Final Adults Nursing Process Paper
advertisement

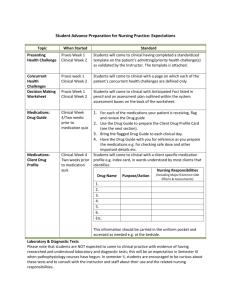
Running head: NURSING PROCESS PAPER Nursing Process Paper Jerel Hershberger Kent State University 1 NURSING PROCESS PAPER 2 Introduction The purpose of this paper is to take a patient that I had cared for on the clinical floor and put together a research paper on the patient from a holistic standpoint. This process paper describes the medical diagnosis, all lab work and diagnostic tests, my assessment of the patient, treatments, a concept care map of the patient, medications the patient is taking, and nursing diagnosis, goals, interventions, and desirable outcomes. This patient was chosen because of her interesting past medical history and her current medical diagnosis. I will describe the patient as PR. Client Profile PR is a female patient that is sixty-eight years old. She is a very pleasant but frail lady with a weight of one hundred six pounds, five feet five inches tall, and a calculated BMI of 17.6. PR has a social history of actively smoking one to two packs per day and denies alcohol use. Time of the assessment and patient care was on September 18, 2012. She was admitted on September 17, 2012 through the emergency department with abdominal pain, nausea and vomiting. PR was diagnosed with complete small bowel obstruction which is blockage in the small intestines. Normally the fluid in the bowels is reabsorbed, but with bowel obstruction the bowels partially retain the fluid which can cause distention. Beatrice Harold writes in the Emergency Nurse (2011) that patients with bowel obstruction can become hypovolemic due to vomiting, poor fluid intake, and fluid that is retained in the bowel lumen and not reabsorbed as normal. This can cause a decrease in blood volume and can lead to hypotension, hypovolemic shock, and diminished renal and cerebral blood flow (Black & Hawk, 2009). Signs and symptoms of bowel obstruction is abdominal pain, abdominal distention, vomiting, and sometimes peristaltic waves NURSING PROCESS PAPER 3 can be visible (Black & Hawk, 2009). Assessments of the vital signs should be made immediately (Harold, 2011). PR also has a current diagnosis of an Abdominal Aortic Aneurysm (AAA). AAA is an out-pouching of the wall of the descending aorta in the abdominal region. AAA is caused by the weakening of the musculoelastic middle layer of the arterial wall, usually caused by plaque build-up or cholesterol deposits (Brunner & Sommers, 2011). Over time, as the pulsating blood rushes through the aorta, the vessel wall becomes increasingly weak, and the aneurysm can enlarge (Brunner & Sommers, 2011). The enlargement and weakening of the vessel wall can become extremely dangerous. Signs and symptoms may include a pulsating abdominal mass. A bruit may also be heard on auscultation of the abdomen (Brunner & Sommers, 2011). Severe back and abdominal pain, decrease in blood pressure, increase in pulse, increase in respirations, and pain, pallor, absent pedal pulses, and paresthesia in the lower extremities are all signs of aneurysm rupture (Brunner & Sommers, 2011). PR has an extensive past medical history. The history includes the following: AAA, Anxiety Disorder, severe Chronic Obstructive Pulmonary Disease (COPD), Lumbar Disc Disease, Depression and Anxiety, long Tobacco history, Hypertension, Hyperlipidemia, Osteoporosis, Peripheral Vascular Disease (PVD), and prior extremity Deep Venous Thrombosis (DVT). Looking at the list of the past medical history, the history of long tobacco use may have had significant impact on her health. Tobacco use may be a cause or part of the cause of her development of COPD, hypertension, PVD, hyperlipidemia, and AAA (Centers for Disease Control and Prevention, 2012). The