Mucosal Lichen Planus: An Evidence

Mucosal Lichen Planus: An Evidence-Based Treatment Update
Parastoo Davari, Hui-Hua Hsiao, Nasim Fazel
Material and methods
Eligibility criteria
In this systematic review, we considered all published systematic reviews and randomized controlled trials (RCTs) of any design that evaluate the effectiveness of any intervention for the treatment of MLP. RCTs that compare at least one active treatment modality with a control group for treating MLP were included. The control group may be a placebo, no treatment, or an alternative therapy. All included RCTs confirmed diagnosis of MLP by clinical presentation and histopathology. Since histolopathological findings in genital erosive LP can be inconclusive,
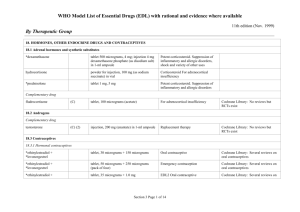
RCTs (n=1) of genital LP without histopathology confirmation were included as well. All treatment modalities including corticosteroids, retinoids, vitamin D3 analogues, calcineurin inhibitors, immunosuppressive agents, phototherapy, and biological agents were considered.
There were no language restrictions in this study. We considered all possible treatment modalities for non-Chinese articles. With regards to the Chinese articles, we limited this review to conventional medical therapies due to the large number of studies in traditional Chinese medicine.
Search strategy
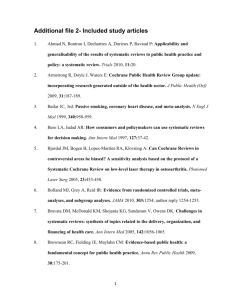
Pubmed (1950- November 1, 2012), EMBASE (1980- September 1, 2012), Cochrane Database of Systematic Reviews (Cochrane Reviews, Issue 8, August 2012), Database of Abstracts of
Reviews of Effects (Other Reviews, Issue 3, July 2012), Cochrane Central Register of
Controlled Trials (Clinical Trials, Issue 8, August 2012), Health Technology Assessment
Database (Technology Assessments, Issue 3, July 2012), and China National Knowledge
Infrastructure (CNKI) (1994 – March 2012) were searched using terms: “Lichen” and “Planus”.
The list of references for the included articles was searched as well.
Outcome measures
The primary outcome was the improvement of symptoms of MLP lesions after 4-8 weeks of treatment. The secondary outcomes include clinical improvement based on the signs, complete resolution of signs and/or symptoms after 4-8 weeks, and side effects of the drug. Other endpoints were reported if these outcomes were not available. Electronic Supplementary
Material 2 demonstrates the Preferred Reporting Items for Systematic Reviews and Meta-
Analyses (PRISMA) flowchart of the study.
Methodological quality assessment of included studies
We chose the following criteria to rank the methodological quality of each RCT: existence of randomization, adequate explanation of the sequence generation for randomization, adequate elaboration of allocation concealment, proper blindness methods, calculation of sample size, checking for comparability of baseline data, performing intention to treat analysis, and patient follow-up after treatment period. We considered a trial as high quality if the study qualified for equal or more than half of the criteria. All other studies were rated as “moderate” quality.
“Quality of Evidence” and “Strength of recommendation” of modalities
We evaluated the “Quality of Evidence” and also “Strength of Recommendation” for each modality using "The American College of Physician” Guideline grading System. Additionally, since many of the modalities have only one randomized controlled trial, we grade the recommendation as “insufficient evidence to determine net benefits or risks.” Evidence may be conflicting, of poor quality, or lacking such as very low sample size (less than a total of 20 after data pooling) per modality.
Meta-analysis
The meta-analysis was performed, if needed, using Review Manager version 5.1.6. The results of dichotomous outcomes were presented as odds ratio (OR) and 95% confidence intervals
(CI). I² statistic was utilized to determine statistical heterogeneity. We explored the reasons for heterogeneity if I² statistic was more than 50% for the primary outcome. We reported the results of meta-analysis if the I² statistic was less than 80%.