Zyvox® Prior Authorization Worksheet
New York State Medicaid Clinical Drug Review Program
Instructions
Program Information
Drugs included in the Clinical Drug Review Program (CDRP) require prior authorization.
A list of CDRP drugs is available at www.nyhealth.gov and at http://newyork.fhsc.com.
Fax requests are NOT permitted for some CDRP drugs.
Prescriber Procedure
If your fax includes the standardized fax form, only the Member Name, ID, DOB, and Clinical
Criteria need to be completed and faxed as an attachment to process your request.
PA requests from 3rd party agencies to include faxes or any media are not allowed. Please have the
prescribing physician or an agent employed by the prescribing practitioner contact our department
for consideration of this request.
Additional documents required for approval include the following:
Documentation of culture and sensitivity results
Clinical notes, lab results, and documentation of the original diagnosis from an Infectious
Disease Specialist must be included with this fax form.
Complete Blood Count (CBC) results
Following review of all of the required information, you will be contacted by the Clinical Support Center
regarding prior authorization for Zyvox®.
Prior Authorization Call Line 1-877-309-9493
For billing questions, call 1-800-343-9000.
For clinical concerns or Clinical Drug Program Review questions, visit www.nyhealth.gov and
http://newyork.fhsc.com or call 1-877-309-9493.
Note: Processing May Be Delayed if Information Submitted is Illegible or Incomplete.
© 2013, Magellan Health Services, Inc. All Rights Reserved.
Magellan Medicaid Administration
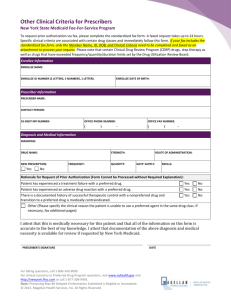
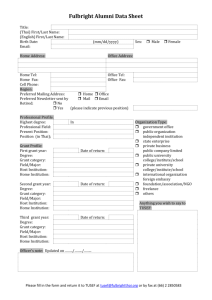
Zyvox® Prior Authorization Fax Form
If your fax includes the standardized fax form, only the Member Name, ID, DOB, and Clinical Criteria need to be
completed and faxed as an attachment to process your request.
Enrollee Information
ENROLLEE NAME:
DATE OF BIRTH:
ENROLLEE MEDICAID ID NUMBER (2 LETTERS, 5 NUMBERS, 1 LETTER):
Prescriber Information
PRESCRIBER NAME:
CONTACT PERSON:
PRESCRIBER 10-DIGIT NATIONAL PROVIDER IDENTIFIER (NPI):
OFFICE PHONE NUMBER:
OFFICE FAX NUMBER:
Clinical Criteria
NAME:
Zyvox® (linezolid)
STRENGTH:
DIRECTIONS:
QUANTITY1:
NEW PRESCRIPTION:
Yes
No
IF NO, DATE THERAPY INITIATED:
EXPECTED LENGTH OF THERAPY2:
DIAGNOSIS2:
DATE OF LAST EVALUATION FOR THIS DIAGNOSIS2:
What is the medication being prescribed for?
Were cultures and sensitivities performed confirming the diagnosis?
Yes
No
(If YES, please include a copy of the culture and sensitivity results.)
If NO, what is the clinical rationale for prescribing Zyvox® without performing culture and sensitivities?
Are you, or have you consulted with, an Infectious Disease Specialist for this patient?3
Yes
No
Prescriptions for Zyvox® are limited to a 14-day supply. Continuation beyond 14 days of therapy will require a new
prescription and a new PA number.
2 Diagnosis and length of therapy will be reviewed by a Clinical Pharmacist and/or Medical Director.
3 Clinical notes, lab results, and documentation of the original diagnosis from an Infectious Disease Specialist must be
included with the fax form.
1
Note: Processing May Be Delayed if Information Submitted is Illegible or Incomplete.
Revision Date: February 8, 2016
Prior Authorization Call Line 1-877-309-9493
For billing questions, call 1-800-343-9000.
For clinical concerns or Clinical Drug Program Review questions, visit
www.nyhealth.gov and http://newyork.fhsc.com or
call 1-877-309-9493.
Page 2
Magellan Medicaid Administration
Zyvox® Prior Authorization Fax Form
Was the patient recently hospitalized for the diagnosis you provided?
Yes
No
If YES, was Zyvox® started in the hospital?
Yes
No
Were there other antibiotics used to treat this diagnosis?
Yes
No
(If YES, provide all medications used and reason for discontinuation.)
Medication History
Please provide at least a three-month history of medication use.
Medication Trial/Previous
Therapies
Date of Therapy
Start Date
End Date
Strength
Frequency
Reason for
Discontinuation
Has the total duration of therapy with Zyvox®, including treatment in an inpatient setting, exceeded 14 days?
Yes
No
(If YES, please include a copy of the CBC taken after the patient initiated Zyvox® treatment.)
According to the Zyvox® prescribing information, myelosuppression (including anemia, leukopenia, pancytopenia, and
thrombocytopenia) has been reported in patients receiving Zyvox®. Complete Blood Counts (CBCs) should be monitored
weekly, particularly in patients receiving Zyvox® for longer than two weeks.
If YES, what is the rationale for exceeding 14 days of treatment?
Please be aware that The U.S. Food and Drug Administration (FDA) has received reports of serious central
nervous system (CNS) reactions when Zyvox® is given to patients taking psychiatric medications that work
through the serotonin system of the brain (serotonergic psychiatric medications). For more information
and a list of the serotonergic psychiatric medications that can interact with Zyvox®, please visit
http://www.fda.gov/Drugs/DrugSafety/ucm265305.htm.
Attestation
I attest that Zyvox® is medically necessary for this patient and that all of the information on this form is
accurate to the best of my knowledge. I attest that documentation of the above diagnosis and medical
necessity is available for review if requested by New York Medicaid.
PRESCRIBER SIGNATURE
DATE
Note: Processing May Be Delayed if Information Submitted is Illegible or Incomplete.
Revision Date: February 8, 2016
Prior Authorization Call Line 1-877-309-9493
For billing questions, call 1-800-343-9000.
For clinical concerns or Clinical Drug Program Review questions, visit
www.nyhealth.gov and http://newyork.fhsc.com or
call 1-877-309-9493.
Page 3