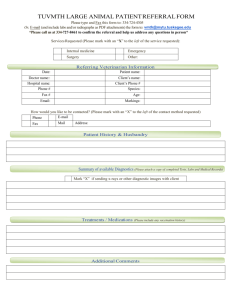
Upper GI
advertisement
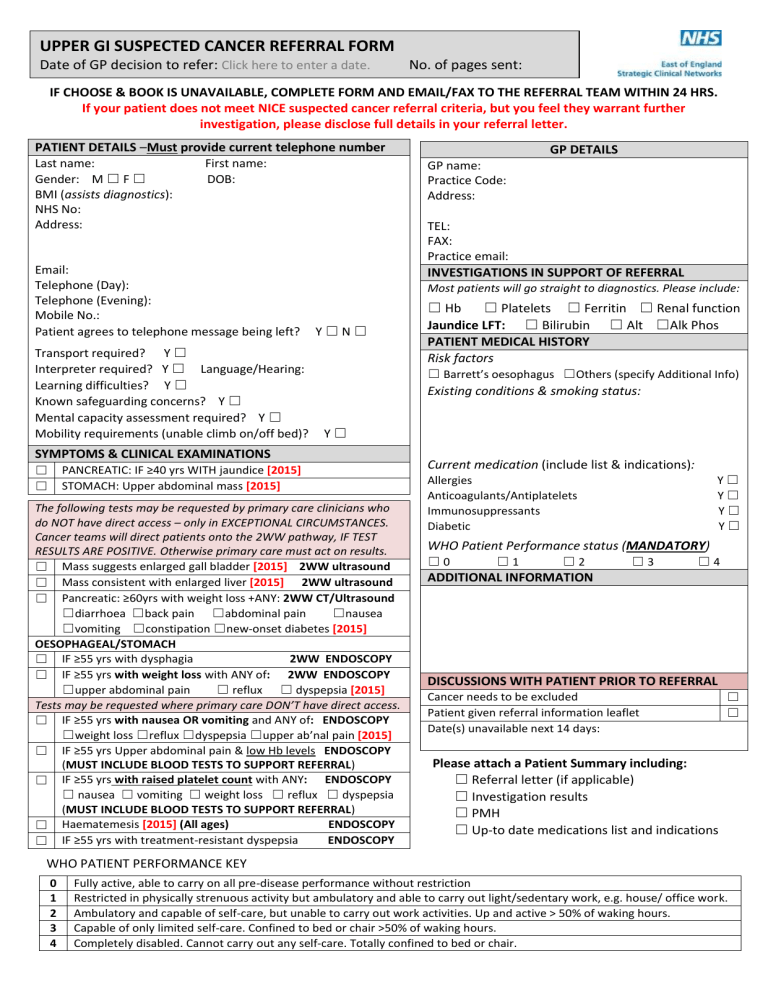
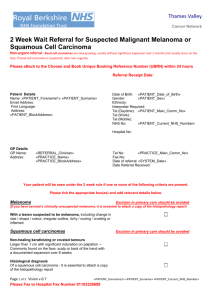
UPPER GI SUSPECTED CANCER REFERRAL FORM Date of GP decision to refer: Click here to enter a date. No. of pages sent: IF CHOOSE & BOOK IS UNAVAILABLE, COMPLETE FORM AND EMAIL/FAX TO THE REFERRAL TEAM WITHIN 24 HRS. If your patient does not meet NICE suspected cancer referral criteria, but you feel they warrant further investigation, please disclose full details in your referral letter. PATIENT DETAILS –Must provide current telephone number Last name: First name: Gender: M ☐ F ☐ DOB: BMI (assists diagnostics): NHS No: Address: Email: Telephone (Day): Telephone (Evening): Mobile No.: Patient agrees to telephone message being left? Transport required? Y ☐ Interpreter required? Y ☐ Language/Hearing: Learning difficulties? Y ☐ Known safeguarding concerns? Y ☐ Mental capacity assessment required? Y ☐ Mobility requirements (unable climb on/off bed)? TEL: FAX: Practice email: INVESTIGATIONS IN SUPPORT OF REFERRAL Most patients will go straight to diagnostics. Please include: Y☐N☐ ☐ Hb ☐ Platelets ☐ Ferritin ☐ Renal function Jaundice LFT: ☐ Bilirubin ☐ Alt ☐Alk Phos PATIENT MEDICAL HISTORY Risk factors ☐ Barrett’s oesophagus ☐Others (specify Additional Info) Existing conditions & smoking status: Y☐ SYMPTOMS & CLINICAL EXAMINATIONS ☐ ☐ GP DETAILS GP name: Practice Code: Address: PANCREATIC: IF ≥40 yrs WITH jaundice [2015] STOMACH: Upper abdominal mass [2015] The following tests may be requested by primary care clinicians who do NOT have direct access – only in EXCEPTIONAL CIRCUMSTANCES. Cancer teams will direct patients onto the 2WW pathway, IF TEST RESULTS ARE POSITIVE. Otherwise primary care must act on results. ☐ Mass suggests enlarged gall bladder [2015] 2WW ultrasound ☐ Mass consistent with enlarged liver [2015] 2WW ultrasound ☐ Pancreatic: ≥60yrs with weight loss +ANY: 2WW CT/Ultrasound ☐diarrhoea ☐back pain ☐abdominal pain ☐nausea ☐vomiting ☐constipation ☐new-onset diabetes [2015] OESOPHAGEAL/STOMACH 2WW ENDOSCOPY ☐ IF ≥55 yrs with dysphagia ☐ IF ≥55 yrs with weight loss with ANY of: 2WW ENDOSCOPY ☐upper abdominal pain ☐ reflux ☐ dyspepsia [2015] Tests may be requested where primary care DON’T have direct access. ☐ IF ≥55 yrs with nausea OR vomiting and ANY of: ENDOSCOPY ☐weight loss ☐reflux ☐dyspepsia ☐upper ab’nal pain [2015] ☐ IF ≥55 yrs Upper abdominal pain & low Hb levels ENDOSCOPY (MUST INCLUDE BLOOD TESTS TO SUPPORT REFERRAL) ☐ IF ≥55 yrs with raised platelet count with ANY: ENDOSCOPY ☐ nausea ☐ vomiting ☐ weight loss ☐ reflux ☐ dyspepsia (MUST INCLUDE BLOOD TESTS TO SUPPORT REFERRAL) ENDOSCOPY ☐ Haematemesis [2015] (All ages) ENDOSCOPY ☐ IF ≥55 yrs with treatment-resistant dyspepsia Current medication (include list & indications): Y☐ Y☐ Y☐ Y☐ Allergies Anticoagulants/Antiplatelets Immunosuppressants Diabetic WHO Patient Performance status (MANDATORY) ☐0 ☐1 ☐2 ☐3 ☐4 ADDITIONAL INFORMATION DISCUSSIONS WITH PATIENT PRIOR TO REFERRAL Cancer needs to be excluded Patient given referral information leaflet Date(s) unavailable next 14 days: ☐ ☐ Please attach a Patient Summary including: ☐ Referral letter (if applicable) ☐ Investigation results ☐ PMH ☐ Up-to date medications list and indications WHO PATIENT PERFORMANCE KEY 0 1 2 3 4 Fully active, able to carry on all pre-disease performance without restriction Restricted in physically strenuous activity but ambulatory and able to carry out light/sedentary work, e.g. house/ office work. Ambulatory and capable of self-care, but unable to carry out work activities. Up and active > 50% of waking hours. Capable of only limited self-care. Confined to bed or chair >50% of waking hours. Completely disabled. Cannot carry out any self-care. Totally confined to bed or chair. ALL AGES STOMACH: Upper abdominal mass [2015] (All ages) ≥ 40 YEARS PANCREATIC: IF ≥ 40 yrs with Jaundice [2015] ≥55 YEARS ANY OF THESE SYMPTOMS: OESOPHAGEAL/ STOMACH: haematemesis [2015] (All ages) OESOPHAGEAL/ STOMACH: IF ≥55yrs upper abdominal pain with low haemoglobin levels OESOPHAGEAL/ STOMACH: IF ≥55yrs with raised platelet count with any: nausea/ vomiting/ weight loss/ reflux/ dyspepsia/ upper abdominal pain ACTION: Urgent direct access Upper GI endoscopy WITHIN 14 DAYS (primary care must ensure result acted on) Anglia Addenbrookes Add-tr.nhsoutpatientreferrals@nhs.net TEL: 01223 586930 Bedford Hospital FAX: 01234 792133 Hinchingbrooke TEL: 01480 847557 hch-tr.cancerMDT@nhs.net Ipswich Hospital FAX: 01473 704120 James Paget FAX: 01493 453325 QEH, King’s Lynn FAX: 01553 613473 Norfolk & Norwich FAX: 01603 286876 Peterborough & Stamford FAX: 01733 678562 2wwreferrals@pbh-tr.nhs.uk West Suffolk Hospital wsh-tr.RapidAccess@nhs.net ACTION: Non-urgent direct access Upper GI endoscopy (primary care must act on result) OESOPHAGEAL/ STOMACH: IF ≥55yrs with nausea OR vomiting with any of: weight loss/ reflux / dyspepsia/ upper abdominal pain [2015] ACTION: Urgent direct access CT scan WITHIN 14 DAYS (primary care must ensure result acted on) SUSPECTED CANCER REFERRAL WITHIN 14 DAYS ≥ 60 YEARS ACTION: Urgent direct access ultrasound scan WITHIN 14 DAYS (primary care ensure result acted on) Beds & Herts East & North Herts FAX: 01438 284503 If you have not received acknowledgement within 48hrs (Mon-Fri) contact the 2WW supervisor on 01438 285206 OESOPHAGEAL/ STOMACH: IF ≥55yr with treatment resistant dyspepsia PANCREATIC: Weight loss AND any of: diarrhoea/ back pain/ abdominal pain/ nausea/ vomiting/ constipation/ newonset diabetes [2015] ≥ 60 YRS OESOPHAGEAL/ STOMACH: IF ≥55yrs with weight loss and any of the following: upper abdominal pain/ reflux/ dyspepsia [2015] OESOPHAGEAL/ STOMACH: IF ≥55yrs with dysphagia [2015] LIVER: abdominal mass consistent with an enlarged liver [2015] (All ages) GALL BLADDER: abdominal mass consistent with an enlarged gall bladder [2015] (All ages) Essex Basildon & Thurrock FAX: 01268 598066 cancer.2wwreferrals@btuh.nhs.uk Colchester Hospital University FT twoweek.waitreferral@nhs.net Luton & Dunstable FAX: 01582 497910 FAX: 01582 497911 West Herts Hospitals TEL: 01727 897199 Wherts-tr.twwreferrals@nhs.net Mid Essex Hospitals FT FAX: 012455 16751 Southend University Hospital FT FAX: 01702 508174