affiliations are established and confirmed in written affiliation agreements with institutions and agencies that provide clinical experience under appropriate medical direction and clinical supervision.
Students should have access to patients who present common problems and be encouraged in the delivery of advanced emergency medicine. All paramedic students will be supervised on clinical rotations by the clinical preceptor and shall not be in the patient compartment alone during transport. Students shall not be used to meet staffing requirements. The contact person for each site will be responsible for assigning students to a preceptor for the rotation. Supervision will be done in accordance with Florida Administrative Code.
Externship Preceptor
The Externship Preceptor is an experienced Paramedic who evaluates the Paramedic Student’s preparation and makes a determination as to the Paramedic Student’s fitness to perform as a minimally competent entry-level Paramedic. The Externship Preceptors final evaluation is the final hurdle that every Paramedic Student must clear in order to be eligible to test for the State and/or National Registry Paramedic Examination for Paramedics.
Observation Phase I
The first phase of field clinical is observation. The student is expected to be become familiar with the policies, procedures and routines of the internship unit and provide any skills
(BLS/ALS) that the student is cleared to perform during this phase. The observation phase allows the student to become accustomed to his or her Preceptor and the unit. The duration of the observation period is left to the discretion of the Clinical Coordinator. The student is required to successfully complete the required hours within the allotted period on specific skills and knowledge in order to advance to the next phase. All skills performed by students in the field must be first demonstrated to an adjunct faculty member in lab who can attest that the student has achieved minimal competency at said skill.
Page 37 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Will perform BLS assessments and BLS skills. The student may suggest ALS therapy, as well as function as the ALS technician. The Preceptor will introduce the student at the various receiving facilities.
Will demonstrate the ability to locate and operate all BLS and ALS equipment.
Will demonstrate the ability to perform a BLS assessment.
Will provide BLS interventions to include definitive and supportive measures
Will make ALS treatment suggestions to the Preceptor.
Will function as the ALS technician for the Preceptor or team leader.
Participation Phase II
The second phase is the participation phase. During the participation phase, the paramedic student is expected to perform assessments and skills as directed by his or her
Preceptor/Preceptor. A paramedic student should have a paramedic Preceptor during this phase and should be performing ALS skills under supervision during hospital clinical.
Paramedic students may only perform those skills that they have been passed in during lab. All skills performed by students in the field must be first demonstrated to an adjunct faculty member in lab who can attest that the student has achieved minimal competency at said skill.
The preceptor will give the student hands-on experience in performing physical exams and vital signs.
May decide what ALS therapy is appropriate. Emphasis should be placed on patient contact and patient needs.
Will perform a head-to-toe exam on all patients encountered.
Will assess vital signs for all patients.
Will decide the appropriate ALS therapy.
Will function as the ALS technician.
Will gather a patient's history, decide and delegate BLS & ALS therapy.
Will gather the patient's chief complaint.
Will use mnemonics to support the history (PQRST, AMPLE, AEIOU TIPS).
Will complete the Patient Care Report (PCR) on all patients.
Will decide and delegate the appropriate ALS therapy, based on the history gathered.
Externship Phase III (Leadership phase)
After learning how to perform assessments and skills, and is able to manage a patient on an EMS call, the student moves into the final Externship phase. An Extern, by definition, is able to perform the assessments and skills of a paramedic but can also lead a team of pre-hospital professionals towards a goal.
Once a student has completed all skills competency in clinical and has completed a specific patient complaint classification then the paramedic preceptor may elect to allow the student to start his or her Externship. Students are only allowed to lead those emergency calls at the level of clinical completion. For example, when the student has completed the patient complaint category “chest pain” then he or she may start leading “chest pain” emergency calls in the field as a part of the Externship.
Page 38 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
The student in this phase:
Will take a more active role in field management.
Will perform the entire patient assessment.
Will delegate ALS therapy.
Will make radio contact to the hospital.
Will provide scene control.
During clinical rotations, each student should perform all required skills and assessments on human patients whenever possible. However, due to limited opportunity for these skills, they may be performed on simulation manikins in the skills lab. Whether in a clinical or lab setting, each skill must be observed and documented by an authorized preceptor.
If a student does not complete the phase requirements in full and in the allotted time, they will not be able to continue on to the next phase or continue with their assigned clinical rotations.
Agency Assignment
Students are assigned to field clinical based on unit availability, Preceptor availability and unit call volume. All ambulance field clinical experiences are with Nature Coast EMS. If a student wishes to do field clinical with another pre-hospital care provider, an affiliation agreement with
Nature Coast Emergency Medical Institute must be on file before the student can begin any field clinical or Externship.
Preceptor Assignment
Preceptors and Externship Preceptors are the backbone of any paramedic’s education. They represent the profession as well as their agency. To be acceptable as a Preceptor, during the observation and participation phase, the Preceptor has to be an on-line Paramedic with at least one year’s experience. To be acceptable as a Paramedic Preceptor, during the Externship phase, the Paramedic Preceptor must be an on-line Paramedic with at least one year’s experience. In all cases, the Preceptor or the Paramedic Preceptor must be acceptable to the paramedic program’s medical director. Other conditions, demanded by the field agency, may also apply.
Field Clinical Uniform
The standard Nature Coast Emergency Medical Institute approved student uniform will be required. The Nature Coast Emergency Medical Institute must approve coats and warm weather clothing.
Scheduling (Hours/Reporting)
Students are responsible for scheduling field Clinical with the Clinical Coordinator. During each phase of the program, students must complete a minimum number of clinical hours. Students should obtain the Clinical Coordinator’s schedule and discuss what shifts are open for the student to attend. The student must turn in a schedule of their shifts for each phase before the end of the second week of classes.
