ROCR Application
advertisement
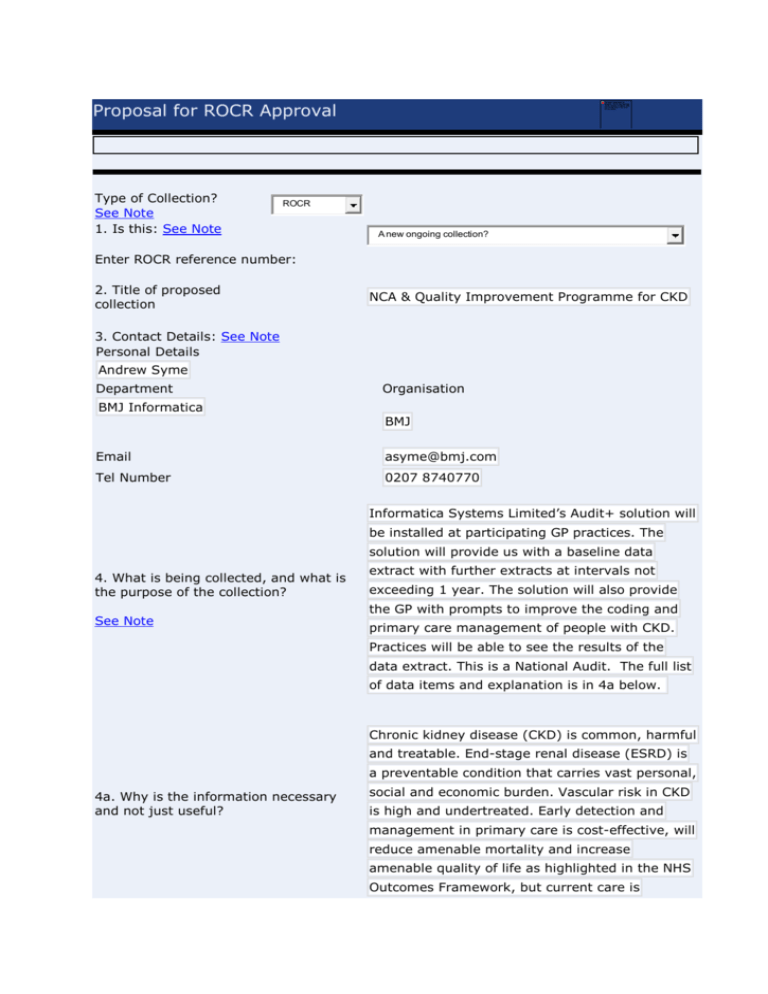
Proposal for ROCR Approval Type of Collection? See Note 1. Is this: See Note ROCR A new ongoing collection? Enter ROCR reference number: 2. Title of proposed collection NCA & Quality Improvement Programme for CKD 3. Contact Details: See Note Personal Details Andrew Syme Department Organisation BMJ Informatica BMJ Email asyme@bmj.com Tel Number 0207 8740770 Informatica Systems Limited’s Audit+ solution will be installed at participating GP practices. The solution will provide us with a baseline data 4. What is being collected, and what is the purpose of the collection? See Note extract with further extracts at intervals not exceeding 1 year. The solution will also provide the GP with prompts to improve the coding and primary care management of people with CKD. Practices will be able to see the results of the data extract. This is a National Audit. The full list of data items and explanation is in 4a below. Chronic kidney disease (CKD) is common, harmful and treatable. End-stage renal disease (ESRD) is a preventable condition that carries vast personal, 4a. Why is the information necessary and not just useful? social and economic burden. Vascular risk in CKD is high and undertreated. Early detection and management in primary care is cost-effective, will reduce amenable mortality and increase amenable quality of life as highlighted in the NHS Outcomes Framework, but current care is variable. Informatica Systems Limited have been selected by HQIP to deliver a national primary care CKD Audit covering all GP Practices in England & Wales and the interfaces between Primary and specialist secondary care Nephrology departments in those jurisdictions. This project is funded and approved by NHS England through the HQIP partnership as part of the NCAPOP. The overarching aims of this Programme are to: 1. Enable the improvement of the accuracy and timeliness in identifying CKD, within NICE national guidance and quality standards. 2. Enable the improvement of outcomes for patients through the provision of high quality comparative data. 3. Directly enhance the capacity of primary care providers to improve the quality of CKD care they deliver. DATA ITEMS PRACTICE AND PATIENT INFORMATION • GP practice. This is required to provide practice specific feedback in the audit • NHS number. This is required for HES linkage, and flagging with ONS • Date of birth. This is required to calculate age at events at baseline and during follow-up • Gender. Kidney function is estimated on a gender- and age-specific basis using serum creatinine values. This is an audit of kidney disease in primary care • Ethnicity. CKD shows ethnic variation, and the estimation of kidney function requires adaptation to the estimation formula according to ethnicity. • Date of extraction. Required to calculate age of patient at the time of data-extraction • Postcode. Required to calculate IMD and to link to HES and ONS data RISK FACTORS FOR CKD (all with dates, using read-codes) • Hypertension • Diabetes • Gout • Ischemic heart disease, congestive cardiac failure, atrial fibrillation • Cerebrovascular disease • Peripheral arterial disease • Kidney stones • Prostatic hypertrophy • Prescription of lithium last 1 year • Prescription of tacrolimus or cyclosporin last 1 year • Systemic lupus erythematosis and connective tissue disorders All these fields are needed to define who should be regularly undergoing kidney function test for an early diagnosis of CKD. • Estimated GFR/corresponding serum creatinine value in the last 12 months, and the first estimated GFR/corresponding serum creatinine value more than 3 months prior to that. If there is no estimated GFR/ corresponding serum creatinine value in the last 12 months, then the most recent estimated GFR/corresponding serum creatinine value within the last 24 months. Because the recommended formula to estimate GFR is