Development of Dried Plasmodium Alciparum Samples for Quality
advertisement
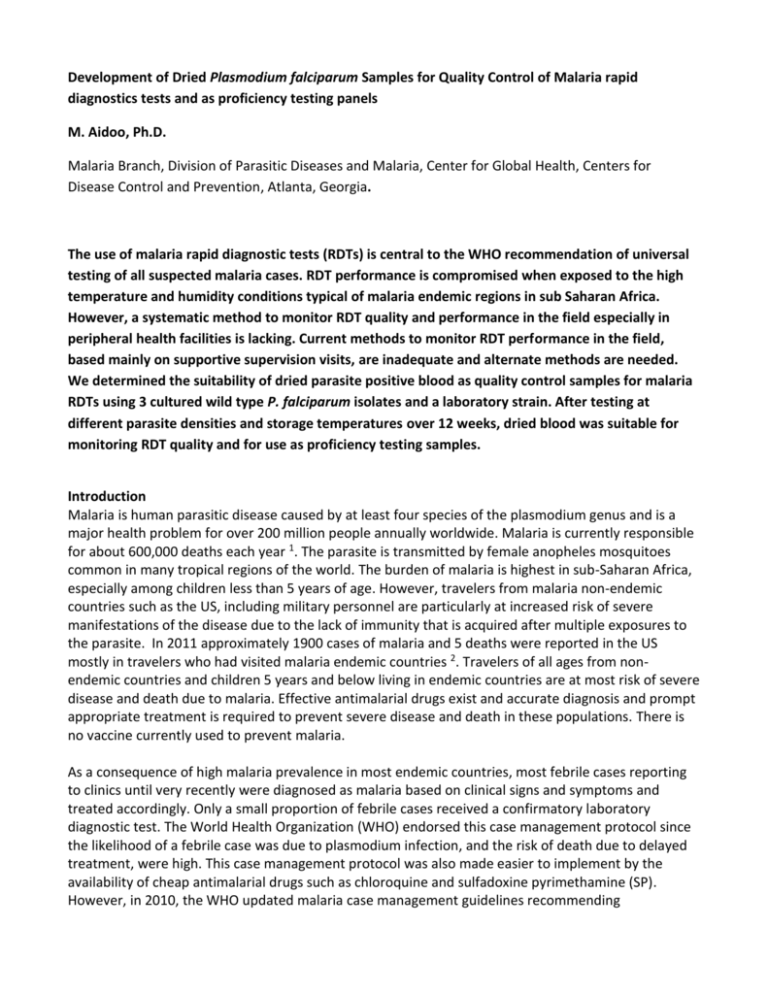
Development of Dried Plasmodium falciparum Samples for Quality Control of Malaria rapid diagnostics tests and as proficiency testing panels M. Aidoo, Ph.D. Malaria Branch, Division of Parasitic Diseases and Malaria, Center for Global Health, Centers for Disease Control and Prevention, Atlanta, Georgia. The use of malaria rapid diagnostic tests (RDTs) is central to the WHO recommendation of universal testing of all suspected malaria cases. RDT performance is compromised when exposed to the high temperature and humidity conditions typical of malaria endemic regions in sub Saharan Africa. However, a systematic method to monitor RDT quality and performance in the field especially in peripheral health facilities is lacking. Current methods to monitor RDT performance in the field, based mainly on supportive supervision visits, are inadequate and alternate methods are needed. We determined the suitability of dried parasite positive blood as quality control samples for malaria RDTs using 3 cultured wild type P. falciparum isolates and a laboratory strain. After testing at different parasite densities and storage temperatures over 12 weeks, dried blood was suitable for monitoring RDT quality and for use as proficiency testing samples. Introduction Malaria is human parasitic disease caused by at least four species of the plasmodium genus and is a major health problem for over 200 million people annually worldwide. Malaria is currently responsible for about 600,000 deaths each year 1. The parasite is transmitted by female anopheles mosquitoes common in many tropical regions of the world. The burden of malaria is highest in sub-Saharan Africa, especially among children less than 5 years of age. However, travelers from malaria non-endemic countries such as the US, including military personnel are particularly at increased risk of severe manifestations of the disease due to the lack of immunity that is acquired after multiple exposures to the parasite. In 2011 approximately 1900 cases of malaria and 5 deaths were reported in the US mostly in travelers who had visited malaria endemic countries 2. Travelers of all ages from nonendemic countries and children 5 years and below living in endemic countries are at most risk of severe disease and death due to malaria. Effective antimalarial drugs exist and accurate diagnosis and prompt appropriate treatment is required to prevent severe disease and death in these populations. There is no vaccine currently used to prevent malaria. As a consequence of high malaria prevalence in most endemic countries, most febrile cases reporting to clinics until very recently were diagnosed as malaria based on clinical signs and symptoms and treated accordingly. Only a small proportion of febrile cases received a confirmatory laboratory diagnostic test. The World Health Organization (WHO) endorsed this case management protocol since the likelihood of a febrile case was due to plasmodium infection, and the risk of death due to delayed treatment, were high. This case management protocol was also made easier to implement by the availability of cheap antimalarial drugs such as chloroquine and sulfadoxine pyrimethamine (SP). However, in 2010, the WHO updated malaria case management guidelines recommending parasitologic confirmation of all suspected malaria cases with a laboratory test before treatment 3 . This recommendation was made for several reasons. First, prevention efforts especially the widespread distribution of insecticide treated bednets had led to reductions in malaria prevalence in many endemic regions to the point where the majority of febrile cases presenting at clinics were no longer caused by plasmodium infection. Second, it had become necessary to switch anti-malarial drugs to efficacious but much more expensive artemisinin-based combination therapy (ACT) because of the development and spread of parasite resistance to chloroquine and SP. To help preserve the efficacy of ACTs, it was important to reduce drug pressure