Page 39 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
The Clinical Coordinator must approve schedules. The Clinical Coordinator must approve any changes one week in advance. It is strongly discouraged for students to make any changes to their schedule once it is filed. Any changes must be submitted in writing to the Clinical
Coordinator with a detailed description of the reason for the change.
The following objectives must be successfully accomplished within the context of the clinical environment. Clinical experiences should occur after the student has demonstrated competence in skills and knowledge in the didactic and laboratory components of the course. Items in bold are essentials and must be completed. Items in italics are recommendations to achieve the essential and should be performed on actual patients in a clinical setting. Recommendations are not the only way to achieve the essential.
If the program is unable to achieve the recommendations on live patients, alternative learning experiences (simulations, programmed patient scenarios, etc.) can be developed. If alternatives to live patient contact are used, the program should increases in the number of times the skill must be performed to demonstrate competence. These recommendations are based on survey data from Paramedic Program Directors and expert opinion. Programs are encouraged to adjust these recommendations based on thorough program evaluation. For example, if the program finds that graduates perform poorly in airway management skills, they should increase the number of intubations and ventilations required for graduation and monitor the results.
Psychomotor Skills
1.
The student must demonstrate the ability to safely administer medications.
2.
The student should safely, and while performing all steps of each procedure, properly administer medications at least 15 times to live patients.
3.
The student must demonstrate the ability to safely perform endotracheal intubation.
4.
The student should safely, and while performing all steps of each procedure, successfully intubate at least 5 live patients.
5.
The student must demonstrate the ability to safely gain venous access in all age group patients.
6.
The student should safely, and while performing all steps of each procedure, successfully access the venous circulation at least 25 times on live patients of various age groups.
7.
The student must demonstrate the ability to effectively ventilate non-intubated patients of all age groups.
8.
The student should effectively, and while performing all steps of each procedure, ventilate at least 20 live patients of various age groups.
9.
The student must demonstrate the ability to perform a comprehensive assessment on pediatric patients.
10.
The student should perform a comprehensive patient assessment on at least 30 (including newborns, infants, toddlers, and school age) pediatric patients.
11.
The student must demonstrate the ability to perform a compressive assessment on adult patients.
12.
The student should perform a comprehensive patient assessment on at least 50 adult patients.
Page 40 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
13.
The student must demonstrate the ability to perform a comprehensive assessment on geriatric patients.
14.
The student should perform a comprehensive patient assessment on at least 30 geriatric patients.
PATHOLOGIES
1.
The student must demonstrate the ability to perform a comprehensive assessment on obstetric patients.
2.
The student should perform a comprehensive patient assessment on at least 10 obstetric patients.
3.
The student must demonstrate the ability to perform a comprehensive assessment on trauma patients.
4.
The student should perform a comprehensive patient assessment on at least 40 trauma patients.
5.
The student should perform a comprehensive patient assessment on at least 20 psychiatric patients.
COMPLAINTS
1.
The student must demonstrate the ability to perform a comprehensive assessment, formulate and implement a treatment plan for patients with chest pain.
2.
The student should perform a comprehensive patient assessment, formulate and implement a treatment plan on at least 30 patients with chest pain.
3.
The student should perform a comprehensive patient assessment, formulate and implement a treatment plan on at least 20 adult patients with dyspnea/respiratory distress.
4.
The student should perform a comprehensive patient assessment, formulate and implement a treatment plan on at least 8 pediatric patients (including infants, toddlers, and school age) with dyspnea/respiratory distress.
5.
The student should perform a comprehensive patient assessment, formulate and implement a treatment plan on at least 10 patients with syncope.
6.
The student should perform a comprehensive patient assessment, formulate and implement a treatment plan on at least 20 patients with abdominal complaints (for example: abdominal pain, nausea/vomiting, GI bleeding, gynecological complaint, etc.)
7.
The student should perform a comprehensive patient assessment, formulate and implement a treatment plan on at least 20 patients with altered mental status.
Paramedic Field Clinical Requirements
1.
The student must demonstrate the ability to serve as a team leader in variety of prehospital emergency situations.
2.
The student should serve as the team leader for at least 50 pre-hospital emergency responses.
The following checklist is to be completed at the end Phase III:
1.
Patient Assessments Thirty (30)
Page 41 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
2.
Chief Complaint - Chest Pain
3.
Chief Complaint - Shortness of Breath
4.
Chief Complaint - Trauma Twenty (20)
5.
Chief Complaint - Altered Mental Status Ten (10)
6.
Chief Complaint - Obstetric
7.
Chief Complaint - Psychiatric
8.
Chief Complaint - Syncope
Twenty (20)
Forty (40)
Twenty (20)
Ten (10)
Twenty (20)
9.
Team Leader
10.
Chief Complaint - Abdominal Pain
Fifty (50)
Ten (10)
11.
Psychomotor Skills Counts a.
Five (5) Successful Live Intubations (field or hospital). b.
Successfully has performed a minimum of 25 IV’s. Five (5) will be pediatric of various ages and (5) will be geriatric. c.
Successfully has performed a minimum of 15 Medication Administrations via
(IM, Sub-Q, Ett, Neb, Rectal or IV push.) d.
Collect four (4) EKG strips from your clinical experience each shift, post and complete the requested information
EMT Program Objectives and Program Description
OBJECTIVES:
Comprehend, apply and evaluate clinical information relevant to the role of an Emergency
Medical Technician. This will be accomplished by a comprehensive course exam and skills practical, as well as the State Exam. Nature Coast Emergency Medical Institute will maintain a student to instructor ratio of 6:1 on all skill lab days.
