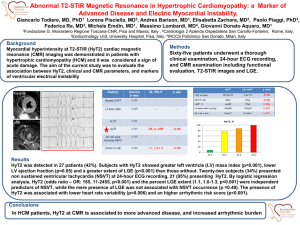
Table 2S. Patients` baseline characteristics. A
advertisement

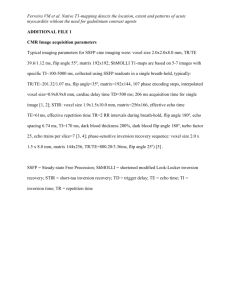
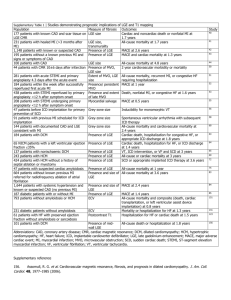
Supplementary material Full title: T1-mapping and outcome in nonischemic cardiomyopathy: all-cause mortality and heart failure Short title: T1-mapping and outcome in nonischemic cardiomyopathy First author: Valentina O. Puntmann Authors: Valentina O. Puntmann1-4*, MD, PhD; Gerry Carr-White2,3, MBBS, PhD; Andrew Jabbour5, MBBS, PhD; Chung-Yao Yu5, MBBS; Rolf Gebker6 MD, PhD; Sebastian Kelle6, MD, PhD; Rocio Hinojar1,2,7, MD, Mres; Adelina Doltra6, MD, PhD; Niharika Varma2,4, MD; Nicholas Child2,4, MBBS, PhD; Toby Rogers3,4,8, MD; Gonca Suna3,8, MD; Eduardo Arroyo Ucar2, MD; Ben Goodman2, MSc; Sitara Khan3,8, MD, PhD; Darius Dabir2,9 , MD; Eva Herrmann10, PhD; Andreas M. Zeiher1, MD, PhD; Eike Nagel1-4,11, MD, PhD, on behalf of International T1 Multicenter CMR Outcome Study Affiliations: 1 Department of Cardiology, University Hospital Frankfurt, Frankfurt-am Main, Germany Guys and St Thomas’ NHS Trust, London, United Kingdom 2 King’s College Hospital NHS Trust, Denmark Hill, London, United Kingdom 3 Department of Cardiac Imaging, King’s College London, United Kingdom 4 St Vincent’s University, Sydney, Australia 5 6 German Heart Institute Berlin, Berlin, Germany 7 Department of Cardiology, University Hospital Ramón y Cajal, Madrid, Spain Cardiovascular Division, King’s College London, London, UK 8 9 Department of Radiology, University of Bonn, Bonn, Germany 10 Institute of Biostatistics and Mathematical Modelling at Goethe University Frankfurt; Frankfurt am Main, Germany 11 Institute of Experimental and Translational Cardiac Imaging, DZHK Centre for Cardiovascular Imaging, Goethe University Frankfurt, Frankfurt am Main, Germany Methods Multicentre consortium A standardized T1-mapping acquisition and postprocessing protocol, developed and validated at King’ s College London, was distributed to participating centers and comparability as well as reproducibility were determined and optimized at each location for each field strength. Sequence specific reference ranges were established in healthy controls. In brief, a standardized T1-mapping acquisition protocol was adopted by participating centers with CMR expertize, which actively support their local clinical cardiology departments. The two UK sites contributed 409 (65%) subjects as the study, followed by Sydney (134, 21%) and Berlin (94, 15%). Delivery of clinical care was compliant with international guidelines and recommendations on patient management. The study has been registered with www.clinicaltrials.gov (NCT02407197). The primary diagnosis of DCM was made by the primary physicians in charge of clinical care. Echocardiography was the lead investigation of assessment of cardiac function and structure. In participating centres, CMR services are integrated into clinical routine and operate on a range of standard referral reasons, including: confirmation of the clinical diagnosis of DCM (cardiac volumes and function), assessment of the presence and extent of LGE, insight into underlying etiology (based non-ischaemic LGE patterns). Relevant clinical metadata were collected for all patients, as summarized in Table 1. All patients were stable at the time of inclusion with no change in regular medication in previous 6 weeks. None of the patients was considered for immediate device treatment (ICD, CRT or LVAD) at the time of the CMR study. None of the patients previously required an ITU admission or inotropic support. Competing risk analysis was performed by review of clinical data prior to inclusion in the study for likelihood of intervening events that could confound the main outcome (an active malignancy, active chemotherapy, etc). Patients with history of a previous malignancy were in remission > 24 months and discharged from further follow-up. We characterize the whole cohort in terms of their mortality risk from heart failure using the MAGGIC score, which is a generalizable easily used risk score for mortality in patients with HF, and includes 13 highly significant independent predictors of mortality in the following order of predictive strength: age, EF, NYHA class, serum