likely to change in the next year, we need raw creatinine values as well. • Most recent proteinuria/urine dipstick codes • Most recent haematuria code • Most recent albumincreatinine ratio measurements All the above are required to define kidney function/damage. • CKD stages read codes and dates • Renal disease codes based on kidney diagnosis read code list All these codes are required to define a cohort of people with kidney disease in primary care and to determine the stage of their kidney disease. These codes will also help to identify patients who have not been correctly coded. They will also enable an assessment of how frequently patients are being monitored and if the correct monitoring is being carried out. • HES outpatient data on who was seen in specialist urology, diabetes, and nephrology clinic • Read code and date for the most recent referral or attendance at nephrology or diabetic outpatients. These are required to identify the patients not under on-going outpatient nephrology follow-up, and patients with indications for referral who were discussed with a specialist within 3 months of identification of the indication. Read codes for the most recent occurrence within the last 12 months, (with date): • Haemoglobin, calcium, phosphate, Vit D and PTH measurements/results • Vitamin D preparations • Alphacalcidol • Ergocalciferol • Cholecalciferol • Calcium tablets + variants • Sevalamer • Lanthanum • Aluminium hydroxide • Calcium acetate • ‘Dulwich mixture’/magnesium+calcium These are needed to determine the patients who have had a haemoglobin checked within the last year and the patients who have had a calcium, phosphate and PTH checked within the last year. Read codes for the most recent occurrence (with date): • Aspirin prescription • Contraindication to aspirin prescription • Statin prescription • Contraindication to statin prescription • Declines statin prescription • Declines aspirin prescription • Exercise advice/weight loss advice • Stop smoking advice • CV risk assessment (e.g Q risk, Framingham) • Declines CV risk assessment These are needed to determine the patients with CKD assessed for cardiovascular risk. Read codes for the most recent occurrence within the last 12 months, (with date): • Systolic BP • Diastolic BP • Antihypertensive medication classes: Angiotensin Converting Enzyme Receptor Blocker - - Angiotensin - Alpha Blocker - Beta Blocker - Calcium Channel Blocker - Diuretic - Aldosterone antagonists - Other Antihypertensive - Contraindication to ACE/ARB These are needed to determine the patients with CKD who have blood pressures in the NICE recommended target range, with use of drugs targeting the renin-angiotensin system in appropriate patients. Read codes for the most recent occurrence within the last 12 months, (with date): • influenza immunization • pneumococcal immunisation • hepatitis B immunisation • Hepatitis B test results These are needed to check that patients with CKD are being protected by vaccination appropriately. OUTCOME DATA Audit data using the cohort of people with kidney disease will be linked to the hospital episode statistics (HES and PEDW) and the office for national statistics (ONS) using ICD-10-codes: 1. Distribution and number of hospitalisation events via A&E in patients with CKD by CKD-stage within a 6-month period (HES/PEDW) 2. Patients with CKD who had either one, or two or more non-elective ICU admissions within a 6-month period (HES/PEDW) 3. CKD patients who had either one, or two or more hospitalisations with acute kidney injury/kidney failure within a 6-month period (HES/PEDW) 4. CKD patients with cardiovascular events (stroke, myocardial infarctions) within a 6-month period (HES/PEDW) 5. CKD patients who die within a 6month period (ONS) In subsequent years the burden for practices that have previously installed the software will be nil as the audit is automated without further practice input. There will remain a one-off install burden per practice of circa 30 minutes for the 4000 to 6000 practices expected to participate. 