Demonstrate technical proficiency in all medical skills necessary to fulfill the role of entry level
Emergency Medical Technician. This evaluation will be completed by a final comprehensive exam, hospital clinical rotations and field externship evaluation. Demonstrate personal behaviors consistent with professional and employer expectation for the Emergency Medical Technician.
Upon successful completion of all the requirements, the student will have met the State of
Florida minimum requirements to take the State certification exam. The following objectives have been established and meet the requirements that are mandated by the State of Florida and the National Registry of Emergency Medical Technicians:
1.
The EMT student will be trained to be a minimally competent pre-hospital care provider able to be a productive member of the EMS/Allied health career field.
The EMT student will learn to handle most BLS medical emergencies via in depth didactic lecture and intensive hands-on lab practical.
DESCRIPTION:
Emergency Medical Technician has training in basic emergency care skills, including automated external defibrillation, use of airway adjuncts, and assisting patient with certain medications. The
EMT course covers a great deal of information and introduces many skills.
The EMT course will include four types of learning activities.
1. Reading assignments from the textbook and presentations and discussions held in class will provide you with the necessary knowledge base.
Page 42 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
2. Step-by-step demonstrations will teach the EMT student hands-on skills that the student will then practice in supervised small groups workshops.
3. Summary skills worksheets will help you to appropriately apply the sequence of steps in complex skills that contain a large number of steps or variations so that you can practice and perform the skill with no error or omission.
4. Case presentations and scenarios used in class will help you apply the knowledge and skills acquired in class, lab and clinical environments.
Page 43 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Course
Number
EMC101/
2
EMC103
EMT PROGRAM (Clock Hours 250)
Course Title
Introduction to Emergency Medical care
The Well-being of the EMT
Lifting and Moving Patients
Medical, Legal, and Ethical issues
Medical Terminology and Anatomy and Physiology
Principles of Pathophysiology
Life Span Development
HIV/AIDS 4 hours
Section 401, Florida Statutes, and Chapter 64J-1, Florida
Administrative Code, which governs emergency medical services in Florida.
The student will learn about medical and legal issues surrounding the emergency medical services field. How to take patient vital signs, obtain relevant history concerning the present and any recent illnesses or recent injuries. This is presented through lecture and practical skill sessions. A four hour (State required) HIV/AIDS program is presented to the student to familiarize them with infection control issues and practices.
Airway Management
Respiration and Artificial Ventilation
Extensive hands-on training and practice with basic airway management techniques and equipment.
Proper training on assisting with ALS procedures.
The student will learn the importance of obtaining and maintaining a patent airway in all types of patients. The student will become familiar with various airway management equipment and techniques. Students will be able to recognize the signs and symptoms of respiratory distress. The student will also become familiar in assisting the EMT or other ALS personnel in prepping advanced airway equipment.
EMC104 Patient Assessment
Scene Size up
The Primary Assessment
Vital Signs and Monitoring Devices
Assessment of the Trauma Patient
Assessment of the Medical Patient
Reassessment
Critical Thinking and Decision Making
Communication and Documentation
Emphasis will be placed on accurate and thorough patient assessment. The student will be required to conduct the proper assessment based on the patient’s condition and provide the appropriate care indicated.
Clock
Hours
14
4
18
Page 44 of 60
Credit
Hours
Location
Classroom
Classroom
Classroom
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
EMC105 Medical Emergencies
General Pharmacology
Respiratory Emergencies
Cardiac Emergencies
Diabetic Emergencies and Altered Mental Status
Allergic Reaction
Poisoning and Overdose Emergencies
Abdominal Emergencies
Behavioral and Psychiatric Emergencies and Suicides
Hematologic and Renal Emergencies
EMC106 Trauma Emergencies
Bleeding and Shock
Soft Tissue Trauma
Chest and Abdominal Trauma
Musculoskeletal Trauma
Trauma to the Head, Neck, and Spine
Multisystem Trauma
Environmental Emergencies
Trauma scorecard methodology (2 hours)
EMC107/
8
Pediatric /Geriatric
Obstetric and Gynecologic Emergencies
Pediatric Emergencies
Geriatric Emergencies
Emergencies for Patients with Special Challenges
Infant and children with medical emergencies can be a challenging and emotional scene to manage. This chapter covers the different anatomy of pediatrics and the unique medical treatment involved. Instruction in cases of
Sudden Infant Death Syndrome (SIDS), child neglect and abuse are covered. During this portion of the program the student is instructed on how to interact with children on their level and provide the proper care for various emergencies.
EMC109 Operations
EMS Operations
Hazardous Materials, Multiple-Casualty Incidents, and Incident
Management
Highway Safety and Vehicle Extrication
EMS Response to Terrorism
Properly lifting techniques of an ambulance stretcher are important not for patient safety but to the safety of the EMT.
