Poster Abstracts - St. Louis Children`s Hospital
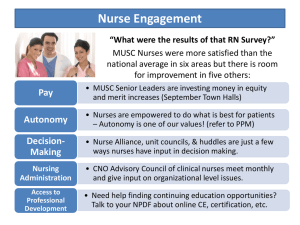
advertisement
Title of Poster A Pediatric Patient Drive Airway Clearance Protocol: Standardization of Practice Based on Evidence Name of Primary Presenter and Credentials Holly L. Lehmuth, B.S. Employer Name, City and State St. Louis Children’s Hospital, St. Louis, Missouri ABSTRACT Background: Providing timely and appropriate delivery of respiratory care for patients requiring airway clearance is critical in managing the care of pediatric patients. Both delays in care and errors occur due to inefficiencies with the current process. Patient driven protocols for respiratory management of pediatric patients have been cited in the literature as one method to improve safe, timely and effective care for these patients. This information led to the following PICO question: For pediatric patients requiring airway clearance, would the implementation of a respiratory patient driven protocol compared to traditional physician order entry result in decreased time to treatment and increased provider confidence in administering the protocol. Methods: The literature was reviewed and a multidisciplinary project team was formed. Guidelines from the American Association for Respiratory Care and other studies were appraised. A new therapist driven protocol for airway clearance was developed based on the best available evidence. Pre-implementation data was gathered to reflect the time from admission until airway clearance orders were obtained and a confidence survey was administered to the respiratory care team to assess their confidence in utilizing a protocol. Respiratory therapists were educated on how to utilize the new protocol prior to a three month pilot of the practice change. Anticipated Outcomes: The pilot will be implemented in fall 2014 and data gathered for six months. Anticipated outcomes include a reduction in the time from admission to delivery of initial airway clearance treatment and an increase in the confidence level of respiratory therapists in implementing a therapist driven protocol. Implications: Implementation of standardized practice protocols can lead to better patient outcomes and professional development opportunities for respiratory therapists. Title of Poster Tantrums, Gagging and Food Refusals: What’s a Parent to Do? Interdisciplinary Feeding Team Treatment of Feeding Disorders Name of Primary Presenter and Credentials Janet Hamill MOT, OTR/L. Kasey Davis PsyD, ABPP Jeanne Saavedra MHS, CCC-SLP Tara Todd RD, LD Employer Name, City and State St. Louis Children’s Hospital, St. Louis, Missouri ABSTRACT Background: Children with feeding disorders have complex and multifaceted needs that extend beyond the focus of a single care provider. Without coordinated care there is a risk of contradictory and confusing advice, creating missed opportunity. The Interdisciplinary Feeding Team, unique in the St. Louis area, provides a coordinated evaluation and management plan for the child. The poster presentation describes team members’ roles, interactions and methods of intervention with focus on interdisciplinary coordination and implementation of treatment. Implications: The creation of a seamlessly integrated team approach provides the family with a plan that prioritizes the patient’s needs and accounts for the family’s lifestyle and resources. Families who utilize this team have usually tried various approaches previously without success; anecdotal feedback during and following treatment is often positive. Improvements in growth, nutrition, core diet, social interactions and family dynamics have been reported by families. Follow up with relevant team members provides the opportunity to address hurdles and adjust the treatment plan for continued progress. Title of Poster Photovoice as an Intervention to Decrease Injuries in Children Name of Primary Presenter and Credentials Mary P. Curtis, PhD, MSN, BSN Employer Name, City and State Goldfarb School of Nursing, Barnes-Jewish College, St. Louis, Missouri ABSTRACT Background: Mothers play a valuable and critical role in the prevention of accidents and injuries in their children. The purpose of this pilot project was to evaluate the use of Photovoice as an innovative communitybased participatory education and research intervention to empower mothers to help identify potential hazards in their own homes and in the community environment. Methods: Participants were asked to photograph potential hazards in their home and complete their own home safety assessment. They were then interviewed by the community nurse educators who reviewed the pictures. Transcripts were reviewed using qualitative description. Results: Four themes emerged: increased awareness of home environment, empowerment for change, learning by doing, and a desire to acquire a safe home environment for their children. Results indicate that using Photovoice as an educational intervention has the potential to be a useful tool in teaching injury prevention to families with children. Title of Poster An Evidence-Based Transition Program for Adolescents with Sickle Cell Disease Name of Primary Presenter and Credentials Emily Yates, MSN APRN PCNS-BC, CPN Employer Name, City and State St. Louis Children’s Hospital, St. Louis, Missouri ABSTRACT Background: Patients with sickle cell disease (SCD) are cared for in our hospital for many years and develop close relationships with health care staff. As these patients near adulthood, the need to transition to an adult care center becomes imminent. This is a difficult transition physically, psychologically and emotionally for patients and families. They are reluctant to leave the pediatric setting that has coordinated provision of medical, social work and psychological services. There are fewer adult physicians specializing in the care of SCD patients so finding a provider is difficult. Our hospital has created successful transition