by preventing indiscriminate use as practiced with chloroquine and SP. Thirdly, laboratory testing for malaria, previously performed through microscopic examination of stained blood smears, became easier by the development of sensitive and specific rapid diagnostic tests (RDTs) that were simple and easy to use by most health workers with minimal training. Malaria RDTs are mostly lateral flow immuno-chromatographic tests with nitrocellulose strips on which parasite-specific antibodies are bound. These antibodies capture parasite antigens in the blood of infected persons and appear as colored bands on the strip. Tests can detect between 1 and 3 parasitespecific antigens. In addition to the parasite-specific antibodies, the nitrocellulose strips also contain antibody bands that capture human polyclonal antibodies and are incorporated on the strip as controls. This control serves as an indicator for flow of blood sample and conjugate mixture along the nitrocellulose strip, but is not necessarily an indication that the test is functioning optimally. A positive RDT result will have both the control and antigen-specific band showing, while a negative test shows only the control band. A test without the control band indicates an invalid, damaged or deteriorated test kit. The availability of sensitive rapid diagnostic tests made it possible to expand the availability of malaria testing to remote settings where such services did not exist. However switching to RDTs presented challenges associated with the lower level health facility settings under which they would be used. First, health workers without formal laboratory training such as village health volunteers, nurses and health officers were being asked to perform testing with minimal training and many quality assurance systems needed to be established to instill trust in test results. Second and more importantly, RDT sensitivity could be reduced when tests were stored for extended periods above manufacturer recommended temperatures which in most sub-Saharan Africa is the norm. In addition, many RDT brands suffer from high inter and intra batch variation and several quality measures are needed to assure the accuracy of test results. A multi-level quality assurance system addresses several aspects of the RDT use. The WHO in collaboration with CDC performs an extensive annual product testing program 4 to help address manufacturing quality. The next quality assessment step involves a pre-procurement quality lot testing program also conducted by the WHO and available free of charge to any country requesting the service. The pre-procurement lot testing program which is independent of manufacturer quality control performs quality control checks on each lot procured by countries. In addition to these upstream quality processes, WHO has guidance documents on methods to transport and store RDTs to preserve their quality at the point-of-care. Despite these quality measures, a systematic method for RDT quality control at the point of care in the field is not established. In the past WHO recommended a QC method that periodically compared RDT results to results from microscopic examination of stained blood smears from the same clinical specimen. This comparison was however inappropriate since RDTs identify parasites indirectly by detecting parasite antigens and microscopy detects actual parasites. As a result of this difference and because the parasite antigens detected by the RDTs can persist for several days after parasite clearance, RDT positive tests could be negative by smear microscopy in cases where patients have received anti-malarial treatment within a few days of being tested. In most of sub Saharan Africa where self-medication is common, paired RDT/microscopy samples for QC has limitations. Furthermore, a dearth of competent microscopists to accurately examine blood slides and the frequent shortage of reagents and supplies made this method of QC impractical in many places. Another QC method that requires a supervisor to observe how well health workers perform RDTs only assures the competence of the health worker and