There are times when the EMT will need to gain access to a patient such as in an overturned or damaged vehicle. These skills and other emergency responding techniques are presented through lecture and hands on practical skills
32
20
8
6
Page 45 of 60
Classroom
Classroom
Classroom
Classroom
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
EMC110 Advance Airway Management
To enhance the understanding of maintaining an patent airway
Learn how to assist EMTs in the management of an advance airway
EMC111 Skills Module I – Lab hrs
Lifting and Moving of Patients
Airway Management
Baseline Vital Signs
Initial Assessment
EMC112 Skills Module II – Lab hrs
Initial Assessment
Focus Assessment/Vital Signs
Detail Assessment
On-going Assessment
Documentation (Prehospital Care Report)
EMC113 Skills Module III – Lab hrs
Bleeding Control/Shock Management
Rigid and Traction Splinting
Longboard/KED/Shortboard Management
Rapid Trauma Assessment
Outside Patient Extrication
EMC114 Skills Module IV – Lab hrs
•
Midterm and Final Skills Evaluation - All Skill
EMC115 Medical Facility Externship
•
Emergency Department
EMC116 Field Externship
• Advance Life Support Ambulance
EMC117 Field Externship
• Health Care Facility – Pediatric ED
TOTAL PROGRAM HOURS
4
12
24
24
8
36
36
4
250
Introduction to EMT Clinical
Clinical education represents the most important component of EMT education since this is where the student learns to synthesize cognitive and psychomotor skills. To be effective, clinical education should integrate and reinforce the didactic and skills laboratory components of the program. Clinical instruction should follow sound educational principles, be logically sequenced to proceed from simple to complex tasks, have specific objectives, and be closely supervised and evaluated. Students should not arrive in the clinical environments with poorly planned activities; they should know what they must accomplish.
This manual serves to provide that structure and a mechanism to track progress. The ability to serve in the capacity of an entry-level or novice EMT requires experience with actual patients.
This process enables the EMT student to build a database of patient experiences that serves as a matrix to help in clinical decision-making and pattern recognition; i.e. building on experiences of the past to facilitate critical thinking skills.
Classroom
Classroom
Simulation
Lab
Classroom
Simulation
Lab
Classroom
Simulation
Lab
Classroom
Hospital
EMS
Health Care
Facility.
Page 46 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Time is no longer used as the criteria to determine the quantity of clinical education. More than any other phase of EMT education, minimum amounts of patient contacts and frequency of skills performed must be established for clinical education. It is acceptable to use a time-based system to help in program planning, but a system must be used to assure that every student satisfies each and every clinical objective. To this end there is a minimum competency requirement for each clinical area, in both skills and patient categories, and for the entire clinical aspect of the EMT program. Typically, clinical education for the EMT takes place in both the hospital and field environments.
Note: Students are not to function as staff during class, clinical or lab and may not be on duty or subject to call during any part of training program. Students are not to be in the patient compartment alone during patient transport and students may not function to meet staffing requirements for any part of training.
Tardiness for all clinical sites
Students are expected to arrive promptly for clinical. Failure to do so will result in the student being assessed a late arrival. Three late arrivals constitute an absence from clinical. It is a privilege to have preceptors to work with our students and we do not want to abuse this. If at any time a student has a problem with clinical scheduling, he/she should discuss the matter with the
Clinical Coordinator. Due to the unpredictable nature of emergency medical services, punctuality is important.
EMTs arriving late may force a department to operate understaffed or force an off-going crew to be held on overtime. Arriving on time is just as important for students. Showing up even a few minutes late may mean missing your mentor for up to several hours depending on call volume and unit availability. Most importantly, it displays a lack of professionalism and commitment to the EMT Program. You are required to report for your shift 15 minutes prior to the start of shift.
Chronic tardiness will affect your grade and standing in the EMT program. Unexcused absences/tardiness will not be tolerated. The field clinical instructor will determine whether an absence/lateness is excused.
The following action will be taken when a student is late or absent from a scheduled shift without excuse:
First Offense: Verbal Warning
Second Offense: Written Warning
Third Offense: Student, Instructor, and Program Director will meet to discuss and
Fourth Offense: resolve the issue.
Action as determined by the Clinical Coordinator and Program
Director. This action may include dismissal from the EMT program.
If you do find yourself in a situation where you will be late for a shift, you should first notify the person you are scheduled to ride with and then leave a message for your preceptor on voicemail or e-mail. Tardiness or absences that are not reported to the instructor in a timely manner will be considered unexcused. All episodes of tardiness and absence will be reported.
Page 47 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
EMT Hospital Clinical Requirements
The following objectives must be successfully accomplished within the context of the clinical environment. Clinical experiences should occur after the student has demonstrated competence in skills and knowledge in the didactic and laboratory components of the course.
Recommendations are not the only way to achieve the essential. If the program is unable to achieve the recommendations on live patients, alternative learning experiences (simulations, programmed patient scenarios, etc.) can be developed. If alternatives to live patient contact are used, the program should increases in the number of times the skill must be performed to demonstrate competence. These recommendations are based on survey data from EMT Program
Directors and expert opinion. Programs are encouraged to adjust these recommendations based on thorough program evaluation.
Demonstrated Competencies
Upon completion of ED rotations, the student should be able to:
Display the ability to perform a focused, pertinent, and accurate history and physical exam.
Demonstrate a working knowledge of CPR and obstructed airway techniques per AHA guidelines.
Demonstrate an understanding and the ability to perform procedures with aseptic techniques.
Demonstrate the ability to control bleeding and apply dressings and bandages to a variety of wounds using aseptic technique.
Demonstrate an understanding of the principles of splinting, and safely, gently, and effectively immobilize a variety of injuries using these principles.
Demonstrate an understanding of the principles of basic and advanced airway management.
Safely and correctly administer O
2
, choosing devices and flow rates appropriate to patient condition.
Demonstrate the correct methods for the use of Bag-Valve-Mask and demand valve devices.
Demonstrate an understanding of the indications for and use of oropharyngeal and nasopharyngeal airways, and correctly insert them.
Demonstrate an understanding of the indications for orotracheal and nasotracheal intubation, and correctly ASSIST with procedure.