programs for cystic fibrosis and oncology patients but none had yet been developed for SCD patients. This led to the following PICO question: For adolescent patients with SCD, would a transition program based on developmental readiness result in a successful move into an adult care setting? Methods: Two staff nurses from the inpatient unit assembled a multidisciplinary team to create a transition program. The team examined evidence related to timing of transition and chose an approach based on developmental readiness. Presently there is a monthly outpatient clinic dedicated to adolescent education about SCD complications. The team will attain baseline data on individual knowledge about complications and pediatric psychologists will take the lead in determining developmental readiness. Nursing representatives from the adult hospital and our team are coordinating a process to transfer care. Roadmaps will be created for each patient and family to communicate progress and help the staff know what steps are yet needed. Evaluation of the program will be determined through monitoring of medical appointment adherence, hospital admissions, emergency room visits and patient satisfaction. The program will be initiated in November 2014. Anticipated Outcomes: A transition program based on developmental readiness is expected to meet the needs of this population. Title of Poster A Pediatric Transfer Call Center: Serving the Community and the Hospital Name of Primary Presenter and Credentials Katherine Schmitz, RN, MHI, MPH, MSW, BSN Employer Name, City and State St. Louis Children’s Hospital, St. Louis, Missouri ABSTRACT Background: Delivery of nursing care begins with the initial telephone call placed by a physician or community hospital requesting admission or direct transfer for a patient. Prior to the creation of our pediatric transfer call center, the process was the sole responsibility of the chief resident and resulted in a delayed admission or transfer and no readily accessible documentation. In an effort to provide a seamless patient referral process that supports the continuum of care, our nurses, physicians, and administrators examined various transfer call programs throughout the country. Methods: A pediatric transfer call center was developed and is available to the community 24 hours a day, seven days a week. The call center is staffed by experienced pediatric nurses who have the ability to recognize the unique needs of children and families. Providing high quality nursing care during the pre-admission process was identified as critical for an environment that positively influences patient outcomes. The transfer process includes consultations between physicians, activation of the transport team, securing bed placement, patient report for the admitting nurse and physician, and follow-up calls to the outlying hospital. A pre-admission document is generated, providing real time patient updates. Additional services provided by the call center include: urgent or routine consults, callbacks to primary physicians regarding admitted patients, maternal/fetal consults and transfers, coordination of after-hour radiology requests, clinic appointments and registration for classes and conferences offered by the hospital. Results: Data collected since 2010 strongly indicates the success of the transfer call center in supporting improved patient outcomes and the health of the community we serve. Learning Objectives: 1. 2. Discuss the need for expert nursing care during the pre-admission process Describe the key elements required for development of a transfer center that meets community needs. Title of Poster I Need How Many Shots?: Compliance in Newly Arrived Refugee Children Name of Primary Presenter and Credentials Kimberly Ewing, BSN, RN Employer Name, City and State St. Louis Children’s Hospital, St. Louis, Missouri ABSTRACT Background: Each year the United States opens its borders to nearly 70,000 refugees. Unlike immigrants, refugees have fled their country to escape danger or persecution. Many of these newly arrived families come into the United States without medical records. It is required that individuals begin receiving immunizations as soon as possible. The vaccination process has long been an overwhelming and stressful one for families. Cultural and language disparities faced by refugees made compliance with the complicated immunization schedule difficult. The hospital’s Healthy Kids Express mobile health team offers a monthly clinic at the International Institute for this population. Available space and resources are limited to a predetermined number of children. Staff noticed a significant number of children were being scheduled for visits during which only one immunization was given. Scheduling a child for only one immunization could lead to as many as 8 visits to achieve complete vaccination. This discovery prompted the team to take a closer look at what they could do to improve efficiency at every appointment. Methods: Nurses collaborated with other programs involved in the acclamation of the families. The care team included patient & family, resettlement agency, case worker, school, and nursing. Focus was on patients 7-18 using a catch-up immunization schedule. By rearranging and standardizing immunizations offered at each visit it was possible to limit the total number of visits to 4. A visual tool was developed to simplify the complicated process of catching up on immunizations. The tool outlined the immunizations and how many visits each child would need. Goals were: 1. To show the family the vaccination process could be completed in as little as 4 visits 2. To increase the completion rate of required and recommended vaccinations Through a retrospective chart review, the number of visits each patient required to complete the immunization process was determined. Special attention was given to patients who exceeded the four visit mark. The percentage of patients