past surgical history for PR is as follows: Aortofemoral bypass, appendectomy, hysterectomy, and a vaginal and bladder suspension. PR also has a list of allergies. The allergies are Augmentin, Penicillins, Cephalosporins, Lincosamides, NURSING PROCESS PAPER 4 Betalactams, Carbapenem, Streptokinase Analogues, Alterplase, Clindamycin, Clavulanic Acid, Potassium Clavulanate, Amoxicillin, Retavase. PR presented to the Emergency Department on September 17, 2012 with abdominal pain. The ED reported she had been vomiting about a dozen times the previous three days, has pain in the epigastrium, is nauseous, but has no abdominal swelling. Assessment Upon initial report from the night nurse, PR was alert and oriented times three. She had complaints of some abdominal spasms, was on two liters of oxygen nasal cannula. PR was up with one assist. Nasogastric tube was to continuous wall suction. PR was medicated for pain with morphine early in the morning at 0530. PR was on routine I&O and was NPO except for medications. PR was a pleasant and cooperative lady. For the head-to-toe assessment findings refer to table one below. Table 1 Assessment Data Assessment Vital Signs Neurological Musculoskeletal Findings BP – 165/79 Oral Temperature – 98.6 Radial Pulse – 82 Respiration Rate – 14 Pulse Ox – 98% on 4L NC Pain – 0 A&O X 3 LOC – active Speech – clear PERRLA – pupils 3mm and brisk Facial Expressions – symmetrical Shoulder Shrugs - Strong Upper Extremities – Strong and full ROM Lower Extremities – Weak bilaterally Gait – Unsteady NURSING PROCESS PAPER Cardiac Respiratory Vascular Gastrointestinal Genitourinary IV Site Output Intake Braden Scale 5 Hand Grasps – Strong Bilaterally Generalized Weakness – Mild S1 and S2 noted No murmurs noted Respiration Rate – Regular Breath Sounds – Clear, decreased in bases bilaterally Cough – Occasional nonproductive cough Oxygen – 2L NC humidified Skin – Warm and dry, no paleness or cyanosis Mucous Membranes – Pink and moist Capillary Refill – Less than 3 sec Pulses – Radial and brachial +2 bilaterally Pedal Pulses - +1 bilaterally Edema – None SCD – Removed Abdomen – Soft and flat Bowel Sounds – Hypoactive Emesis – None NG Tube – Yes in right nare to continuous wall suction at 25mm Hg, secretions are dark brown liquid Pain – None on palpation Last Bowel Movement – 1 week ago from admission Catheter – Foley inserted on 9/17/12 Urine Assessment – Amber urine Output on Shift – 700ml Foley Site – Free of redness Left antecubital - #20 gauge Site free of redness without swelling and drainage Urine – 700ml NG – 250ml Parenteral – 713ml Amount of Free Text – 139ml NG – 360ml Moisture – 4 Mobility – 3 Activity – 4 Nutrition – 1 Friction and Shear – 3 Total Braden Score - 15 Treatments An oral contrast dye was administered through the NG tube for a CT that was ordered. This was for an abdominal CT to view the bowel obstruction. I was not on shift for the results of NURSING PROCESS PAPER 6 the CT. Continuous wall suction for decompression of the stomach was administered. PR was on continuous two liters nasal cannula oxygen and incentive spirometry every one hour while awake was also ordered. Lab Information and Diagnostic Tests For a complete list of the lab work for PR, refer to tables two through four below. The following tables will give arterial blood gases (ABG’s), CBC, and electrolytes. The table will show the test, normal ranges, patient results, and the relevance for this specific patient. Table 2 Arterial Blood Gases Test pH Normal Values 7.35 – 7.45 Patient Results 7.37 pCO2 35 – 45 mm Hg 68.7 mm Hg O2 75 – 100 mm Hg 51 mm Hg HCO3 22 – 26 mEq/L 38.5 mEq/L BE +1 - -2 10.0 Normal Values *5,000 – 10,000/mm3 Patient Results 12.2/mm3 Relevance to Patient Patient is within normal range but