Demonstrate an understanding of the principles of suctioning, and correctly use oropharyngeal and nasopharyngeal suction devices.
EMT Field Clinical Requirements
The student must complete (3) 12 hour shifts with an approved ALS Ambulance. A minimum of five (5) patient transports during the field externship is the goal.
Page 48 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Demonstrated Competencies
The student should assist with and/or perform the following procedures during the Field internship rotations:
1. Perform patient assessment including initial, ongoing, vital signs, and obtaining complete history.
2. Assist with cases of cardiopulmonary arrest by performing CPR, airway maintenance, including BVM and appropriate mechanical adjuncts, and medication administration appropriate to training level.
3. Assist with wound care.
4. Assist with splint and cast application.
5. Assist with the application of O
2 and appropriate airway adjuncts including mechanical aids.
6. Assist with preparation for, and performance of diagnostic and/or therapeutic procedures.
7. Assist with lifting, moving and transportation of patients.
8. Assist with cleaning and restocking of the Ambulance.
Hospital or Other Clinical
Student Responsibilities
1.
Be prompt in reporting for scheduled rotations. If a student knows that he/she will be late for a given rotation, then they must contact the unit or department to notify them that you are going to be late. The clinical coordinator must also be notified. Please leave a message with your name, class, the clinical you are attending and the reason you are late.
2.
Review rules and operating procedures of the given unit with the clinical adjunct at the beginning of the rotation. This will help clarify the student’s role in the unit.
3.
Review clinical objectives for the rotation with the hospital preceptor, and discuss those activities and skills that the student may perform under the supervision of the hospital preceptor. Students may only perform those skills for which they have been properly trained and authorized by the Program Medical
4.
Review relevant patient records to review the patient’s past medical history, physician’s/nurse’s assessments, diagnosis and in-hospital care. It must be clearly understood that all information contained in a patient’s record must remain confidential. Violation of this confidentiality will result in dismissal from the program.
5.
Complete all documentation required for each clinical rotation. The student must have all required forms completed and signed at the end of the particular rotation.
6.
Unexcused missed clinical will not be tolerated.
General Considerations for the Clinical Objectives
Although specific clinical objectives will vary from unit to unit, there are general considerations, which apply to all student activities while in the clinical areas: These include the ability to:
Accurately relate patient complaints to pathophysiology or pharmacologic effects.
Page 49 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Obtain patient history from the patient or his/her chart in a systematic fashion.
Conduct a thorough, appropriate patient assessment, noting signs, symptoms, and other pertinent findings.
Explain procedures to the patient in a manner, which the patient can understand.
Demonstrate professional behavior and genuine concern whenever dealing with patients, family, or other staff members.
Accurately and concisely document assessment findings and therapeutic interventions.
Clinical Goals
1.
An educated EMT should be exposed to a broad variety of patient care environments
(clinic, emergency, in-patient, pre-hospital, home healthcare, and wilderness.)
2.
An educated EMT should have achieved a sufficient depth of knowledge to be said to be competent as a novice EMT provider.
3.
An educated EMT should be able to express him or herself clearly, completely, and accurately in all forms of communications, written, printed, or spoken.
4.
An educated EMT should develop the skills to understand, accept, and relate to people of different backgrounds and beliefs.
5.
An educated EMT should be expected to have some understanding of and experience in thinking about moral and ethical problems.
6.
An educated EMT should have conceptual ability: i.e. the ability to think rationally, to develop informed opinions, and to comprehend new ideas.
Hospital Preceptor
The Hospital Preceptor is a member of the hospital staff that has agreed to help EMT students gain a more meaningful experience. These Hospital Preceptors may be Registered Nurses,
Physician Assistants, Advanced Nurse Providers (i.e. Nurse Midwife) or even Physicians
(Attending Physicians and Residents).
The Hospital Preceptor’s primary responsibility is to their patients and to their employer and it is a privilege for an EMT Student to be permitted to participate in patient care. While teaching is an important aspect of professional conduct, there are times when patient care takes priority and the
EMT student is asked to step aside or even leave the unit.
Clinical Objectives
Students are expected to perform assessments and skills on patients, following the standards taught in class. Students are furthermore expected to document those assessments and skills utilizing the documentation standards distributed in class.
During the first phase of externship clinical, the student can expect the clinical adjunct to meet with the student at the beginning of the shift.
The clinical preceptor will orient the student to the unit and to the hospital, pointing out the
Page 50 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion supply room, conference room, chart room, etc. and introduce the student to the staff.
During the second phase of externship clinical, the student can expect the clinical preceptor to ask the student to demonstrate his or her skills. All skills performed by students in the hospital must be first be demonstrated to an adjunct faculty member in lab who can attest that the student has achieved minimal competency at said skill.
It is the responsibility of the student to enter all assessments and skills performed either in the field or in the hospital into patient care reports and turned in within one week, (7) days, of the completion of rotation.
Location of Clinical
All clinical experiences will be obtained at those locations approved by Nature Coast EMI.
Eight (8) to twelve (12) hours of clinical experiences are scheduled each week. The clinical rotations will begin immediately and conclude two weeks prior to the end of class.
Clinical Assignment
Once a student has been scheduled for a clinical rotation, the responsibility rests with him/her for satisfying the clinical rotation. Students are scheduled for a clinical rotation by the Program
Director or a designate (the Clinical Coordinator). Unless otherwise noted, no student may schedule himself/herself for any clinical rotation.