not the quality of the test. A simple method of preserving malaria parasite-infected blood as samples for quality control and proficiency testing of malaria RDTs is presented here. Most of this study has been reported elsewhere5. Methods Rapid Diagnostic Tests. Because RDT characteristics vary widely (over 200 kits available on the market), we selected 10 high-performing RDT products from 3 manufacturers (Table 1). All 10 RDTs had received high scores for performance in the WHO annual product testing. The RDTs detected an antigen specific to Plasmodium falciparum only (Histidine Rich Protein-2 or HRP-2) or a combination of HRP-2 and an antigen (plasmodium lactate dehydrogenase, pLDH) common to all Plasmodium species that cause malaria in humans. One RDT detected pLDH only. The same lot of each RDT product was used for all experiments with the exception of RDT 1 for which a different lot was used for the last time point of testing. Table 1. RDT Brands and their antigen specificity Dried P. falciparum infected Blood Preparation. Parasites used in the study included the 3D7 laboratory strain of P. falciparum and three in-vitro cultured P. falciparum isolates, Nigeria XII, PH 1, and FC27/A3. The cultured wild-type isolates were obtained from an ongoing sample collection program to support RDT evaluation and were obtained as frozen 50µl aliquots at 200 and 2000 parasites/µl. The 3D7 isolate was obtained from cultures at the CDC malaria laboratories. The cultures were harvested when 95% or more of the parasites were at the ring stage of parasite development and then diluted with parasite negative blood at the same hematocrit to the desired parasite density. For baseline reactivity, the frozen aliquots of parasites isolates were thawed at room temperature and tested on all the 10 brands of RDT. The 3D7 parasites from cultures were tested after dilution to the desired parasite concentration. After baseline reactivity was confirmed for all the samples on all 10 RDT brands, several replicates of 50µl aliquots were prepared and air-dried in a bio-safety cabinet. To confirm maintenance of reactivity after drying, representative samples of all the DTS were rehydrated with PBS Tween 20 solution and tested again on the 10 RDT brands. Sample vials were stored at 4 oC, at room temperature (~25oC) or in a dry incubator set at 35oC depending on experiment to be conducted (Figure 1). Figure 1. A schematic diagram of dried blood preparation Dried blood rehydration and RDT testing. Dried blood pellets in tubes were rehydrated with PBSTween 20 solution. On the day of testing, 50 µl (same as initial blood volume before drying) PBS-Tween 20 was transferred into DTS vials as needed and incubated for a minimum of 1 hour at room temperature for complete rehydration. After incubation, samples were gently mixed and tested on RDTs according the manufacturer’s instructions for each brand. For pilot testing, DTS for three parasite strains (Nigeria XII, PH 1, and FC27/A3) at 200 or 2000 parasites/µl and stored at 4oC, at room temperature (~25oC) or 35oC were tested after 1, 4 and 12 weeks of storage. At each time point, each of the 3 isolates at 200 and 2000 parasites/µl was tested for the 3 storage temperatures (total of 18 tests; 3 time points x 3 storage temperatures x 2 parasite concentrations). Tests were scored as negative (test band absent), positive (test band present), and weak positive (test band present but distinctly faint when compared to the control band). The control test band has to be positive for any test to be valid. A false negative test was defined as P. falciparum infected blood identified as positive by a test at baseline (before drying) and appearing as a negative test after drying. In addition to high temperatures, RDTs deteriorate when exposed to high humidity. Therefore, to prevent exposure to humidity, RDTs are packaged in airtight pouches. To test the utility of DTS in identifying failing tests, 8 mm diameter holes were punctured, one on each of the two sides of the pouch, on a subset of two RDT brands. Half of the punctured RDTs were stored at room temperature