slightly acidosis. Patient has CO2 retention because of COPD. Lack of diffusion across alveolar wall from COPD/ hx. of smoking. Patient may be hypoxic. Kidney’s compensating for respiratory acidosis. High volume of base compensating for increased CO2. (Cavanaugh, 2009) Table 3 Complete Blood Count (CBC) Test White Blood Cells (WBC) Relevance to Patient Increase WBC can indicate presence of infection, may be NURSING PROCESS PAPER 7 Red Blood Cells (RBC) Hemoglobin *4.2 – 5.4 million/mm3 *12 – 16 g/dl 4.12 million/mm3 Hematocrit *38 – 47% 37.6% Platelets *150 ,000 – 450,000/mm3 140,000/mm3 11.7 g/dl related to COPD, small bowel obstruction as well. Patient is just below norm. Age may have Slightly below normal. Could cause slight anemia. Slightly below normal. This could cause decrease in clotting, as caused by heparin. *indicates female values (Cavanaugh, 2009) Table 4 Electrolytes Test Sodium Na+ Potassium K+ Normal Values 135 – 145 mEq/L 3.5 – 5.0 mEq/L Patient Results 144 mEq/L 3.3 mEq/L Chloride ClBlood Urea Nitrogen (BUN) Creatinine 95 – 105 mEq/L 5 – 20 mg/dL 99 mEq/L 8 mg/dL 0.6 – 1.2 mg/dL 0.710 mg/dL Glucose 70 – 110 mg/dL 136 mg/dL (Cavanaugh, 2009) Diagnostic Tests Relevance to Patient Within normal range. Low K+. Administer K+ and monitor for muscle weakness, dysrhythmias. May be result of NPO status, and fluid buildup in abdominal region. Within normal range. Within normal range. Good renal function. Within normal range. Good renal function. Slightly elevated. May be because of continuous D5% RL. 136 mg/dL is not a critical level. NURSING PROCESS PAPER 8 The following are diagnostic tests on PR such as Ultrasounds, Chest X-ray, Computed Tomograhy (CT), Echocardiogram, and Venous Doplex Studies. These are tests that were current up to the end of my shift. Refer to table five for a complete study of these tests. Table 5 Diagnostic Tests Test Ultrasound of Abdominal Aorta Date 9/08/2011 Ultrasound of Abdominal Aorta 3/20/2012 Chest PA/AP Lateral 9/17/2012 Computed Tomography (CT) of Abdominal and Pelvis Region 9/17/12 Echocardiogram 9/17/12 Venous Doplex Study of Both Legs Administration of Oral Contrast Dye for Computed Tomography of Abdomen 9/18/12 9/18/12 Patient Findings and Relevance Focal aneurismal dilation involving the midto-distal aorta. Measures 4.4cm in anteroposterior dimensions and 3.8cm in transverse dimensions. Aorta is atherosclerotic. Sonographic images of the abdominal aorta demonstrate diffuse atherosclerotic plaque. Aneurysmal dilation of the distal abdominal segment. Lungs are emphysematous. Aorta calcified and mildly tortuous. Complete small bowel obstruction identified in small-mid. Fusiform infrarenal abdominal aortic aneurysm measuring 4.6 cm transverse dimensions. Slight ascites. Aortic valve is mildly sclerotic. Not enough to be aortic stenosis. All other findings normal. No evidence of deep or superficial venous embolisms. Administration of 500ml of oral contrast dye through nasogastric tube. This treatment will help show the small bowel obstruction. The ultrasounds show the history of PR’s growing Abdominal Aortic Aneurysm. The results also show atherosclerosis of the aorta as well. The results of the Echocardiogram also show a mildly sclerotic aortic valve. This may be relevant with the history of hyperlipidemia. This patient will need to have frequent ultrasounds on the abdominal region to monitor the growth of the aneurysm, and may need to eventually have surgery to fix the aneurysm. The CT NURSING PROCESS PAPER 9 scan shows the complete small bowel obstruction. This explains PR’s lack of bowel movements. Fluid can also accumulate in the intestine because of the obstruction which is why the slight ascites was seen on the CT scan (Brunner & Sommers, 2011). This