No more than two students are scheduled in one clinical area at a time. Students will stay with their designated preceptor in the assigned clinical unit. Students may not float to other clinical areas without permission of the clinical adjunct. Preceptors are assigned to students in many of the areas. In other units, the resident physician will serve as the preceptor/supervisor. Students may be permitted to assist other unit staff members with various activities at the discretion of their Clinical Preceptor.
When you arrive on the unit, introduce yourself to the charge nurse. Inform the charge nurse of the length of time that you will be on the unit and show him/her your clinical check sheet. Ask to meet with your preceptor.
Health Assessment
Before any patient contact, every student is expected to have a health assessment completed and on-file. The pre-clinical health assessment includes a record of current immunizations as well as laboratory work. The health assessment ensures that our patient’s are protected as well as the student or faculty. The cost of the health assessment is the student’s responsibility. The health assessment must be completed on the form provided by the school and submitted before any patient contact is allowed.
Page 51 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Physical Forms for Health Status
Physical exam reports must be turned in no later than the end of the first week of class or the student may NOT begin his/her clinical rotations. These forms are turned in to the Clinical
Coordinator.
Health and Liability Insurance
While as a student at Nature Coast EMI’s EMT Program, the student is covered by a general liability policy for acts committed in the course of their instruction as a student. Students are encouraged to consider obtaining additional malpractice insurance at minimal cost that is available from a number of insurance companies. For more information, please contact the program director.
While health insurance is not mandatory, it is highly recommended. Students are responsible for all expenses associated with healthcare while a student including but not limited to needle stick incidents, falls, and other illness/injuries that might occur in the course of the class.
Clinical Attire
Students are expected to wear school uniform for clinical:
Students are expected to wear the approved program shirt with I.D badge.
Women may not wear a skirt at any time during the clinical period.
Black closed-toed shoes are required, boots are recommended.
Sandals or multi-color sneakers are not permitted.
Underclothing may not be visible, particularly T-shirts with printing.
The nametag of the student must be clearly visible on the uniform shirt.
If clothing should become soiled during clinical, the student should change into spare clothes; students are encouraged to bring a change of clothes to clinical.
Personal items like wallets and purses should be secured. The Program takes no responsibility for personal items that are lost or stolen. Students are encouraged to only bring the minimum that is needed.
Jewelry must not interfere with patient care. In general, post earrings are acceptable, while hoop earrings and the like are unsafe and therefore unacceptable. Body piercings must not be visible.
Special Unit Attire
Students will do rotations on special units such as the operating room and childbirth center may have special uniform requirements. Students are expected to comply with the unit’s dress policy.
Clothes are to be left in lockers provided by the unit. Students are reminded to not leave valuables in those lockers.
Infection Control
Students must wear personal protective equipment any time they are in contact with a patient
(i.e. practice standard precautions). The following rules must be adhered to at all times:
Page 52 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
1.
Exposure to blood should be minimized. When the possibility of exposure to blood or other body fluid exists, gloves are recommended. During extrication, or when broken glass is present, leather gloves or fire fighter gloves should be used. If hands accidentally become contaminated with blood, they should be washed thoroughly as soon as possible.
When there is a risk of eye or mouth contamination (for example, the patient is vomiting bloody material or there is arterial bleeding), protective eyewear and masks are recommended.
2.
Needles and other sharp objects should be considered as potentially infective and be handled with extraordinary care. Needles should not be recapped. If it is necessary to recap a needle, use the appropriate technique (shoe holding the cap to the floor).
Needles, syringes and broken vials should be immediately placed in a puncture-proof
“sharps” container after use.
3.
Pocket masks with one-way valves or bag valve masks should be used for artificial respiration.
4.
Masks should be worn by the EMT or patient for those infectious agents known to be transmitted by the airborne route (i.e., tuberculosis, chicken pox, measles, etc.).
Sufficient information should be obtained to determine the presence of respiratory illness.
5.
Equipment should be thoroughly cleaned after each use. Disposable equipment should be considered for use whenever appropriate.
In the event of significant exposure, an instructor should be notified and an incident report filed.
Significant exposure is defined as the following:
Any puncture of the skin by a needle or other sharp object that has had contact with patient’s blood or body fluids or with fluids infused into the patient.
Blood spattered onto mucous membranes (e.g. mouth) or eyes.
Contamination of open skin (cuts, abrasions, blisters, open dermatitis) with blood, vomit, saliva, amniotic fluid or urine. A bite wound to providers would be included in this category.
Conflicts of Interest
To prevent the potential for a claim of conflict of interest students are not allowed to perform clinical rotations in the hospital units in which they are employed, or have relatives/significant others’ as clinical adjuncts, hospital preceptors, field training officers or field preceptors.
Clinical Scheduling Policies
Each student will be scheduled for clinical rotations based upon his or her work schedule and rotation request. Unless otherwise noted, all scheduling is accomplished via electronic mail or written request. Final scheduling rests with the Program Director or designates (Clinical
Coordinator).
AT NO TIME IS A STUDENT TO ARRANGE HIS/HER OWN CLINICAL ROTATIONS.
Failure to comply will result in disciplinary action and may result in dismissal from the program.
Page 53 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Cancellation of clinical rotations due to illness or injury must be made at least one (1) hour in advance of the scheduled rotation. Failure to comply will result in disciplinary review and may result in dismissal from the program. In case of emergency, advance notification may be waived.
Please note that all time missed from clinical shifts, regardless of reason, must be made up.
Regulation and Control
Failure to abide by the above listed rules may result in the student be asked to leave Clinical or
Externship by the hospital preceptor, clinical adjunct, field training officer, or the externship preceptor. Ejection will result in an absence recorded in attendance. Students may be asked to leave a unit or agency at any time by a member of the staff of the facility or agency. The student shall immediately comply, without comment, with the request and report the situation to the clinical coordinator.
