Framework For Locality CHTs – Referral Criteria
advertisement
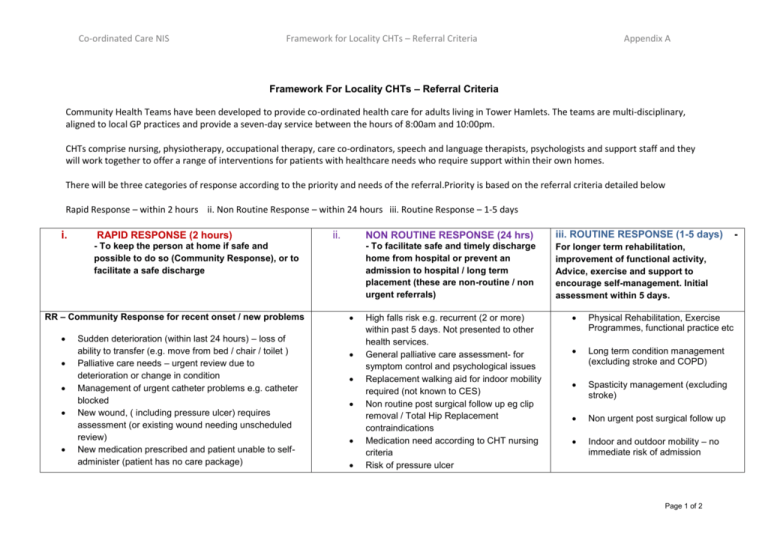
Co-ordinated Care NIS Framework for Locality CHTs – Referral Criteria Appendix A Framework For Locality CHTs – Referral Criteria Community Health Teams have been developed to provide co-ordinated health care for adults living in Tower Hamlets. The teams are multi-disciplinary, aligned to local GP practices and provide a seven-day service between the hours of 8:00am and 10:00pm. CHTs comprise nursing, physiotherapy, occupational therapy, care co-ordinators, speech and language therapists, psychologists and support staff and they will work together to offer a range of interventions for patients with healthcare needs who require support within their own homes. There will be three categories of response according to the priority and needs of the referral.Priority is based on the referral criteria detailed below Rapid Response – within 2 hours ii. Non Routine Response – within 24 hours iii. Routine Response – 1-5 days i. RAPID RESPONSE (2 hours) ii. - To keep the person at home if safe and possible to do so (Community Response), or to facilitate a safe discharge RR – Community Response for recent onset / new problems Sudden deterioration (within last 24 hours) – loss of ability to transfer (e.g. move from bed / chair / toilet ) Palliative care needs – urgent review due to deterioration or change in condition Management of urgent catheter problems e.g. catheter blocked New wound, ( including pressure ulcer) requires assessment (or existing wound needing unscheduled review) New medication prescribed and patient unable to selfadminister (patient has no care package) NON ROUTINE RESPONSE (24 hrs) iii. ROUTINE RESPONSE (1-5 days) - To facilitate safe and timely discharge home from hospital or prevent an admission to hospital / long term placement (these are non-routine / non urgent referrals) For longer term rehabilitation, improvement of functional activity, Advice, exercise and support to encourage self-management. Initial assessment within 5 days. High falls risk e.g. recurrent (2 or more) within past 5 days. Not presented to other health services. General palliative care assessment- for symptom control and psychological issues Replacement walking aid for indoor mobility required (not known to CES) Non routine post surgical follow up eg clip removal / Total Hip Replacement contraindications Medication need according to CHT nursing criteria Risk of pressure ulcer Physical Rehabilitation, Exercise Programmes, functional practice etc Long term condition management (excluding stroke and COPD) Spasticity management (excluding stroke) Non urgent post surgical follow up Indoor and outdoor mobility – no immediate risk of admission Page 1 of 2 - Co-ordinated Care NIS Framework for Locality CHTs – Referral Criteria Fall with injury requiring assessment (recurrent non injurious falls will be seen as per 1-5 days pathway) Client / carer at immediate risk of injury due to manual handling Breakdown of urgent equipment (if not covered by CES) Breakdown of social / care package e.g. carer in hospital etc (Note: clients not known to the CHT’s will be managed by First Response social care team) Acute chest infection / aspiration. Client at risk of admission and requires assistance with secretion clearance(must have already been seen by GP/Consultant within 24 hours and commenced on antibiotics) Urgent symptom management for long term conditions (excluding stroke and COPD) or frial complex client Death of a client already on caseload or in transition from hospital Appendix A Difficulty in carrying out daily tasks Post operative wound care requiring daily review Risk of falls (not within urgent and non routine ) Administration of injections - including Tinzaparin/Insulin Client / carer at risk of injury due to manual handling Issues with Swallowing Issues with communication due to health diagnosis Vocational rehabilitation – facilitation of return to work or study following diagnosis of neurological condition Cognitive rehabilitation Palliative re-assessment post routine admissions Facilitation of discharge from hospital e.g. attending discharge planning meeting Routine physiological assessment e.g. BP monitoring Psychological distress due to health condition RR – Rapid supported Discharge. Assessment for community IV antibiotics (1st dose to be administered in a supervised environment) Palliative care clients requesting rapid transfer to the community (Community Health Team to contact ward within 2 hours) Facilitation of discharge from ED of hospital (ie nonadmitted patients) whereby patient is at high risk of readmission (within 24 hours) NB: ward teams are expected to complete all necessary assessments and referrals required for safe discharge before the patient comes home. They should also provide sufficient notice to Community Health Teams and adult social care to ensure transfer to the community is seamless (as per Joint Hospital Discharge Policy). For example, nursing equipment e.g. hospital bed/pressure relieving mattress requires 3 working days. Page 2 of 2