and the other half stored in an incubator set at 37 oC and 100% humidity. Intact RDTs were similarly stored. At time intervals 2 hrs., 6 hrs., 30 hrs., 2 weeks and 4 weeks DTS were tested on RDTs with punctured pouches to check for test deterioration. Intact RDTs were tested for comparison. DTS stability. To determine the stability of DTS over time, a panel of samples using P. falciparum laboratory strain clone 3D7 at 1000 and 2000 parasites/µl was produced. The parasite dilutions obtained were tested on 3 RDT brands to determine baseline reactivity and then distributed into 60 µl aliquots in tubes and dried as described above. After confirming retention of reactivity after drying, DTS were stored at 4oC and tested at irregular intervals for up to 2 years. Proficiency Testing. A PT panel consisting of 4 DTS with contents anonymized was given to technicians to conduct RDTs. In addition to scoring the final result, an assessment of how well the test was conducted was done with a 9-step checklist. Results DTS Pilot Testing. After 12 weeks of testing, 4 of the 10 RDT brands, all detecting the P. falciparumspecific antigen HRP2 maintained reactivity that was comparable to baseline reactivity with DTS at parasite concentrations of 200 and 2000 parasites/µl held at all storage temperatures and time points tested. Two RDT brands, both HRP2 tests, also maintained reactivity for all samples at both parasite concentrations at all temperatures and time points with the exception of specimens of the PH 1 strain at 200 parasites/µl when stored at 35oC for 12 weeks. The remaining 4 RDT brands lost reactivity in a total of 53 of 506 tests (10.5% false negative). These RDTs shared certain common characteristics. First, all 4 tests were combination tests designed to detect P. falciparum by the HRP2 antigen and the other three human malaria species by the pLDH antigen or all plasmodium species by pLDH only. Second, with the exception of Nigeria XII parasites at 2000 parasites/µl that were nonreactive with pLDH at one time point, on one RDT, reactivity was lost only for samples at 200 parasites/µl. In addition, for 3 of 4 RDTs that were combination tests detecting P. falciparum separately from other plasmodium parasites (HRP2 and pLDH as separate bands), reactivity was lost for pLDH and not HRP2 for 2 RDT brands (RDTs 2 and 10) at the low (200 parasites/µl) parasite density. Finally, weak baseline reactivity of the pLDH band was the single most predictive factor for loss of reactivity after drying blood. The latter characteristic is particularly exemplified by RDT 5, a pLDH only test, in which weak baseline test band intensity for all 3 parasite strains at 200 parasites/µl was predictive of non-reactivity after drying Effect of storage temperature and duration of storage on dried blood reactivity. Within the 12-week time frame of the testing, storage temperature did not appear to influence the reactivity of the DTS. For 4 RDTs brands, no loss in reactivity compared to baseline was observed. In some instances indications of storage temperature influencing DTS reactivity could not be confirmed. Loss of reactivity for one parasite isolate stored at 35oC was not associated with a loss of reactivity for another parasite stored at the same temperature and length of storage. For example, RDT 5 at week 1, using dried PH 1 at 200 parasites/µl was non-reactive for samples stored at 4oC and RT but reactive for the sample stored at 35oC. At week 12, the same sample was non-reactive for samples stored at 4oC and 35oC but reactive for the sample stored at RT. This result suggested test specific variation rather than DTS nonreactivity. Effect of parasite isolate on dried blood reactivity. At comparable parasite densities, similarly stored Nigeria XII and FC27/A3 but not PH 1 retained their reactivity on 8 of 10 RDTs implying a parasitespecific reactivity profile. Indeed, at 200 parasites/µl, baseline reactivity for PH 1 was weak or negative on 4 of 10 RDT brands. In addition, at 200 parasites/µl, PH 1 reactivity was weak for all storage temperatures at weeks 1 and 4. Sensitivity of Dried