EMT Field Clinical
Agency Assignment
Students are assigned to field agencies based on unit availability, Field Preceptor availability and unit call volume. All students will function under the direct supervision of an EMS preceptor and shall not be in the patient compartment alone during transport and shall not be used to meet staffing requirements in accordance with Section 64J-1, Florida Administrative Code.
Field Clinical Uniform
The standard Nature Coast EMI approved student uniform will be required: polo shirt with embroidery and navy blue EMT Pants. The Nature Coast EMI must approve coats and warm weather clothing.
Scheduling (Hours/Reporting)
Students are responsible for scheduling Field Clinical with the Clinical Coordinator. During each phase of the program, students must complete a minimum number of clinical hours. Students should obtain the Clinical Coordinator’s schedule and discuss what shifts are open for the student to attend. The student must turn in a schedule of their shifts for each phase before the end of the second week of classes. The Clinical Coordinator must approve schedules. The Clinical
Coordinator must approve any changes one week in advance. It is strongly discouraged for students to make any changes to their schedule once it is filed. Any changes must be submitted in writing to the Clinical Coordinator with a detailed description of the reason for the change.
Page 54 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
EMT TEXTBOOKS/LEARNING RESOURCES:
Brady 12 th Edition Textbook – Emergency Care – Copyright 2012
Brady 12 th
Edition Textbook – Emergency Care – Copyright 2012
Resource Central EMS Student Access Card – Pearson Copyright 2012
MyBrady Lab – Pearson – Emergency Care – 12 th
Edition
Paramedic TEXTBOOKS/LEARNING RESOURCES:
Advanced Cardiac Life Support, current edition, American Heart Association - 2011
Paramedic Care: Principles & Practices, 4/e , Bledsoe, (Brady) 2012
Paramedic Care: Principles & Practices, 4/e , Bledsoe, (Brady) 2012 Workbook
Pediatric Advanced Life Support, current edition, American Heart Association - 2011
Prehospital Trauma Life Support, current edition, Mosby (AEMT) - 2010
Essentials of A & P for Emergency Care, Bledsoe, Colbert (Brady)2011
Prehospital Emergency Pharmacology, 7th Edition, Bledsoe 2011
Holiday Calendar
New Year’s Day
Martin Luther King, Jr. Day
President’s Day
Memorial Day Observed
Independence Day
Labor Day
Thanksgiving Day
Day after Thanksgiving
Christmas Day Observed
Academic Calendar
Nature Coast EMI offers:
Open Enrollment beginning and Ending Dates of all programs are available on our website: www.NatureCosatEMS.org
New Years Day Observed
Student Services
As a service to our students, Nature Coast EMI will provide an updated job listing board in the library and on the website. We will also provide each class, periodic opportunities, where area recruiters will provide information about their services and/or departments and be able to provide hiring criteria and application information. Nature Coast EMI will assist students with job placement, but does not guarantee job placement or employment.
Sexual Harassment/Discrimination
Nature Coast EMI will not tolerate any kind of harassment and/or discrimination in any form.
This policy will be adhered to by the faculty as well as all students.
Nature Coast EMI abides by the following law:
It shall be unlawful employment practice for an employer to refuse to hire or to discharge any individual or otherwise to discriminate against any individual with respect to his compensation, terms, conditions, or privileges of employment because of such individual’s race, color, religion, sex or national origin.
Page 55 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Accreditation
Nature Coast Emergency Medical Institute is not accredited by the Committee on Accreditation of Educational Programs for the Emergency Medical Services Professions (CoAEMSP). Nature
Coast Emergency Medical Institute is in process of submitting a Letter of Review (LoR) for
CoAEMSP and once accepted, paramedic students will be eligible to sit for the National Registry
Paramedic Exam as well as the Florida State Paramedic Exam. Students that enroll in this institution may not be eligible for Title IV Federal Financial Assistance, and state student financial assistance. In addition, credits earned at this institution may not be accepted for transfer to another institution, and may not be recognized by employers.
Nature Coast EMI Licensure and Approval Board:
Commission for Independent Education
License No. 4158.