can cause a loss of fluid for the patient, and may cause fluid volume loss. It is important to keep PR hydrated with IVs. Medications For a complete list of medications that PR was prescribed refer to table six below. You will find the medication’s name, purpose, route, dose, class, side effects, and the reason PR is taking the medication. Table 6 Medications Medications Purpose Albuterol Sulf Used as a bronchodilat or for asthma or COPD Fluticason/salmeter Decreases ol inflammatio n and causes bronchdilatio n Tiotropium Long-term Bromide maintenance tx. of brochospasm in COPD Hepairn Sodium Prevention of thrombus formation Clonidine HCL Used for mild to moderate Route, Dose Class Side Effects 2.5mg INH q4hr prn 1 puff INH 2 times daily Bronchodilator Nervousness, restlessness, chest pain, palpitations Headache, N/V, palpitations 18mcg INH q day Bronchodilator Tachycardia, dry Anticholinergic mouth 5000 Units Anticoagulants Bleeding, pain at infection site 0.1mg TD q7 days Antihypertensi ve Drowsiness, dry mouth, bradycardia Long Acting Beta-2 Agonist, Corticosteroid Reason patient is taking medication History of COPD History of COPD History of COPD Imobility from being hospitalized and prior DVT, PVD History of hypertensio n and AAA NURSING PROCESS PAPER 10 hypertension Protonix Treatment of GERD 40mg IV q day Proton pump inhibitors Headache, abdominal pain Methylprednisolon e SOD SUCC Used systemically and locally in chronic diseases 30mg IV q day Corticosterioid Peptic ulceration, hypertention, thromboembolis m, adrenal suppression Headache, constipation, diarrhea Zofran Prevention 4mg IV of nausea q6hr and vomiting prn Antiemetic Ativan Decreases anxiety by depressing CNS 1mg IV 3 times daily PRN Antianxiety, sedative, hypnotics, analgesic adjuncts Dizziness, drowsiness, apnea, lethargy Dextrose 5% RL Provides hydration and calories Caloric sources, carbohydrates Fluid overload, hyperglycemia Morphine sulfate Reduces severe pain 1000ml IV at 70ml/h r 2mg IV q4hr prn Opioid analgesics Respiratory depression, constipation, sedation, confusion 20mg/h r Bronchodilator Arrhythmias, tachycardia, nausea, vomiting, seizures, anxiety Aminopheline Long term control of reversible airway obstruction caused by COPD (Deglin & Vallerand, 2012) For GERD, relieve acidic regurgitatio n from bowel obstruction Decreases inflammator y response in chronic COPD PRN med for N/V from bowel obstruction History of anxiety disorder, anxiety of being in hospital Caloric source because of NPO status For pain reported by patient greater than 5 on VAS scale History of severe COPD NURSING PROCESS PAPER 11 Nursing Diagnosis Table 7 Care Plan Nursing Diagnosis Risk for fluid volume deficit related to vomiting upon admission secondary to complete bowel obstruction AEB… - No bowel movement for 1 week - NG to continuous wall suction - Strict NG output recorded - Decreased Potassium of 3.3 - Ascites on CT secondary to bowel obstruction Short-term Goal Patient will maintain blood pressure within patient’s normal range and show no manifestations of dehydration in next 12 hours. Long-term Goal Patient will maintain fluid balance as evidenced by balanced measuring intake and output and monitory lab electrolyte balance within normal lab ranges in next 48 hours. Interventions/Rationales 1. Monitor patient’s vital signs every 4 hours. a. Note presence and degree of postural BP changes, observe for temperature elevations or fever. b. Tachycardia is present along with a varying degree of hypotension depending on degree of fluid deficit. 2. Maintain patient’s fluid balance by administering parenteral fluids with sodium chloride, bicarbonate, and potassium added as ordered. a. Monitor electrolyte lab data. 3. Monitor (check) patient’s urinary output hourly. a. Measure or estimate fluid losses from all sources (i.e. NG tube, foley, diaphoresis). b. Fluid replacement needs are based on correction of current deficits and ongoing losses. 