Blood Detection. Using the baseline result as the gold standard and combining results from all 3 parasites and storage conditions, all DTS at 2000 parasites/µl retained reactivity (100% sensitivity) on all 9 RDT brands that detect HRP2 (Table 2). At 2000 parasites/µl, sensitivity for pLDH (Pan) specific bands for 2 combination tests with pLDH bands separate from HRP2 bands was 100%. The sensitivities for the 2 remaining RDTs (RDTs 2 and 6) were lower at 80%. At 200 parasites/µl DTS stored at all temperatures and time points were detected at 100% sensitivity on 6 of 9 RDTs for HRP2. The sensitivity on 2 of the 3 remaining HRP2 detecting RDTs was 100% up to week 4 at all temperatures, dropping to 87.5% for week 12 samples stored at 35 oC. The mean sensitivity of dried blood detection for pLDH was low (29%, range 0-100%) at 200 parasites/µl. This low sensitivity was partly attributable to weak baseline reactivity on the pLDH bands on specific RDT brands DTS stability. Dried 3D7 at 1000 and 2000 parasites/µl stored at 4oC remained reactive after several weeks of storage (Table 3) with reactivity for both parasite densities for over 2 years. Utility of DTS for QC and PT. DTS were used to identify tests that were failing due to exposure to high temperatures and humidity with tests punctured to simulate failure showing reduced performance after only 30 hrs. of incubation at 37oC and 100% humidity (Table 4). Proficiency testing. Using a 9-step checklist during administration of the PT panel, errors were identified in the conduct of the test and in interpretation of faint test bands (Table 5). Table 2. Sensitivity of DTS detection using Table 3. DTS Long –Term Stability Testing Table 4. Punctures RDT test result showing deterioration after exposure to high temperatures and humidity. Time series experiments using punctured RDT pouches RDT 2 2 hrs Test 1 2 hrs Test 2 6 hrs Test 1 6 hrs Test 2 30 hrs Test 1 30 hrs Test 2 Week 2 Test 1 Week 2 Test 2 Week 4 Test 1 Week 4 Test 2 RDT 5 2 hrs Test 1 2 hrs Test 2 6 hrs Test 1 6 hrs Test 2 30 hrs Test 1 30 hrs Test 2 Week 2 Test 1 Week 2 Test 2 Week 4 Test 1 Week 4 Test 2 Punctured Intact Room Temperature C Pan Pf C Pan 4+ 4+ 4+ 4+ 3+ 4+ ND ND ND ND 2+ 2+ 2+ 2+ 1+ 1+ ND ND ND ND 3+ 3+ 2+ 2+ 1+ 2+ ND ND ND ND 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ Punctured Intact Room Temperature C T C T 4+ 4+ 4+ 4+ 4+ 4+ ND ND ND ND 2+ 2+ 2+ 4+ 2+ 2+ ND ND ND ND 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ 2+ 2+ 2+ 2+ 2+ 2+ 2+ 2+ 2+ 2+ 2+ 2+ 2+ 2+ 1+ 1+ 2+ 2+ 1+ 1+ Punctured Intact o Pf C Pan 3+ 3+ 2+ 2+ 2+ 2+ 2+ 3+ 2+ 2+ 4+ 4+ 4+ 4+ 4+ 4+ ± ± ± ± 1+ 1+ 1+ 1+ 1+ 1+ ± ± Neg Neg 37 C Humidified Pf C 2+ 2+ 2+ 2+ 2+ 2+ Neg Neg Neg Neg 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ Punctured Intact 37oC Humidified C T C T 4+ 4+ 4+ 4+ 4+ 4+ ± ± ± Neg 2+ 2+ 2+ 2+ 2+ 1+ Neg ± Neg ± 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ 4+ 2+ 2+ 2+ 2+ 2+ 1+ 2+ 2+ 2+ 2+ Sample used was dried 3D7 at 1000 parasite/µl. Punctured RDTPouches had two 8mm holes on each side of the pouch 37OC= humidified incubator set at 37OC Pan Pf 1+ 1+ 1+ 1+ 1+ 1+ 1+ 1+ 1+ 1+ 2+ 2+ 2+ 2+ 2+ 1+ 2+ 2+ 2+ 2+ Table 5. Two Examples of completed 9-Step Proficiency Testing Checklist Discussion Malaria RDT performance can be adversely affected by storage at temperatures above the manufacturer’s recommended range. According to manufacturer-provided product specifications, most RDTs require maximum storage temperatures not to exceed approximately 30oC, above which test performance may be compromised, especially if tests are stored for prolonged periods at such temperatures. In sub-Saharan Africa, ambient temperatures are frequently above 30 oC and therefore in peripheral health facilities where refrigeration is likely to be unavailable for cool storage of RDTs, high temperature exposure is expected to be common. The length of time a test has to be stored at the higher than recommended storage temperatures before performance is adversely affected is unknown and likely variable. Therefore, monitoring RDTs stored under such conditions is critical to assuring