Cate: Birth Claims
advertisement

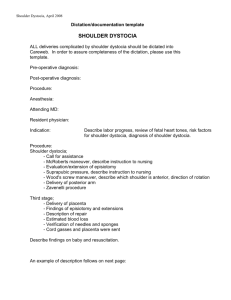
SHOULDER DYSTOCIA: PLAINTIFFS’ THEORIES AND DEFENSE STRATEGIES By: Rodney Cate Hand Arendall, LLC 11 North Water Street RSA Tower, Suite 30200 Mobile, Alabama 36602 Email: rcate@handarendall.com Direct Dial: (251) 694-6274 INTRODUCTION Shoulder dystocia is an obstetrical emergency occurring when the fetus’s shoulder becomes lodged beneath the mother’s pubic bone causing the fetus to become stuck just prior to delivery. The obstetrician must react quickly to effectuate the delivery to prevent an hypoxic event. In a typical shoulder dystocia lawsuit, the damage to the fetus is a brachial plexus injury, which typically results in paralysis, temporary or permanent, to the fetus’s arm. This paper discusses shoulder dystocia, accepted delivery protocols, plaintiffs’ lawyers’ theories and strategies for defense. SHOULDER DYSTOCIA - BACKGROUND Shoulder dystocia results from the failure of the fetal shoulders to deliver spontaneously. The fetal head is delivered but the baby’s anterior shoulder gets stuck behind the mother’s pubic bone. This typically results in the “turtle sign,” when the fetal head retracts back toward the uterus resulting in the baby’s cheeks puffing out. The baby remains stuck in this position until the anterior shoulder is released. Shoulder dystocia is an obstetrical emergency because the umbilical cord can get trapped or compressed resulting in decreased or cessation of oxygen to the brain. When injury does occur to the baby, the injury is typically a brachial plexus injury resulting in either transient or permanent damage or paralysis to the baby’s impacted arm. The brachial plexus is the area where the nerve roots controlling movement of the arm attach to the spinal cord. Erb’s palsy results from a stretching of upper nerves or avulsion of upper nerve roots C5 through C7. Klumpke’s palsy results from damage to the lower nerves or roots C8 through T1. 2 Although some obstetrical literature describes brachial plexus injuries occurring in the absence of shoulder dystocia, the prevailing view is brachial plexus injuries occur as a result of excessive lateral traction on the head of the baby away from the impacted shoulder. Some traction on the fetal head is typically required in any delivery. With shoulder dystocia, a greater amount of traction on the fetal head may be necessary to effectuate the delivery. A stretching or avulsion of the brachial plexus nerves can occur when lateral traction is placed on the baby’s head in attempting to effectuate delivery. No movement occurs as the baby’s shoulder is stuck, resulting in a stretching or tearing of the nerve roots from the spinal cord to the arm. Shoulder dystocia has been reported to occur in 0.6% to 2.4% among vaginal deliveries of fetuses in the vertex presentation.1 It has been reported that the incidence of brachial plexus injuries following a delivery complicated by shoulder dystocia varies widely from 4% to 40%.2 Of the 4% to 40% of deliveries complicated by shoulder dystocia with a reported brachial plexus injury, fewer than 10% of those cases of shoulder dystocia result in persistent brachial plexus injury.3 MANAGEMENT OF SHOULDER DYSTOCIA Once there is recognition of shoulder dystocia, typically from the turtle sign, the obstetrician should first ask for help from a second obstetrician and extra personnel. Because of the risk of an hypoxic-ischemic event, a delivery room nurse should note the time on the fetal heart strip when the shoulder dystocia has occurred and alert everyone in the room as to the elapsed time. ACOG has developed a patient safety checklist for documenting the significant events occurring during the delivery following shoulder dystocia. Initially, the obstetrician should attempt gentle 1 ACOG Practice Bulletin, Clinical Management Guidelines for Obstetricians-Gynecologists, Number 40, November 2002. 2 Id. 3 Id. 3 traction with assisted maternal efforts to deliver the baby. Whether to perform an episiotomy is a clinical decision made by the obstetrician. Reports are inconclusive as to the effectiveness of an episiotomy. If delivery is unsuccessful, the first suggested maneuver is known as the McRoberts maneuver. McRoberts consists of removing the legs from the stirrups and sharply flexing the thighs up onto the abdomen in an attempt to rotate the symphysis pubis toward the maternal head and decrease the angle of pelvic inclination. This does not result in an increase in pelvic dimension but pelvic rotation cephalad tends to free the impacted anterior shoulder.4 McRoberts also involves a labor nurse applying supra pubic pressure in an attempt to dislodge the impacted shoulder. It must be noted, fundal pressure is contraindicated in shoulder dystocia as fundal pressure may further worsen the impaction of the shoulder and also may result in uterine rupture.5 The McRoberts maneuver resolves 50% to 60% of shoulder dystocias. If McRoberts maneuver is unsuccessful, multiple other obstetrical maneuvers are then recommended: Woods’ corkscrew maneuver, delivery of the posterior shoulder and Rubin maneuvers. There has been no consensus as to whether these maneuvers should be performed in any order. If these are not successful, deliberate fracture of the clavicle, and in a worst case scenario, Zavanelli maneuver in which the fetal head is pushed back into the pelvis and a cesarean section can be performed. CAN SHOULDER DYSTOCIA BE PREDICTED? According to ACOG, shoulder dystocia is most often unpredictable and unpreventable.6 Specifically, the ACOG Practice Bulletin states in its summary of recommendations: “Shoulder 4 Cunningham, et al., Williams Obstetrics, 22nd Edition, 2005, p. 515. ACOG Practice Bulletin, Clinical Management Guidelines for Obstetricians-Gynecologists, Number 40, November 2002. 