Blood Health Consultations - Minnesota Hospital Association
advertisement
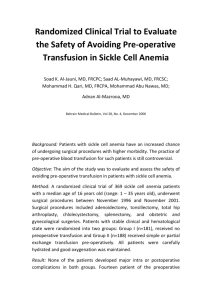
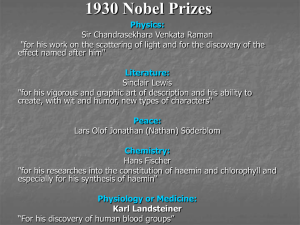
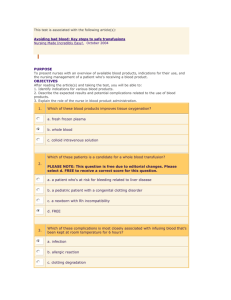
Blood Health Consultations Background: Pre-operative anemia is a problem of process, and it has significant negative implications for the patient and the hospital. Pre-operative anemia alone increases the risk for surgical complications, length of hospital stays, risk for surgical site and other infections, and increases risk for pulmonary and/or kidney injuries at a rate three times the non-anemic surgical person. Traditionally, patients have pre-operative exams too close to the day of surgery, making it difficult for the primary care physician to correct low blood counts pre-operatively. Blood transfusion is common in surgical patients, particularly in those with anemia on the day of surgery. Twenty-five percent of individuals having elective joint replacement surgeries are anemic. Too often, clinicians proceed to the operating room with anemic patients, having the mindset that post-operative transfusions will be used to assist recovery. As many as thirty percent of these “total joint” patients receive blood post-operatively, generally with two or more units of blood. Surgeon-specific transfusion rates range from 5% to 95% when controlled for same procedure types. Transfusion overuse has become so common place, that in 2012, the Joint Commission and the American Medical Association both designated the reduction of blood use as one of their collective top five care improvement initiatives. Innovation: In 2012, Fairview Southdale Hospital launched a pilot project in cooperation with pathologist, Katherine Frey, MD, and surgeons, John Anderson, MD, Edward Szalapski, MD, Joseph Teynor, MD, and Michael Nemanich, MD, all of Twin Cities Orthopedics. These surgeons collaborated to obtain pathologist driven blood health consultations and peri-surgical blood and anemia needs-planning for patients preparing to have elective joint replacement surgeries. Together they used a proprietary, IT-based, algorithmic program Dr. Frey developed, aimed at virtually assessing and managing these surgical candidates with pre-operative anemia and minimizing their need for post-operative blood transfusions. The program also provided outcomes reporting capabilities. In this pilot, all patients had their laboratory blood values assessed by Dr. Frey, and all patients received inpatient blood health care plans including a transfusion risk score. Pre-operative patients who were found to be anemic were also contacted to have additional lab tests obtained at lab sites closely located to the person’s home. When needed, anemia treatment was often accomplished pre-operatively via infusion therapy, again at convenient locations for the patient. Pathology consultations were also generated for the primary care physician, the surgeon, the hospital, and the patient, recommending best practice interventions to achieve optimum “blood health” peri-operatively. Results: Fairview Southdale Hospital implemented this pilot with a focus on improving patient care, on safely minimizing blood transfusions, on minimizing complications from poor blood health, and on avoiding unnecessary transfusion costs during one’s inpatient stay. Pre-Pilot Baseline: o 15.88% of patients with joint replacement surgeries at Fairview Southdale Hospital received transfusions and averaged 1.8 units per transfusion. Pilot results for 2012 - 2013: o Two hundred forty-six patients used this consultation service in 2012 through 2013. o 3.2% received blood transfusions and averaged 1.5 units per transfusion o Thirty-one fewer patients received blood than would have been expected o Fifty-eight fewer units of blood were used than would have been expected o Blood use appropriateness was reviewed and found to be at 100% vs. at 80% pre-study o There were no anemia related post-operative complications o Length of stay changes were not tracked in this pilot o Fairview Southdale Hospital realized a cost avoidance of $58,000 in this pilot group o Potential cost savings of $356,000 annually if all patients having joint replacement procedures were taken through this consultation process. Potential for Replication: Given these early results, and the fact that no additional physical space is needed to conduct this process, discussions are ongoing related to expanding this virtual pathology consultative service across the Fairview Health System. Nationwide, greater than three million patients having surgeries might benefit from such services. Conducting pre- and peri-operative blood health consultations has the potential to markedly reduce blood use across not only orthopedic surgery cases, but it may also benefit those individuals having certain, elective cardio-thoracic, gastro-intestinal, and gynecologic procedures. Using blood health consultation services as described here, could also assist hospitals in realizing improved quality outcomes, in lessening co-morbidities, and in enhancing cost savings.