Joe`s Allergic Reaction Outline
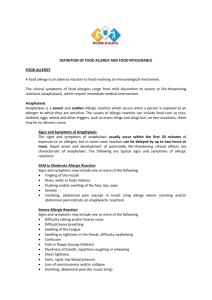
advertisement
Allergic Reaction: Overview • Allergy – Inappropriate, often harmful response to a normally harmless substance • Atopy – Genetic predisposition to allergic rxns.(Ex: Seasonal allergies • Rise in IgE and Esinophils • Antigen – Foreign invaders. (ex: Pet Dander, peanuts) • Antibody – Attacks the antigen Function of IgE • Bind with… Antigens. This triggers the mast cell “Water balloon of chemical mediators (ex: histamine, leukotrienes)” – Will see skin reactions, whelps, Diff breathing, Laryg Edema, hives, rashes • Trigger… • Release chemical mediators • Disorders Reference pg1860 • Antigen B-Cells IgE binds Antigen • Stimulates release to mast cells binds to • B-Cell IgE IgE Chemical Mediators • Released from stimulated mast cells • Trigger sequence of events resulting in symptoms • 2 types – Primary Mediators – Secondary Mediators Primary Mediators, Pharm Chap 69 • Histamine – Effects: Edema, Airways, Bronchi, Laryngeal edema, Itching, redness of skin, Mucosa membranes eye/nose (weeping of tissues in general) – Maximum amount of intensity is w/in 15min of contact w/ antigen – Constriction of bronchioles – Dilation of small vessels & constriction of core vessels – Two types: *H1 receptors- bronchiolar and vascular smooth muscle cells. Activation of H1 receptors causes dilation of small blood vessels. Incr capillary permeability. Bronchoconstriction. Itching/Pain. Mucous secretion. (ex: Benadryl) *H2 receptors- gastric parietal cells. Activation of H2 receptors is secretion of gastric acid. Allergic responses. Histamine release. Severe = Anaphylaxis, (treat: epinephrine). (ex: Zantac, pepcids) Other Primary Mediators • Eosinophil Chemotactic factor – Eosinophils- They incr in number with allergy and parasitic conditions and decr w/ steroid administration. Larger than Neutrophils. • Platelet aggregating factor • Prostaglandins (Will cause the inflammation along w/ fever and pain) Secondary Mediators released in response to a primary • Each causes smooth muscle contraction & increased vascular permeability • Leukotrienes- responsible for the inflammatory response (responsible for wheals/whelps in skin) • Serotonin- Vasoconstrictor • Bradykinin- responsible for muscous production Hypersensitivity – 4 types • Type I – Anaphylatic • Type II – Cytotoxic • Type III - Immune Complex • Type IV - Delayed Type I - Anaphylactic • Most severe form of hypersensitivity • Characterized by edema in many tissues & hypotension • Begins within minutes, mediated by IgE antibodies (if no increase in IgE than its not Anaphylactic Reaction) • Type 1 is a TRUE ALLERGY • Severity depends on exposure, amount of allergens, sensitivity of target organs, and route of allergen exposure. • Requires previous exposure Examples of Type I Reactions • Extrinsic asthma- outside source, ex: pet dander • Allergic rhinitis • Systemic anaphylaxis • Insect sting reactions • Vasodilation in extremities, incr capillary permeability, smooth M Contraction, and high levels of eosinophils. Type II or Cytotoxic • Body attacks self- cytotoxic- related to compliment cascade. Ex (Mgravis, blood transfusion reactions) • IgG or IgM antibody • Activation of complement cascade • Cell destructionType III or Immune Complex • Involves IMMUNE COMPLEXES, when antibody binds w/ antigen. They don’t break down the way they should and form slusters leading to… • Phagocytosis- tissue damage. • Injury due to – ↑Circulating complexes & Vasoactive amines – ↑ vascular permeability & tissue injury. – Joint & kidneys Type III or Immune Complex • Systemic Lupus Erythematosus (SLE) • Rheumatoid Arthritis • Nephritis • Bacterial Endocarditis Type IV