Small Group Activities Article Summary April 17
advertisement
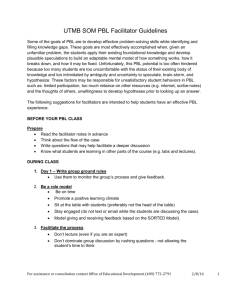
Small Group Activities 18 articles were reviewed. Four of these articles are on Simulation Based Learning; seven on Team-Based Learning, and the rest on Problem-Based Learning. Practice points TBL is a feasible and effective educational approach in preparing large numbers of students for learning in a PBL environment. Its implementation could be adapted to fit the course objectives, content and context. TBL is a cost-effective and less resource demanding approach that appears to develop students’ understanding of PBL. TBL could be combined with PBL as a strategy to support guided discovery learning. PBL is resource intensive for faculty and these resource implications may cause resistance to any intended introductory courses. Students joining an integrated PBL medical curriculum need to be prepared for their future learning. Phase one: ‘Preparatory phase’ Four mini workshops (2 h each) were conducted over a period of 4 weeks. It introduced students to adult learning principles, small group and PBL, concept mapping, reflective and constructive feedback, self and peer evaluation and information search, assimilation and presentation. This gave the students a background understanding of why the school had adopted a PBL approach to learning. Phase two: ‘Application of TBL and PBL’ This phase extended over 6 weeks. All students were introduced to three health related problems: (a) the newborn, antenatal and postnatal care, (b) obesity in adulthood, and (c) care of the elderly (Figure 1). Each problem was studied over two sessions (2 weeks); one session per week for 2 h. Session one included in-class and out-of-class activities. In the class, each team read the problem and discussed possible explanations of the different cues and identified team-learning issues. In each team, the tutorial session was lead by one student ‘peer tutor’ (Maudsley et al. 2007). The ‘peer tutor’ was responsible for facilitation of ‘intragroup. Phase three: ‘Student’s assessment and course evaluation’ The assessment blueprint was developed in order to match assessment instruments with the course outcome. Program evaluation and students’ perception of the course was obtained through a structured questionnaire which included 28 items measuring individual students’ perception of the course learning process (TBL/PBL) and learning skills (12 items), knowledge contents (2), personal development (3), educational environment (3), student assessment (1) and evaluating the faculty (7) Abstracts articles Abdelkhalek N, Using TBL approach to prepare students for PBL approach. University of Sharjah, UAE & Chinese University of Honk Kong, China This study looked at using Team Based Learning (TBL) method to get students ready for a Problem Based Learning (PBL) curriculum. Study included 363 medical and dental first year students. They were divided into 25 per class and then into groups of 8 or 9 in a group. A questionnaire with 28 questions was used in evaluation. The study used mean score and averages to rate student satisfaction with the method. Results proved that the TBL method was successful, extremely satisfied students and the students were ready for PBL curriculum in a week. Haidet P, 2012 on TBL This study proposes guidelines for using the TBL method and also about reporting the results. They identify the seven core elements of the TBL method and relate them to educational principles that maximize student engagement and learning. Hartling L, 2010 on PBL, University of Alberta, Canada This article is a systematic review on PBL. Studies included were 30 (MEDLINE, PSYCINFO & ERIC). Results indicate that PBL does not impact knowledge acquisition. Koles PG, 2010 This study looks at TBL and how it affects students’ performance in examinations. Study looked at 178 second year medical students and how they fared in 28 comprehensive course exams over a 2 year period. The students performed better in their exams related to course content. Students in the lowest quartile benefit more than the students in the upper quartile. McGaghie WC, This article (Review) evaluates studies on Simulation Technology in undergraduate and graduate medical education and its implications for CME. It concludes that this technology is a powerful tool in health education. It does not replace real patient interactions and caring but just complements it.