creatinine, diabetes, beta-blocker, systolic BP, body mass index, time since diagnosis, smoking, chronic obstructive pulmonary disease, gender, and ACE-inhibitor or angiotensin-receptor blockers [19]. Cardiovascular magnetic resonance image acquisition All subjects underwent a standardized CMR protocol for routine assessment of cardiac volumes, mass and LGE imaging, at 1.5 or 3-Tesla (T) scanner equipped with advanced cardiac software, multi-transmit technology (3T only) and a 32-channel receiver coil (Achieva or higher, Philips Healthcare, Best, The Netherlands). All cine CMR were performed using a balanced steady-state free precession sequence in combination with parallel imaging (SENSitivity Encoding, factor 2) and retrospective gating during a gentle expiratory breath- hold (TE/TR/flip-angle: 1.7ms/3.4ms/60°, spatial resolution 1.8x1.8x8 mm). Late gadolinium enhancement was performed using gapless whole heart coverage of short axis (SAX) slices ~15 minutes after administration of 0.1 or 0.2 mmol/kg body weight gadobutrol (Gadovist®, Bayer, Leverkusen, Germany), as appropriate for the individual eGFR) [1], using a mid-diastolic inversion prepared 2-dimensional gradient echo sequence (TE/TR/flip-angle 2.0 msec/3.4 msec/25°, acquired voxel size 1.4x1.4x8mm) with an individually adapted prepulse delay to achieve optimally nulled myocardium. Balanced steady state free precession single breath-hold modified Look-Locker Imaging (MOLLI, (3(3)3(3)5)) was used for T1 mapping and performed in a single midventricular short axis slice at mid-diastole, prior to contrast administration and prior to LGE imaging, respectively (TE/TR/flip-angle: 1.64msec/3.3msec/50°, acquired voxel size 1.8x1.8x8 mm, phase encoding steps n=166, 11 images corresponding to different inversion times (3+3+5 MOLLI scheme), adiabatic prepulse to achieve complete inversion). Full sequence exam card is included at the end of this document (Table 1S). Image analysis Assessment of cardiac volumes and LV mass was performed following recommendations for standardized postprocessing using commercial software (CVI42®, Circle, Calgary, Canada). Endocardial LV borders were manually traced at end-diastole and end-systole. The papillary muscles were included as part of the LV cavity volume. LV end-diastolic (EDV) and endsystolic (ESV) volumes were determined using rule of discs. Ejection fraction (EF) was computed as EDV-ESV/EDV. All volumetric indices were normalized to body surface area (BSA). T1 measurements were performed using OsiriX® (Pixmeo, Switzerland)-based plug-in in a midventricular short axis (SAX) slice conservatively within the septal myocardium (septal) as well as in the whole SAX myocardium, as previously described and validated. Following offline image co-registration and motion correction, T1 values were determined by fitting a 2parameter exponential model to the measured data applying Look-Locker, noise and heart rate correction. Care was taken to avoid contamination with signal from the blood pool. Areas of LGE were excluded from the T1 region of interest. Statistical analysis Missing data for hematocrit was solved using multiple imputations based on regression method (SPSS V.22). Using this programme we first analyzed the existing data for the patterns and determined that the hematocrit values were missing in a random fashion. We used a set number of 5 imputations and chose the automatic method. We reviewed the iterations for variance. Means and variances of the pooled imputed hematocrit data were similar to the original (same for ECV original vs. the total using also the imputed). We also have tested the comparative strengths of predictions based on original and pooled data, which remained similar. A uni- and multi-variable Cox proportional hazards model was used for analyzing predictive associations of variables with the outcome. Univariable Cox regression models were fitted for each continuous predictor to test the assumption of linearity with the outcome. For T1 mapping measurements, this was performed per field-strength, as well for the whole cohort. Kaplan-Meier curves are used for visualizing the cumulative event free survival. A log-rank test was performed to compare event free survival curves in subjects for dichotomized