File
advertisement
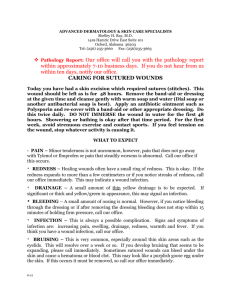
Concept Map: Case Scenario Student: Misbah Sami Student # 822313441 Professor: Kelly Ross NURS 252-015 Complex Issues and Patient Safety Humber College ITAL 1 Concept Map: Case Scenario 2 The purpose of writing this paper is to provide an evidence based rationale for selecting priority pathophysiological diagnosis, symptoms, and treatment. My case scenario is of a 63 year old female who has been diagnosed for stage 1 left breast cancer and is undergoing radiation for its treatment. There is stage 2 skin breakdown at radiation site. She comes in emergency with severe burning pain and irritation at radiation site. She also complains of weakness and numbness in left arm and radiating to hand. Her vital signs are as follows: temp. 38.3, pulse. 84, resp.16, B.P.135/90, Oxygen sat. 98% on R/A, auscultation: no adventitious sounds Priority Pathophysiological Nursing Diagnosis and Evidence Based Rationale: Infection due to impaired skin integrity at radiation site: In the treatment of breast cancer, localized radiation therapy follows or precedes local surgical resection of the tumor. Its purpose is to destroy cancer cells in and around the original tumor site. This combination is highly effective in this cancer's treatment. Although radiation therapy can play a significant role in the cure or control of cancer, and the palliation of symptoms, it also has side effects. Ionizing radiation causes damage to the DNA of cells, limiting their ability to divide and reproduce. Radiation causes damage to both cancerous and normal cells. As Poirier. P ( Nursing: Research and Reviews, 2013) describes, " Radiation skin reactions or radiation dermatitis occur in nearly all patients receiving radiation therapy. ...... Modern equipment and sophisticated treatment planning techniques produce a "skin-sparing" effect, with the therapeutic dose delivered to the target organ, minimizing the dose to the skin. Still, approximately 95% of patients receiving radiation therapy may experience some degree of skin reaction, ranging from mild erythema to more serious and uncomfortable moist desquamation." Concept Map: Case Scenario 3 Most cases of infected wounds are caused by bacteria, originating either from the skin, other parts of the body or the outside environment. The skin contains bacteria (normal flora) which are normally harmless if the skin is intact. However, the protective barrier formed by the skin is disrupted when there is a wound such as after radiation treatment, and these normal flora are able to colonize the injured area. Infection is described as a continuum from contamination, colonization, critical colonization, to infection It is important to recognize that all open wounds are contaminated with non replicating organisms on the surface of the wound that are ordinarily cleared by the host. As the bacterial burden increases, colonization occurs when organisms replicate, increase in number, and adhere to the wound bed without causing harm or injury to the host. When replicating organisms-present in the wound bed-cause changes that trigger the body's immune response locally at the wound site but not systemically, critical colonization has occurred, which may begin to delay wound healing. If this process is unimpeded, the organisms in the wound and surrounding soft tissue can further increase and cause a host response resulting in non healing or deterioration and breakdown of the wound leading to wound infection. (Cook. L, Ousey. K, 2011). Patients with any kind of malignancy and those receiving chemotherapy or radiation therapy are also at increased risk for all kinds of infections. Fever as Priority Clinical Manifestation of Infection and Evidence Based Rationale: Fever is a clinical manifestation of spreading or systemic infection (Groeneveld, A. B. J., Bossink, A. W. J., van Mierlo, G. J., & Hack, C. E. , 2001). If a wound gets infected, patient initially reacts with an acute inflammatory response. Fever is a manifestation of the release of proinflammatory cytokines (interleukin-1Î, interleukin-1Î2, interleukin-4, interleukin-6, and tumor necrosis factor Î) from macrophages, lymphocytes, fibroblasts, epithelial cells, and endothelial cells as a consequence of infection or inflammation. At this initial stage there might Concept Map: Case Scenario 4 be classic signs of inflammation such as pain, redness, swelling and heat. If the infection is not controlled and keeps progressing from contamination to spreading and systemic infection, it indicates multiplication of bacteria causing systemic reactions. The multiplying micro-organisms in the wound now have overwhelmed the host's immune response leading to sepsis, bacteraemia, and pyrexia. Cancer patients who have a break in skin or mucosal barrier are immunocompromised and thus at increased risk of fever because microorganisms can cause local or systemic infection ( Pizzo, P. A., 1999). Evidence Based Treatment of Infection: Antipyretics: NSAIDs, including ibuprofen, are well established analgesic, antipyretic and antiinflammatory drugs for use in the clinical setting, including in hospitalized patients ( Lesley, J, S, 2012 ). The release of products of inflammation such as thromboxane A2 ( vasoconstrictor ), prostacyclin ( vasodilator ), and prostaglandin E2, result in symptoms of fever, increased heart rate, increased rate of breathing and lactic acidosis. Use of ibuprofen to halt the production of these products of inflammation reduces temperature, heart rate, breathing rate and lactic acidosis. But it does not reduce the mortality rate associated with it. It means that antipyretics should be used in combination with antibiotics after receiving the culture report. Systemic Antibiotics: Fever can be a sign of infection induced syndrome called sepsis or systemic infection. To reduce the mortality rate due to sepsis, there needs to be better control of underlying infection. Cultures from obvious infectious sites should be obtained before starting the antibiotic therapy. Mortality rate is higher for patients who do not receive prompt antibiotic therapy. Antibiotic Concept Map: Case Scenario therapy should be started as soon as infection is suspected and later when results of culture are obtained, therapy can be narrowed to most sensitive selection of antibiotics ( Wheeler, A. P., & Bernard, G. R. , 1999). The physical methods of Reducing Fever: The physical methods of reducing fever by cooling the body with drinking plenty of water and removing extra clothing, or tepid sponging are not much effective if used as monotherapy without the use of antipyretics. Although these methods may be successful to initially lower the temperature but this effect is not long lasting and ultimately antipyretics and antibiotics remain the mainstay for the treatment of fever and underlying infection (Purssell, E. , 2000). 5 Concept Map: Case Scenario References ( All Peer Reviewed Articles have been retrieved from Humber Library Website ) Cook, L., & Ousey, K. (2011). Demystifying wound infection: Identification and management. Practice Nursing, 22(0964-9271), 424-428. Groeneveld, A. B. J., Bossink, A. W. J., van Mierlo, G. J., & Hack, C. E. (2001). Circulating Inflammatory Mediators in Patients with Fever: Predicting Bloodstream Infection. Clinical and Diagnostic Laboratory Immunology, 8(6), 1189–1195. doi:10.1128/CDLI.8.6.1189-1195.2001 Poirier, P. (2013). Nursing-led management of side effects of radiation: Evidence-based recommendations for practice. Dovepress, 3, 47-57. Pizzo, P. A., M.D. (1999). Fever in immunocompromised patients. The New England Journal of Medicine, 341(12), 893-900. Retrieved from http://search.proquest.com/docview/223957564?accountid=11530 Purssell, E. (2000). Physical treatment of fever. Archives of Disease in Childhood, 82(3), 238– 239. doi:10.1136/adc.82.3.238 Lesley, J, S. (2012). Intravenous Ibuprofen: In Adults For Pain and Fever. Proquest, 1099-1109 6 Concept Map: Case Scenario Wheeler, A. P. , & Bernard, G. R., (1999). Treating patients with severe sepsis. The New England Journal of Medicine, 340(3), 207-214. Retrieved from http://search.proquest.com/docview/223953810?accountid=11530 7