325 West Gaines St, Ste. 1414
Tallahassee, Fl 32399-0400
(888) 245-3200 (toll free)
Florida Department of Health
Division of Medical Quality Assurance
EMT/Paramedic Certification Office
4052 Bald Cypress Way, Bin C85
Tallahassee, FL 32399-3285
Phone: (850) 488-0595
Fax: (850) 921-6365
Web: www.doh.state.fl.us/mqa/EMT-Paramedic
Page 56 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Nature Coast EMI Equipment List
AIRWAY
Oral pharyngeal airways
Nasal pharyngeal airways
Bag valve mask
Pocket mask with one way valve
SUCTION
Portable suction unit
Connecting tubing
Soft tip suction catheters
Rigid suction tip
Meconium Aspirator
Bulb syringe
Oxygen (O2) and Supplies
O
2
tank with wrench
Regulator with high flow port
Demand valve **
Bite sticks
High concentration mask
Simple face mask
Nasal cannulas
Venturi mask
O
2
tubing
Nebulizer
DIAGNOSTIC EQUIPMENT
Blood pressure cuffs
Infant)
Stethoscopes
Teaching stethoscopes
Thermometer
Penlights
INFECTION CONTROL
Gloves (latex, non-latex, & powder free)
Disinfectant
Biohazard trash bags
Sharps container
Personal protective equipment
PHARMACEUTICALS
Insta glucose
Epi Pen trainer
Activated charcoal
Placebo inhalers
Nitroglycerin
(Adult, Child, & Infant)
(Adult, Child, & Infant)
(Adult, Child, & Infant)
(Adult)
(Battery Powered & Manual)
(Sizes 6 - 18 French)
(Adult, Child, & Infant)
(Adult, Child, & Infant)
(Adult, Child, & Infant)
(Adult)
(Thigh, Large Adult, Adult, Child, and
(Adult & Pediatric)
(All Sizes)
(Gown, Eye & Face Shields)
(May be simulated)
Page 57 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
MEDICAL TRAINING EQUIPMENT
AED trainer with pads
CPR manikins
Airway manikins
Childbirth manikins
Full body basic life support manikins
Moulage kit
IMMOBILIZATION AND EXTRICATION
Non-wood long spine board with straps
Short board
Vest style immobilization device with straps
C-collars
Head immobilizers
Basket stretcher
Scoop stretcher
Car seat
Flexible stretcher
Patient restraints
SPLINTS
Traction splints (two out of the three)
Vacuum
Air
Padded board splints
PATIENT TRANSPORT EQUIPMENT
Stretcher with straps
Stair chair with straps
BANDAGES AND DRESSINGS
Elastic bandage
Roller gauze
Non-sterile or sterile sponges
Abdominal pads
Multi trauma dressing
Non-adherent dressing
Petroleum gauze
Triangular bandages
Eye pads
Band-aids
Tape
Cold packs
Burn sheets
OB kits
Tongue depressors
MISCELLANEOUS
(Adult & Child)
(Adult, Child & Infant)
(Adult, Child & Infant)
(Adult & Child)
(Adult & Pediatric)
(Adult & Pediatric)
(Adults)
(Adult Child & Pediatric)
(Adult & Pediatric)
(Child & Infant)
(Adult & Pediatric)
(Assorted sizes)
(Assorted sizes)
(Assorted sizes)
(Must be capable of multi level positioning)
(Assorted sizes)
(May be simulated)
Page 58 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Trauma shears
Ring cutter with extra blades
Emergency/Survival blanket
Jump bag
Helmets
Football Helmet and Shoulder Pads
(Open & Full face)
PARAMEDIC TRAINING PROGRAM EQUIPMENT AND SUPPLIES
In addition to equipment and supplies required for EMT Training Programs
AIRWAY
Esophageal intubation detector (Two out of three)
Colorimetric CO2 detector
Bulb type intubation detector
Syringe type intubation Detector
Endotracheal tubes
(Adult & Pediatric)
(Adult)
(Adult)
(Sizes 2.5-8)
Naso-gastric tubes
Commercial manufactured tube holder
Laryngoscope handles with batteries
Laryngoscope with Macintosh and miller blades
Replacement laryngoscope light bulbs
Stylettes
Lighted stylettes
Cricothyrotomy kit
(Assorted sizes)
(Adult & Pediatric)
(Adult & Pediatric)
(Complete set of each)
(Assorted sizes)
(Adult)
Pneumothorax kit
Superglotic airways
OXYGEN AND SUPPLIES
Continuous Positive Airway Pressure (CPAP) with Circuits and Mask
Automatic Ventilator with Circuits Mask and Peep Valve
(Adult)
(Adult & Pediatric)
DIAGNOSTIC EQUIPMENT
Glucometer with lancets and test strips
CARDIOLOGY SUPPLIES
Cardiac monitor capable of defibrillation with cables
Cardiac monitor capable of defibrillation, 12 lead EKG, and pacing, with cables. and wave form end title carbon dioxide detector capable of printing.
Battery support system with spare batteries
EKG paper
Rhythm generator capable of generating 3 or 4 lead displays
Rhythm generator capable of generating 12 lead rhythms
IV AND PHARMACEUTICALS SUPPLIES
IV catheters
Butterfly needles
Blood collection tubes
Vacutainer device with luer adapter
Syringes
Hypodermic needles
(Sizes 22 – 14 gauges)
(Assorted Sizes)
(Sizes 3-20cc)
(Sizes 25-18 gauge)
Page 59 of 60
NATURE COAST EMERGENCY MEDICAL INSTITUTE STUDENT CATALOG
Serving with Excellence and Compassion
Intraosseous Needles
Practice medication ampoules, vials, and premeasured syringes
Macrodrips IV sets
Microdrips IV sets
IV extension sets
3 way stop cocks
Buretrol solution set
IV fluids
IV start kits
ADVANCED LIFE SUPPORT PHARMACOLOGICAL DRUGS
(May be commercially packaged or simulated)
Atropine
Dextrose
Furosemide
Magnesium
Nalaxone
Sodium Bicarbonate
Epinephrine 1:10000
Epinephrine 1:1000
Lidocaine
Amiodarone
Dopamine
Vasopressin
Procinamide
Adenosine
Digoxin
Verapamil
Cardizem
Morphine Sulfate
Nitroglycerin
Aspirin
Lidocaine drip
Dopamine drip
MEDICAL TRAINING EQUIPMENT
IV trainer
Cricothyrotomy manikins
Intraosseous trainer
IM and Sub-Q injection trainer
Pneumothorax trainer
Full body advanced life support manikins
Consumable parts for all trainers
Triage tags
Two-way communication radios or walkie-talkie
Length-Base resuscitation device
(Adult)
(Adult)
(Pediatric)
(Adult & Pediatric)
(Adult)
(Adult, Child, & Infant)
(Adult, Child, & Infant)
Page 60 of 60