variables. Collinearity in multivariable analysis was avoided by exclusion of variables, which suffered with interdependency between these same variables in its calculations (such as native T1 and ECV, or NYHA and MAGGIC score), as well as by grouping the role of different biomarkers in prediction of outcome as per their physiological meaning (i.e. tissue characterization of diffuse disease (by T1 mapping indices) vs. tissue characterization of regional disease (by LGE), vs. biomarkers of cardiac structure (EDV) vs. biomarkers of cardiac function (by EF). We used ‘the strongest of the group’ approach: we weighted the individual biomarker by individual Chi2/Wald values obtained in univariable analyses to select the strongest biomarker of the group (for example: tissue characterization of diffuse disease – T1 mapping indices-> native T1). Where there were more than 1 marker available, we only conducted analysis by the strongest predictor of the group, which allowed controlling for the interdependency of measures and collinearity effects on their individual prediction). Posthoc sample size analyses are performed as comparisons of rates for all cause mortality, using Post-hoc Power Calculator (http://clincalc.com/Stats/Power.aspx). For this we used dichotomized data for native T1 (normal/abnormal), as well as native T1 in lower-middle vs upper tertile, based on the present cohort of 637 subjects. Results Native T1 normal/abnormal Native T1 (tertiles) All cause mortality Univariable analysis LR Chi2 (p-value) Wald Adj HR (95%CI) Sig. (p-value) Multivariable analysis 1.5 T Model 1 <0.001 23.5(<0.001) Native T1 (septal)(per 10msec change) 27.1 1.1 (1.11-1.27) <0.001 Native T1 (septal)(per 10msec change) 14.2 1.1 (1.109-1.22) <0.001 ECV (%) 8.9 1.06(1.01-1.16) 0.002 15.8 1.1 (1.08-1.21) <0.001 18.6. 1.1(1.04-1.21) <0.001 9.0 1.06(1.01-1.16) 0.001 Model 2 3.0 T (n=280) Model 1 Native T1 (septal)(per 10msec change) ECV (per % change) 28.1(<0.001) 17.4 (<0.001) 23.2 (<0.01) Discussion The performance of ECV may have been reduced by the following 2 reasons: 1.) Hematocrit was unavailable in 15.9% of patients. In 45% of patients hematocrit was sampled on the same day. The most recent SCMR recommendations on ECV determination recommend hematocrit contemporaneous sampling at the time of CMR study. It must be noted, that a) this statement is not a guideline, b) this recommendation has been made on consensus of a scientific premise rather than on evidence of feasibility. Most importantly, the viability of this recommendation has not been tested in clinical practice. There is evidence for considerable variability of hematocrit measurement, due to within-subject biological variation (3%) and analytical variation (3%), which may explain a relative change of approximately 12% between two successive hematocrit values, measured with a time interval between 1 day and 1-2 months, in a normal healthy adult [2]. Whereas evidence in the presence of disease and medications is missing, there is evidence that methods used of one hospital vary from that of another [3,4]. Therefore, the point of care blood testing at the scanner appears to offer no alternative to the central laboratory testing (as used in this study) due to inherent high variability of hematocrit measurement. We conducted a prospective study in a clinical setting involving active clinical CMR imaging departments with high patient throughput. Although these were departments with dedicated CMR scanners, we found implementation of contemporaneous blood sampling/hematocrit measurement at the scanner impossible due to constraints on time and personnel without available specific research personal, resulting in higher costs of the CMR procedure. 