quality. Such test monitoring could be achieved by positive controls that are regularly used to test for RDT performance. Unfortunately, because positive controls do not exist and therefore are not provided as contents of the test kits, and malaria RDTs require fresh or frozen parasitized blood, field monitoring has largely been ignored as a component of a comprehensive malaria RDT quality assurance system. This is despite the importance of guaranteeing the quality of RDTs in peripheral health facilities where they are more likely to be used. The dried tube method tested here has been successfully used for preserving samples for HIV antibody detection6. The use of DTS as quality control samples appeared to be a feasible method for monitoring RDT performance. However, our results revealed that, for country-specific programs, standardization of the sample on the specific RDT to be monitored is critical to obtaining desired results. While DTS retained reactivity on 4 RDT brands irrespective of parasite isolate, parasite density, storage temperature and length of time stored, reactivity was lost on other RDTs dependent on one or a combination of these variables. Of note, detection of DTS by HRP2-specific tests or HRP2-specific test lines on combination tests was more consistent compared to pLDH bands as reported elsewhere 3. Essentially, DTS reactivity was test-dependent. For instance, at 200 parasites/µl, all 3 parasite isolates showed weak reactivity at baseline on RDT 5, a pLDH only test, while pLDH reactivity was lost for 2 of the 3 parasites on RDTs 6 and 10 both combination tests detecting HRP2 and pLDH. In addition to test-dependent differences, the parasite isolate also appeared to influence reactivity. At 200 parasites/µl, PH 1 was likely being recognized close to its detection limit that is conferred by the amount of HRP2 it produces. Irrespective of storage temperature and length of storage, PH 1 at this parasite concentration was associated with more weak or lost reactivity than the other parasite isolates irrespective of whether HRP2 or pLDH was the target antigen. Based on the parasite and test-dependent reactivity patterns, the use of dried blood requires characterization and standardization of the parasite isolate for the type of tests to be monitored. Strong baseline (prior to drying) reactivity at a required parasite density is critical to retaining dried blood reactivity after rehydration since weak baseline reactivity may suggest reactivity at the limit of detection of the test and slight intra-lot variations (well-documented among malaria RDTs) may result in loss of reactivity on some tests. No clear temperature-related loss of DTS reactivity was observed. However, the loss of reactivity of PH 1 at 200 parasites/µl stored only at 35oC for 12 weeks on RDTs 7 and 9 suggests a possible temperature effect and therefore prolonged DTS storage should be at cool temperatures. In addition to their utility as quality control samples, DTS were useful as proficiency testing panels for assessing health workers’ ability to perform RDTs and interpret results. DTS could therefore simultaneously be used for assessing the competency of health workers proficiency and overall test performance. Evaluation of this method for QC and PT is ongoing in 3 malaria endemic African countries. References 1. World Malaria Report 2013. Geneva, World Health Organization 2013. 2. Centers for Disease Control and Prevention. Malaria Surveillance — United States, 2011. MMWR 2013;62(No. SS-5) . 3. Guidelines for the Treatment of Malaria, Second Edition, Geneva, World Health Organization, 2010. 2010. 4. Malaria rapid diagnostic test performance - Results of WHO product testing of malaria RDTs: Round 4 5. Aidoo, M et al. 2012. Dried Plasmodium falciparum-infected samples as positive controls for malaria rapid diagnostic tests. Malar J. 11:239. 6. Parekh, B.S. et al 2010. Dried tube specimens: a simple and cost-effective method for preparation of HIV proficiency testing panels and quality control materials for use in resource-limited settings. J Virol Methods 2010, 163: 295-300.