6 ACOG Practice Bulletin, Clinical Management Guidelines for Obstetricians-Gynecologists, Number 40, November 2002. 5 4 dystocia cannot be predicted or prevented because accurate methods for identifying which fetuses will experience this complication do not exist.”7 According to Williams Obstetrics: “Although there are clearly several risk factors associated with shoulder dystocia, identification of individual instances before the fact has proven to be impossible.”8 Fetal macrosomia and maternal diabetes increase the risk of shoulder dystocia. Maternal obesity is associated with macrosomia and thus increases the risk for shoulder dystocia. Other antepartum conditions associated with shoulder dystocia include multiparity, postterm gestation, previous history of macrosomic birth, and a previous history of shoulder dystocia. Intrapartum risk factors include labor induction, epidural anesthesia, and operative vaginal delivery.9 PLAINTIFFS’ THEORIES IN SHOULDER DYSTOCIA CASES RESULTING IN BRACHIAL PLEXUS INJURIES AND POTENTIAL DEFENSES In the majority of lawsuits involving shoulder dystocia and a brachial plexus injury, plaintiffs’ attorneys make two basic claims: (1) that there were considerable risk factors suggesting shoulder dystocia was likely to occur and therefore a planned cesarean section should have been recommended or at least offered by the obstetrician and (2) the obstetrician applied excessive force when attempting to deliver the baby after shoulder dystocia was evident resulting in the stretching or avulsion of the nerves in the brachial plexus causing paralysis of the baby’s arm. Of course, the more antepartum risk factors present will make the case more difficult to defend. However, as stated above, the accepted medical literature is very strong in stating shoulder dystocia cannot be predicted or prevented. ACOG’s Level C recommendation on informed consent states: 7 Id. Cunningham, et al., Williams Obstetrics, 22nd Edition, 2005, p. 514. 9 ACOG Practice Bulletin, Clinical Management Guidelines for Obstetricians-Gynecologists, Number 40, November 2002. 8 5 In patients with a history of shoulder dystocia, estimated fetal weight, gestational age, maternal glucose intolerance, and the severity of the prior neonatal injury should be evaluated and the risks and benefits of a cesarean delivery discussed with the patient.10 Defending the allegation that the obstetrician should have been able to predict shoulder dystocia is the easiest to defend based upon the medical literature. Retaining good obstetrical expert witnesses to explain to the jury what the literature states and why predicting a shoulder dystocia is nearly impossible is essential in defending these cases. Most good plaintiffs’ lawyers will not file a shoulder dystocia/brachial plexus injury case unless there was permanent damage. It is worth the expense of hiring two obstetrician experts to testify regarding standard of care. Having a nationally-known expert who has written extensively on the subject along with a local expert is typically a good combination to present an effective case. The informed consent-type claim wherein plaintiff’s counsel alleges enough risk factors were present to require the obstetrician to give the mother informed consent and the option of having a cesarean section is somewhat more difficult to defend. Of course, with any case, the facts drive the defense. For instance, if the patient had a history of shoulder dystocia along with an estimated fetal weight higher than the prior pregnancy, a higher gestational age and diabetes, a defendant will be hard-pressed to argue he or she had no duty to at least discuss the risk and benefits of a planned cesarean delivery versus an attempted vaginal delivery. However, if the only risk factor is a history of shoulder dystocia and no other risk factors, the defense is much easier. According to ACOG, a history of shoulder dystocia is associated with a recurrence rate 10 ACOG Practice Bulletin, Clinical Management Guidelines for Obstetricians-Gynecologists, Number 40, November 2002. 6 ranging from 1% to 16.7%.11 Additionally, fewer than 10% of cases involving shoulder dystocia result in a persistent brachial plexus injury. Given the low percentage of brachial plexus with permanent injury, even a patient with a history of shoulder dystocia has an extremely low percentage of again having a shoulder dystocia resulting in a brachial plexus injury. ACOG does recommend consideration of a planned cesarean delivery to prevent shoulder dystocia for suspected fetal macrosomia with estimated fetal weights exceeding 5,000 grams in women without diabetes and 4,500 grams in women with diabetes.12 In defending a case where estimated fetal weight exceeds these parameters, the defense can argue ultrasound is not an accurate predictor of macrosomia and most macrosomic infants do not experience shoulder dystocia. Again, the facts will drive the defense. CLAIM OF EXCESSIVE TRACTION CAUSING BRACHIAL PLEXUS INJURY At trial, plaintiff’s counsel will play a day in the life video showing the injured child attempting various tasks without the use of his arm. Plaintiff’s counsel most likely will bring the child into court to demonstrate in front of the jury activities the child cannot perform without the use of both his arms. Plaintiff’s counsel will make the argument that the child has no or limited use of his arm because of the excessive traction used by the obstetrician in delivering the child following a shoulder dystocia. Plaintiff’s counsel will call expert witnesses to testify brachial plexus injuries that follow shoulder dystocia are caused by excessive traction used by the obstetrician in attempting to deliver the baby. 11 ACOG Practice Bulletin, Clinical Management Guidelines for Obstetricians-Gynecologists, Number 40, November 2002. 