2.) The results of T1 mapping indices are T1 mapping sequence dependent. For example, a very T1 accurate sequence will provide more information in the postcontrast values while missing important information in the native measurement, and conversely. As such, ECV by a T1 accurate method and ECV by the type of MOLLI, as used in the present study, may differ significantly in terms of information and may not be comparable. In the young field of T1 mapping research, details of all these aspects are relevant, and should not be limited to the research in phantoms, but provided by experience in a clinical setting, because many of these effects cannot be sufficiently understood by in vitro measurements. Investigators should be encouraged to report the data in full, as well as to include the details of sequences to clarify the different results, as a part of comprehensive clinical sequence characterization. Loss to follow-up is a major limitation of prognostic models. We observed 8% loss-to follow up, which is more than the observed deaths. This is partly a reflection of an increasingly mobile human population particularly affected by inclusion of London-sites. However, these subjects were on average similar to the overall cohort in terms of heart risk score (MAGGIC) and T1 mapping indices. Applying the similar rate of events as observed in the overall cohort we believe that we would have missed at the most 1.6 cardiac mortality event – which would not substantially change the results based on the overall cohort. LGE reflects extracellular accumulation of gadolinium contrast agent and it is visualized when the disease is sufficiently regionalized, allowing the contrast between one type of tissue to another. LGE is a marker of extracellular regional myocardial disease. In a defined clinical setting it corresponds to replacement fibrosis. In another setting it may also represent extracellular edema and other histological entities, with or without various amounts of cellular disruption. T1 mapping (outside LGE) is a quantifiable reflection of myocardial composition, including areas, which LGE cannot see based on its regionally defined scale. We strived to exclude LGE from T1 mapping ROIs by cross-referencing the images, especially in cases of midwall striae. Because midwall stria tend to be present in basal segments, they are usually out of the mid-SAX imaging plane and rarely problematic. Thus, the number of patients where the LGE poses an issue for the septal ROI is relatively small. The effect of non-ischaemic LGE is likely minimal, however this issue requires a systematic study, also across a range of LGE sequences [5]. References: 1. Reiter T, Ritter O, Prince MR, Nordbeck P, Wanner C, Nagel E, Bauer WR. Minimizing risk of nephrogenic systemic fibrosis in cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2012;14:31. 2. Thirup P. Haematocrit: within-subject and seasonal variation. Sports Med. 2003;33(3):231-43. 3. Lacher DA, Barletta J, Hughes JP. Biological variation of hematology tests based on the 1999-2002 National Health and Nutrition Examination Survey. Natl Health Stat Report. 2012;(54):1-10. 4. Banfi G1, Lombardi G, Colombini A, Lippi G. A world apart: Inaccuracies of laboratory methodologies in antidoping testing. Clin Chim Acta. 2010;411(1516):1003-8. 5. Puntmann VO, Voigt T, Chen Z, et al. Native T1 mapping in differentiation of normal myocardium from diffuse disease in hypertrophic and dilated cardiomyopathy. JACC Cardiovasc Imaging. 2013;6(4):475-84 Table 1S. Details of T1 mapping sequence parameters based on the exam card. 3(3)3(3)5MOLLI Nucleus = H1; Coil selection 1 = HRTorsoCardiacP; element selection = Coil selection 2 = element selection = All (16); HRTorsoCardiacA; All (16); Dual coil = yes; CLEAR = yes; Recon voxel size (mm) = 0.99; Reconstruction matrix = 400; SENSE = yes; P reduction (RL) = 2; P os factor = 1; Stacks = 1; slices = 1; fold-over direction = AP fat shift direction = F; Contrast enhancement = B-FFE offset frequency = balanced; 0; Acquisition mode = cartesian; Fast Imaging mode = TFE; shot mode = TFE startup echoes = (number) = single-shot; user defined; 10; B-TFE startup mode = lin. sweep up; shot interval = shortest; profile order = linear; Echoes = 1; TE = shortest; Flip angle (deg) = 50; TR = shortest; Halfscan = yes; factor= 0.60; Water-fat shift = minimum; RF Shims = adaptive; Shim = volume; ShimAlign = no; Fat suppression = no; Water suppression = no; TFE prepulse = invert; delay = (ms) = user defined; 300; T1 mapping = MOLLI 3-3-5; Cardiac synchronization = trigger; device = Cardiac frequency = ECG; 50; R-R window (%) = 10, 20; Number of heart phases = single phase; trigger delay = longest; Respiratory compensation = breath hold; Reference tissue = Cardiac muscle; Total scan duration = 00:18.0; Rel. signal level (%) = 100; Act. TR/TE (ms) = 3.3 / 1.64; Scan time / BH = 00:18.0; ACQ matrix M x P = 180 x 216; ACQ voxel MPS (mm) = 1.80 / 1.80 / 8.00; REC voxel MPS (mm) = 0.98 / 0.97 / 8.00; Scan percentage (%) = 100; TFE factor = 67; TFE dur. shot / acq (ms) = 259.0 / 219.7; TFE shot interval (beats) = 1; Min. TI delay = 92.5238037; Entered heartrate = 50; Trigger delay max. / act. (ms) = 1080.0 / 908.6; Max. heart phases = 3; Act. WFS (pix) / BW (Hz) = 0.393 / 1104.7; Min. WFS (pix) / Max. BW (Hz) = 0.391 / 1111.1; SAR / local torso = < 59 %; Whole body / level = < 0.9 W/kg / normal; B1 rms = 1.60 uT / 47 %; PNS / level = 47 % / normal; Table 2S. Patients’ baseline characteristics. A- demographic data, B-Cardiovascular magnetic resonance findings. Data is presented as median (interquartile range, IQR), comparisons *p-value of <0.05, **p<0.01. Comparison between groups was made for HF endpoint (a composite of HF death or unplanned HF hospitalization). Significance relates to the comparisons between patients that survived and died (p<0.05 is considered significant). BMI – body mass index, NYHA – New York Heart Association, GFR – glomerular filtration rate, SCD – sudden cardiac death; RAS- Renin-angiotensin-aldosterone system; MAGGIC integer risk score of survival in heart failure, as previously described [20]. LV – left ventricular, EDV – end-diastolic volume, ESV – endsystolic volume, EF-ejection fraction, RV-right ventricular, LGE- late gadolinium enhancement, SAX – short axis, ECV – extracellular volume fraction, T – Tesla. Results for patients with available haematocrit results only. A. Patients characteristics All patients No HF endpoint HF Endpoint Significance (n=536) (n=501) (n=62) (P-value) Age (years) 50(37-76) 49(39-74) 52(42-77) 0.36 Gender (male n,%) 332(62%) 295 (60%) 37 (60%) 0.95 BMI (kg/m2) 27(23-30) 27(23-30) 26(22-29) 0.70 Heart rate (bpm) 69(60-79) 69(60-78) 69(61-74) 0.72 127(113-139) 126(113-138) 131(119-141) 0.82 Systolic blood pressure (mmHg) Diastolic blood pressure (mmHg) 79(71-85) 77(69-84) 80(70-89) 0.86 Estimated GFR (mls/min/1.73m2) 79(76-81) 79(77-82) 77(64-79) 0.09 Haematocrit (%) 43(39-46) 44(39-45) 42(37-45) 0.33 Hypertension (n,%) 257(48%) 225(45%) 32 (51%) 0.43 Diabetes (n, %) 129(24%) 115(23%) 14 (22%) 0.85 Atrial fibrillation (n,%) 43(8%) 33(7%) 10(16%) 0.009 High cholesterol (n,%) 161(30%) 140(28%) 21(34%) 0.30 Smoking, current or previous (n,%) 150(28%) 127(25%) 23(37%) 0.03 Family history of cardiomyopathy or SCD 48(9%) 52(9%) 4(7%) 0.58 Alcohol excess (n,%) 70(13%) 68 (9%) 2(3%) 0.06 Chronic kidney impairment (n,%) 86(16%) 71(14%) 15(24%) 0.10 II 381(71%) 352(70%) 29(47%) <0.001 >III 155(29%) 122(24%) 33(53%) <0.001 13 (10-19) 13(10-18) 15(11-22) 0.005 NYHA functional class (n,%) MAGGIC score Medication RAS inhibitors 311(58%) 282(56%) 29(63%) 0.04 Diuretics 204(38%) 177(35%) 35(57%) <0.001 Beta-blockers 155(29%) 130(26%) 25(40%) 0.008 Calcium channel blockers 145(27%) 126(25%) 19(30%) 0.37 All patients No HF endpoint HF Endpoint Significance (n=536) (n=501) (n=62) (P-value) LVEDV index (mL/m2) 109(89-132) 101(91-125) 114(90-119) 0.04 LVESV index (mL/m2) 48(31-58) 44(30-55) 56(39-70) 0.07 LVEF (%) 47(29-50) 48(43-51) 44(34-48) 0.001 B. CMR quantification of function and structure LV mass index (g/m2) 88(62-98) 87(66-93) 94(63-107) 0.29 RVEF (%) 53(31-61) 55(49-61) 44(32-59) <0.001 145 (27%) 116 (24%) 29 (46%) <0.001 Midwall stria (n,%) 60(11%) 43(9%) 17(27%) <0.001 Epicardial (n,%) 21(4%) 17 (4%) 4 (7%) 0.25 Regional fibrosis (patchy), n%) 21 (4%) 18 (4%) 3(4%) 0.71 Diffuse (n,%) 43 (8%) 39 (8%) 4(6%) 0.57 6.2(2.1-9.5) 5.7(1.9-7.2) 8.1(3.2-11.4) 0.002 Native T1 (septal) (msec) 997(958-1056) 991(955-1012) 1052(1002-1081) <0.001 Native T1 (SAX)(msec) 962(842-1031) 959(898-1001) 978(926-1022) 0.06 Postcontrast T1 (msec) 439(397-483) 441(397-483) 429(401-471) 0.23 26(21-32) 26(22-30) 30(23-31) <0.001 CMR tissue characterisation LGE (present, n,%) LGE type LGE extent (% of LV volume) CMR T1 mapping 1.5 T (n=303) ECV (%) 3.0 T (n=233) Native T1 (msec) 1113(1064-1157) 1106(1057-1142) 1177(1106-1203) <0.001 Native T1 (SAX)(msec) 1058(958-1128) 1057(956-1104) 1079(968-1137) 0.04 Postcontrast T1 (msec) 441(401-489) 439(401-489) 429(411-488) 0.36 26(21-32) 26(21-30) 30(26-33) <0.001 ECV (%)