needing ≥ 5 visits before immunization completion was gathered per year starting in 2009. Patients included for the study had a least two visits and not to exceed eight visits. Patients with only one visit were excluded from data. Results: Prior to implementation of the scheduling tool 33% of patients required ≥ 5 visits to become fully immunized. After implementation there was a 18% decrease in the number of patients who needed ≥ 4 visits. Less than 15% of the total number of patients seen needed ≥ 4 visits in 2013: down 50% from 2012. Implications: Developing a scheduling tool reduced the number of visits needed for full immunization. This benefited the program in several ways: Families spent fewer days at clinic appointments allowing children to spend more time in school The limited space available for appointments at the once monthly clinic was maximized thus allowing more children access The design of the tool allows the consenting nurse to show the family at the initial visit the required number of immunizations and visits for vaccine completion The benefits extended into unexpected areas such as education: This partnership not only increased understanding of when a family needed to return for immunizations but also relayed the “in progress” immunization status to the school Title of Poster Integration of Pediatric Nurse Practitioners as Hospitalists: Foundation for the Future Primary Presenter and Credentials Cheryl Grave, RN, CPNP Employer, City and State St. Louis Children’s Hospital, St. Louis, Missouri ABSTRACT Background: The role of the hospitalist pediatric nurse practitioner (HPNP) developed from three forces converging together: Responding to the changes to resident education limiting work hours and availability for patient care Needs of the changing pediatric healthcare environment The Institute of Medicine (IOM) and Robert Wood Johnson Foundation’s (RWJF) “Future of Nursing: Leading Change, Advancing Health” (2010) report The IOM and the RWJF were tasked with to identifying and responding the role of nursing in the changing healthcare landscape. The most transformational outcome of the 2010 report is the call to advance the practice of nursing the fullest of one’s education and training. Our institution integrated Pediatric Nurse Practitioners (PNPs) into the hospitalist team on a busy general medicine unit to answer all three of these forces and improve the overall care of patients and their families Methods: Pilot Unit consisted of a 32-bed inpatient unit. The population included general medicine, sickle cell disease, rheumatology, infectious disease, and genetics averaging 5,600 patient days per year with 1,830 admissions. Talent Acquisition Considerations included: Character seen as important as clinical skills Education and formal preparation Interest in inpatient care Willingness to work nights, weekends, holidays Experience with in-patient medicine Comfortable with ambiguity Hospitalist PNP Preparation for the role included: Nursing & Intern orientation Physician champions along with the pediatric residency program provided key education Extensive shadowing experiences Results: Measures indicate that high quality care for patients and families has been the primary outcome Improved family centered rounds Increase continuity of care for patients, families and staff Improved equity among healthcare providers Increased opportunities for Hospitalist PNP development through participation in the APRN Council and safety initiatives Outcome data supported expansion to other inpatient units as well as increase in number of Hospitalist PNPs on the unit Implications: The changing healthcare landscape has created an opportunity for nurses to shape the future. The creation and implementation of the Hospitalist PNP role demonstrates a strong bridge between the past and future of nursing. Relying strongly on the nursing framework in the development, implementation, and enhancements of the HPNP role set the foundation for the creation of a dynamic, innovation solution for the future. Title of Poster Tracheostomy Emergencies Simulation Training for Home Care Nurses Name of Primary Presenter and Credentials Jodi Carter, MSN, RN, CPNP Employer Name, City and State Washington University School of Medicine, St. Louis, Missouri ABSTRACT Background: The number of children discharged to home with tracheostomy tubes and mechanical ventilators has increased significantly over the past two decades. These children are at risk of life-threatening emergencies that require prompt recognition and intervention by trained caregivers. For this reason, most hospital programs require a minimum of two caregivers be trained on the child’s care prior to discharge, including tracheostomy cardiopulmonary resuscitation. Skilled home nursing care is often arranged to support the family in caring for their child. In our experience, families often report that the home care nurses lack the skills needed to provide safe care to their children. Our goal was to develop an educational program on tracheostomy emergencies for the home care nurse. Methods: Study design was a pre-test/post-test format and a confidence scale. Home care nurses were provided with two hour didactic lesson on the home ventilator followed by two hours of simulation training using high fidelity mannequins. The focus was on common tracheostomy emergencies, including: accidental decannulation, tracheostomy obstruction, difficult reinsertion, and water lavage. Each scenario was followed by a debriefing. Preliminary Results: 22 nurses enrolled with data collection completed on 14 nurses. Average test scores increased by 12% after training. Overall confidence scales increased in 57% of the nurses. Implications: Simulation is a feasible and desired teaching method. Home care nurses are in need of resources for improving their skills for tracheostomy and ventilator emergency situations suggested by our preliminary data.