12 Id. 7 Many children who have suffered brachial plexus injuries are treated at Texas Children’s Hospital in Houston, Texas. The pediatric neurosurgeons or plastic surgeons who treat and perform surgery on the injured child will provide favorable causation testimony to the plaintiff. The group of physicians at Texas Children’s Hospital have written papers on management of obstetrical brachial plexus injuries. One paper states: “In a review of our center’s experience and of the literature available, we believe that traction is the predominant force creating these devastating injuries. The pathogenesis of the injury … is excessive lateral traction on the head of the infant away from the shoulder during labor.”13 Going further, the paper is critical of obstetrical literature that suggests an alternative cause of obstetrical brachial plexus injuries other than excessive traction following the shoulder dystocia. Such obstetrical literature points to brachial plexus injuries as being associated with high intrauterine forces, not traction injuries. Some obstetrical literature studies have shown brachial plexus injuries where delivery was made by cesarean section. The physicians at Texas Children’s Hospital in their paper are critical of the obstetrical literature. Specifically, their article states: “Although the above-mentioned studies from the obstetrical literature may help to explain certain cases in which brachial plexus lesions occurred in the absence of lateral neck traction, we believe that in the great majority of lesions, lateral traction during birth is the culprit.”14 DEFENDING THE CLAIM OF EXCESSIVE TRACTION DEPENDS UPON THE FACTS OF THE CASE If the charting was poor and no documentation was made of the use of any of the recommended maneuvers used to relieve shoulder dystocia, the defense will be extremely difficult. With little or sparse documentation of what happened at the time of delivery, plaintiff’s counsel can make Shenaq S., “Current Management of Obstetrical Brachial Plexus Injuries at Texas Children’s Hospital Brachial Plexus Center and Baylor College of Medicine. Seminars in Plastic Surgery,” Volume 19, Number 1. 2005: 46 14 Id. 13 8 the easy argument that the obstetrician pulled too hard on the baby’s head in attempting the delivery, causing a brachial plexus injury. In defending these claims, one should expect the mother or family members inside the delivery room to testify delivery room nurses were pushing on the uppermost portion of the mother’s belly or fundus. Fundal pressure is contraindicated when shoulder dystocia is discovered. Hopefully, the nurses and obstetrician will document supra pubic pressure was ordered and applied. Assuming the delivery is well-documented, a good way to defend these cases is to show a very orderly progression of actions once the shoulder dystocia was documented. Hopefully, the documentation will show the maneuvers employed by the obstetrician necessary to free the impacted shoulder and deliver the baby. The obstetrician will testify he or she used the necessary amount of traction to deliver the baby but not excessive force. The obstetrician should testify he or she used the same amount of force or pressure as used in all deliveries. The infant must be delivered as expeditiously as possible. The jury must understand the obstetrician goes through his or her progression of maneuvers in attempting to deliver the baby, but the baby must be delivered in a timely fashion or potentially suffer catastrophic brain injury or death. These cases are defended by showing the obstetrician performed the maneuvers required to deliver the baby in an orderly and timely fashion. However, it is important to show to the jury obstetrical literature providing evidence that permanent brachial plexus injuries occur where no shoulder dystocia is involved and in situations where delivery was accomplished by cesarean section. There is logic in plaintiff’s argument that brachial plexus injuries following shoulder dystocia result from traction on the fetal head that is applied in the opposite direction of the impacted shoulder. Given that the shoulder does not move and force is applied to the fetal head in the 9 opposite direction of the impacted shoulder, it makes anatomical sense that injury to the brachial plexus could result as the nerve roots are stretched or avulsed. The standard of care in a delivery complicated with shoulder dystocia is to follow the recommended maneuvers to effectuate the delivery. Compliance with the standard of care does not equate to a delivery without injury. Brachial plexus injuries, even permanent ones, can occur even when the obstetrician handles the complicated delivery within the standard of care. CONCLUSION These cases can be difficult to defend in that the jury will tend to be sympathetic to a young child who has little to no use of an arm. As to causation, it makes logical sense that a brachial plexus injury occurs because the shoulder is stuck and does not move and traction or pressure is placed on the head in the opposite direction in an attempt to deliver the baby resulting in stretching or tearing of the nerve or nerve roots. Nevertheless, these cases can be successfully defended if the medical record sets out an orderly rendition of what happened in the delivery room and the obstetrician performed the maneuvers required to effectuate delivery. 1968964 10