4. Palpate patient’s peripheral pulses, note capillary refill and skin color and temperature every 4 hours. a. Conditions that contribute to extracellular fluid deficit can result in inadequate organ perfusion to all areas and may cause circulatory collapse and shock. Evaluation/Outcomes Evaluation of goals could not be determined because the student’s shift ended before the goal’s time frame. Appropriate outcomes of the goals are electrolyte and acid-base balance, fluid balance, and hydration. If goals are met, teaching of oral hydration of 4 12oz cups of water per day and report to physician if there is a drop in BP and pulse, or a decrease or increase in urine output. Reference/Evidence(Black & Hawk, 2009) based Research (Doenges, Moorhouse, & Murr, 2010) NURSING PROCESS PAPER 12 Table 8 Care Plan Nursing Diagnosis Impaired Gas Exchange related to decreased ventilation secondary to history of severe COPD/emphysema AEB… - 2L O2 NC to maintain SpO2 at 98% - Decreased lung sounds at bases bilaterally - History of smoking 1-2 packs per day - ABGs – pO2-51; pCO2-68.7 Short-term Goal Patient will maintain pulse ox of greater than 92% with 2L O2 NC or less for next 1 week. Long-term Goal Patient will maintain adequate gas exchange as evidenced by ABG values at baseline for next 1 month. Interventions/Rationales 1. Monitor the patient’s respiratory rate, pattern, and pulse oximetry every 4 hours, ABG results, and manifestations of hypoxia and hypercapnia. a. Prompt recognition of deteriorating respiratory function can reduce potentially lethal outcomes. 2. Administer low-flow oxygen therapy (1-2 L/min) as needed via nasal cannula. a. Oxygen corrects existing hypoxemia. 3. Assist the client into the high-Fowler position. a. The upright position allows full lung excursion and enhances air exchange. 4. Administer bronchodilators as ordered. Monitor for side effects. a. Bronchodilators relax bronchial smooth muscle, facilitating air flow. Common side effects include tremor, tachycardia, and other cardiac dysrhythmias. Evaluation/Outcomes Evaluation of goals could not be determined because the student’s shift ended before the goal’s time frame. Appropriate outcomes of the goals are adequate Acid-Base balance, Ventilation, and Gas Exchange. If goals are met, home-going patient teaching of effects of smoking, deep breathing, and coughing would be appropriate interventions. Also monthly physician check-ups for pulmonary functions would be appropriate. Reference/Evidence(Black & Hawk, 2009) based Research NURSING PROCESS PAPER 13 References Black, J.M. & Hawks, J.H. (2009). Medical-surgical nursing: clinical management for positive outcomes. (8th ed). St. Louis: Sounders Elsevier Inc. Brunner, L.S. & Sommers, M.S. (2011). Diseases and disorders: a nursing therapeutics manual. (4th ed.). Philadelphia: F.A. Davis Company. Cavanaugh, B.M. (2009). Nurse’s manual of laboratory and diagnostic tests. Philadelphia: F.A. Davis Company. Centers for Disease Control and Prevention. (2012). Smoking and tobacco use. Retrieved from http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smokin g/ Deglin, J.H., & Vallerand, A.H. (2012). Davis’s drug guide for nurses. (12th ed.). Philadelpia: F.A. Davis Company. Doenges, M.E., Moorhouse, M.F. & Murr, A.C. (2010). Nursing care plans: Guildelines for individualizing client care across the life span. (8th ed.). Philadelphia: F.A. Davis Company. Harold, B. (2011). Urgent treatment of patients with intestinal obstruction. Emergency Nurse, 18(11), 28-31. Retrieved from web.ebscohost.com.proxy.ohiolink.edu