Delayed Hypersensitivity Non- Atopic reactions, so no incr in IgE or Eosinophil levels • • Occurs 24-72 hrs after exposure Examples – TB test – Poison Ivy – Contact dermatitis (tape, topical medications, cosmetics) • S/S = Itching, erythema, raised lesions Nursing Care of Hypersensitivity See Chart 53-7, pg 1876 Assessment • History • Physical assessment Diagnostic Testing • WBC – Normal, because its antigen, not infection • Eosinophils (granulated WBC) • Normal 1-3% • ^ 5-15% suggestive allergy • ^15-40% moderate • ^50-90% severe- Definite allergic reaction • Eosinophil count of tissue smear – Swab in mouth, oral, throat Diagnostic Testing • IgE level – ↑ IgE levels indicate allergic disorder • Useful in evaluation of: – Immunodeficiency – Drug reactions – Atopic vs. non-atopic dermatitis, asthma, and rhinitis Diagnostic Testing • Skin tests – Prick/Scratch (easiest test available) – IntraDermal (injection of antigen INTO the skin) • Interpretation – Urticarial wheal, erythema, or pseudopodia “reaching outward of redness” – Do not perform while pt has active bronchospasm Diagnostic Testing • Provocative testing- direct admin of allergen into target tissue. – Only one test per visit. • RAST (Radioallergosorbent Test)- The patient's blood is mixed with a possible allergen in a test tube. – The Safest cause there is no pt contact. Allergic Disorders • 2 types – Atopic • IgE & Genetic predisposition • Allergic rhinitis • Allergic asthma • Atopic dermatitis – Non-atopic • No IgE • No organ specificity • No genetic link Anaphylaxis – Type I Hypersensitivity • Reaction of Antigen + IgE antibody • Release of histamine, other mediators, & WBCs – Smooth muscle spasm – Bronchospasm – Mucosal edema – Inflammation – Increased capillary permeability- fluids are seepiong into the tissue Anaphylaxis – Type I Hypersensitivity Clinical Manifestations • Mild – Tingling/ warmth, – fullness in mouth/throat – Nasal congestion – Perioribital swelling – Pruritis – Sneezing • Moderate – Sx of mild rx & • Flushing • Warmth • Anxiety • Itching Anaphylaxis Clinical Manifestations • Severe (right amount to rt organ Cardiac arrest = PTTP) – Abrupt onset of previous symptoms – Bronchospasm – Laryngeal edema – Severe dyspnea – Cyanosis – Hypotension… cardiac arrest Management of Anaphylaxis • Prevention – Avoidance!!! – Epinephrine- epi pen on hand = good. But only use when having reaction! Normal + Pen = Cardiac arrest – Screening for allergies – Identification- allergy band = good Anaphylaxis – Type I Hypersensitivity • Medical Management – Depends on severity – Support Resp/Cardiac fx • Oxygen • Epinephrine 1:1000 SQ, then IV • Antihistamines, Benadryl, cortisone- to decr inflammation so pt can breathe • Iv fluids, volume expanders, vasopressors • Possibly aminophylline or steroids – Desensitization- commonly done for insulin, aka “Controlled anaphylaxis” Anaphylaxis – Type I Hypersensitivity Nursing Management • Assess pt with allergies for s/sx anaphylaxis • Increasing edema • Respiratory distress • Notify physician • O2 • Prepare emergency meds • Patent IV • Document response, VS, labs Allergic Rhinitis • a.k.a. Hay fever- most common foorm of respiratory allergy • Often with conjunctivitis, sinusitis, & asthma • Complications – Chronic nasal obstruction, polyps, or obstruction in airways – Chronic otitis media – Anosmia- lack of smell Allergic Rhinitis • HISTAMINE!! – Tissue edema d/t vasodilation and increased capillary permeability. Manifestations of Allergic Rhinitis…. • Nasal congestion • Clear, watery discharge • Sneezing • Itching • Dry cough • Headache • Sinus pain Allergic Rhinitis • Not a severe disease but a serious disease in that it greatly affects quality of life… – Fatigue – Loss of sleep – Poor concentration – Dry, chapped, sore skin to face Assessment of Allergic Rhinitis • History- how long had it, anything improves it? • Physical Assessment • Allergy testing • Serum IgE levels Management of Allergic Rhinitis • Relieve symptoms – Avoidance therapy – Immunotherapy (allergy shots)- kinda like desensitization – Pharmacotherapy • • Antihistamines- Benadryl (but its sedating), so Zyrtec, Claritin Adrenergics- stop mucosal weeping, decr edema. Short term use, else poss Rebound Effect. • Mast Cell Stabilizers- Nasalcrom • Corticosteroids- Flonase, Nasonex (localized steroids) – Education Allergic Rhinitis: Nursing Diagnoses • Ineffective breathing pattern • Deficient knowledge- decongestants will raise BP • Ineffective individual coping- inability to breath. Feels miserable. Contact Dermatitis • A type IV hypersensitivity • Clinical Manifestations – Acute or Chronic skin inflammation – Itching – Burning – Skin lesions – Edema – Weeping, crusting, drying and peeling of skin – Risk of secondary infection d/t scratching • Assessment • Four types: – Allergic- pt is suceptible to a certain thing – Irritant- 80% of contact dermatiitis cases – Photoxic- chem irritant and a sun exposure – Photoallergic- sun exposure and allergen contact Atopic Dermatitis An allergic contact dermatitis • A.K.A. Eczema • A type I sensitivity disorder. • Common in children. • Have dry, red, hyperirritable skin – Extended contact could lead to severe reaction – Treat w/ topical cream Dermatitis Medicamentosa • Skin rash from internal medication administration (causes BRIGHT RED RASH) • Sudden onset. Stop med that causes this, else poss Anaphylaxis. • Common type adverse drug rx • Intense, vivid color • Other systemic symptoms possible • Alert patient to hypersensitivity (for future prevention) Urticaria • Hives – Pinkish, edematous elevations – Itch, local discomfort – Angioneurotic edema = Angio edema (the deeper layers of skin. Includes eyelids, lips, feet, tongue) • Caution for airway obstruction – Prepare for poss Tracheostomy Common side effect of ACE Inhibitors • Food Allergies • Type 1 Hypersensitivity • The Usual Suspects?? – Seafood, legumes, seeds, nuts – Egg whites, Milk, Chocolate – Classic allergic and GI symptoms – N/V/D, swelling of lips and tongue, Abd pain, Wheezing • Elimination is key to mgmt • Drug therapy – H1/H2 blockers – Antihistamines – Adrenergic- in case of reaction – Steroids- reduce inflammation • Nursing Mgmt – Prevention, Pt & family teaching, recognition of sx • Latex Allergies Keep in mind of all the products that contain… • Implicated as cause in many allergic responses – Rhinitis -Conjunctivitis – Contact dermatitis -Urticaria “hives” – Asthma -Anaphylaxis Latex Allergy • 1-3% pop. (10-17% HCW) • 19% of anesthesia reactions • Routes of exposure – Cutaneous, mucosal, – Parenteral, aerosol (powder) Latex Allergy Clinical Manifestations • Irritant Contact dermatitis (redness, itching) – Non-immunogenic response – Erythema, pruritus – Treatment: • change brands/type Latex Allergy - Type 1 • Type I – Immediate – Rhinitis, conjunctivitis, asthma, anaphylaxis • Signs & Symptoms: – Localized itching -Erythema – Hives -Angioedema – Rhinitis -Conjunctivitis – Anaphylactic shock -Cardiac arrest Latex Allergy – Type IV • Type IV – Delayed (Most common type) – vesicular skin lesions on back of hands, papules, pruritus – Most common type • Latex Allergy Diagnosis: -Skin tests (Prick Test) -RAST test (blood sample) Treatment: -Avoidance -Antihistamines -Emergency supplies • Ask all patients about allergies before beginning treatment • Make sure you post signs and remove latex materials from the room. • Teach pt. epinephrine self-injection