5. What has changed since this collection was last approved, and what is the overall effect of the changes? 6. What is the latest date for approval? See Note 7. Which organisation will be collecting this information? 01/01/2014 NHS England 1st Keyword: 8. List top three Keywords 2nd Keyword: 3rd Keyword: 9. What is the start date for this proposed collection? See Note 9a. Please state when you would like the ROCR licence to run from. 10. What is the finish date for this proposed collection? Please also include the date if the collection is ongoing. See Note 01/03/2014 01/03/2014 01/12/2016 CKD Kidney Renal The National CKD Audit is part of the National Clinical Audit and Patient Outcomes Programme (NCAPOP). NCAPOP is a closely linked set of 11. What Operating Framework commitment does the proposal support? centrally-funded national clinical audit projects See Note that collect data on compliance with evidence based standards, and provide local trusts with benchmarked reports on the compliance and performance. They also measure and report patient outcomes. 12. Who supports this proposal? See Note Minister: Earl Howe Group Director: Prof Bruce Keogh Policy Lead/Section Head support from: Simon Bennett Senior Civil Servant, to whom correspondence about the collection can be addressed: (give name, organisation, section, telephone and email address) Name Organisation Simon Bennett NHS England Section Telephone Quality Framework Team, Clinical Directorates 07768 486422 simonbennett1@nhs.net Email Has evidence of Gateway Support: (eg date, person, Gateway number if applicable) No Proposal for ROCR Approval ROCR Contact Details 13. Burden calculation? See Note Frequency Annual See Note Organisational Type GP Practice Number of organisations 400 Occupational Group See Note Days Hours Minutes Burden Days Burden Years Annual Burden £ Senior Managers 0 0 0 0 0 0 Managers 0 0 0 0 0 0 Clerical & Administrative 0 0 30 26.67 0.13 6070.4 Maintenance & Works 0 0 0 0 0 0 Healthcare Assistants and other support staff 0 0 0 0 0 0 Healthcare scientists 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 5 4.44 0.02 6068.31 All Nurses, Midwives and health visiting staff Scientific, therapeutic & technical staff (ST&T) (Inc. AHP's) Consultants GPs Hospital Doctors 0 0 0 0 0 0 CEO 0 0 0 0 0 0 Directors 0 0 0 0 0 0 Total 0 0 35 31.11 0.16 12138.71 Insert another Organisation type Grand Total Days 31.11 Grand Total Years Grand Total Burden 0.16 12138.71 1. The software install is a one off activity of circa 30 mins. 2. The annual audit collection is automated without practice input. 3. Please state if this is an increase or decrease in burden. See Note Data quality is already a required part of the patient management and the focussed QI tool will help GPs to manage data quality for CKD patients. Are you planning on collecting from Independent and Voluntary Sector Organisations? No Proposal for ROCR Approval ROCR Contact Details 14. If sampling of organisations is not being used please state why. See Note 15. Are the estimates above and the design of the collection supported by any pilots, consultation exercises, trials or other tests of the proposal? If so, please give details. See Note HQIP requirement is a national audit of all CKD patients. Therefore sampling is not appropriate in this case. 1. The collection is fully automated without GP or Practice involvement. This is achieved using the BMJ Informatica iCAP product (installed base more than 2000 GP practices) which is a proven technology. 2. The quality improvement tool, builds on the Audit+ product, and provides assistance to GPs in undertaking an activity which is already part of patient management. The efficacy of the QI tool will be subject to pilot testing and the tool will be subject to continuous improvement based on user feedback. 16. If your proposal results in an Not required as this is a new collection. See question 2 increase to the ongoing burden (as indicated in Q13 above), please indicate what measures you propose to reduce the burden elsewhere to result in a net zero change or decrease. See Note 17. What collection method do you Web based collection propose to use? Email See Note Extract from existing NHS systems Other electronic (e.g. spreadsheet or disk) Unify2 Input to Database Database extract Telephone Paper Omnibus collection See Note Other (give details) 17a. If other, please state: 18. For Non Foundation Trusts is the collection statutory, mandatory, part mandatory, voluntary or not required? See Note VOLUNTARY 18a. For Foundation Trusts is the collection statutory, mandatory, part mandatory, voluntary or not required? See Note NOT REQUIRED 19. Which of the following equalities dimensions are included in the collection? See Note Age/Date of Birth Gender Ethnicity (NHS standard 16 + 1) Sexual Orientation Faith Disability 20. Of those you propose to include in Q19, please give details of the definitions you intend to use for each? Collecting from GP Systems so definitions will be set by the systems producing the data which will in turn be driven by the MIM Specification. 21. Is this request accompanied by a No position statement from the NHS Data Model & Dictionary Service and the Information Standards Board for Health and Social Care (ISB HaSC)? If required, please contact Data Standards - datastandards@nhs.net, or ISB information.standards@nhs.net See Note 22. Is the information to be collected intended for publication or other release? If not, please give reasons why. See Note 23. If the answer to Q22 was yes, please state your publication or release strategy. See Note Yes. 1. Practice level data will be provided to CCGs & GPs through the National CKD Audit website. A Public & Patient version of the report will be provided to HQIP & published on the National CKD Audit Website. 2. Subject to suitable anonymisation, and agreement from HQIP, raw data will be made available through National CKD Audit Website and data.gov.uk in line with the Transparency & Open Data Agenda. 24. Will the data collection generate The RCGP has identified CKD as a clinical priority, any media interest, and if so, what therefore some media interest is expected. BMJ measures do you have in place to deal Informatica have a communications and media team, with it? and will work with HQIP to respond to any media enquiries. 25. Does the proposal have any impact on Social Services? See Note 25a. If the answer to Q25 was yes, please give reason. 26. Do you intend to collect information from NHS Foundation Trusts? See Note No No Please attach documents that support your ROCR application. Without a list of the questions to be asked we will not be able to process your application Insert item Proposal for ROCR Approval ROCR Contact Det 27. If the answer to question 26 is yes, state why? 28. Is the information or any part of it already collected? If so please state why this should be collected again. 29. Please explain why you propose the frequency of collection as stated in Question 13. 30. If you are proposing to collect from all Foundation Trusts, please give reasons why a sample cannot be used? 31. Can the proposed information be provided by commissioners rather than directly from Foundation Trusts? If not, why not? 32. Does all the data requested fall into one or more of these categories? See Note a. Vital for Patient Care b. Essential for the flow of funds to NHSFTs c. The requesting body has a statutory duty to provide the information d. Very High ministerial profile See Note e. Necessary for Care Quality Commission assessment f. Directly underpins delivery of a target (State which).





![Risk Adjustment Factor [RAF]](http://s2.studylib.net/store/data/005748329_1-97f04b2983127ae4930cafa389444167-300x300.png)
