Miscarriage. Preterm labor. Multifetal pregnancy
advertisement

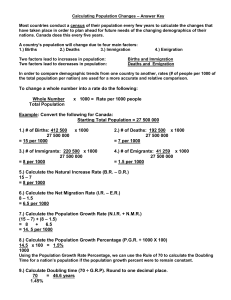
1 BUKOVINIAN STATE MEDICAL UNIVERSITY “Approved” on methodological meeting of Department of Obstetrics and Gynecology with course of Infant and Adolescent Gynecology “___”______________________ 201_ year protocol # T.a.the Head of the department Professor ________________ O.A. Andriyets METHODOLOGICAL INSTRUCTION for practical lesson “Miscarriage. Preterm labor. Multifetal pregnancy” MODULE 4: Obstetrics and gynecology CONTEXT MODULE 9: Pathology of pregnancy, labor and puerperium Subject: Obstetrics and Gynecology 6th year of studying 2nd medical faculty Number of academic hours – 6 Methodological instruction developed by: ass.prof. Andriy Berbets 2 Chernivtsi – 2010 3 1. Actuality of topic The problem of the involuntary premature breaking of pregnancy has not only medical but also social value, as closely associated with the question of fruitlessness, death of fetus, birth of sick children which give high morbidity and considerable level of child's death rate. 1. 2. 3. 4. 5. 6. 2. Duration of class: 6 hours 3. Educational purpose Student must know: Classification of involuntary abortions for the term of pregnancy and clinical form. Classification of premature births. Reasons involuntary premature breaking of pregnancy and premature births. Diagnostics of abortions in the early and late terms of pregnancy and premature births. Treatment of early and late involuntary abortion. Features of conduct of premature births. Student must be able: 1. To set reasons the involuntary premature breaking of pregnancy. 2. To diagnose premature births. 3. In good time to conduct prophylactic and medical measures at involuntary abortions premature births. 4. To make the plan of conduct of premature births. 5. To define beginning of the first period of births, objectively to estimate the dynamics of childbirth (degree of opening of neck of uterus, duration of labor). 6. To estimate partograph. 7. To determine and estimate palpitation of the fetus. 8. To determine beginning of the second period of births, objectively to estimate the dynamics of advancement of head of the fetus to the birth ways. 9. To give help in births and to conduct the anaesthetizing of births. 10. To demonstrate active tactic of conduct of the III period of births (on a phantom). 11. To demonstrate expecting tactic of conduct of the III period of births (on a phantom). 12. To determine general bleeding in births. 13. To estimate the state of new-born after a scale Аpgar. 14. To draw conclusions (resume) of births. 15. To estimate maturity of the fetus. Student must be able to perform the following practical skills: 1. To diagnose reasons of abortion of pregnancy, premature births. 2. To be able to distinguish the periods of breaking of pregnancy, premature births. 3. To be able to diagnose the clinical forms of the involuntary breaking of pregnancy and premature births. 4. To estimate the state of neck of uterus. 5. To be able to apply medical measures at all clinical forms of the involuntary breaking of pregnancy and premature births. 6. To estimate the results of amnioscopy, amniocentesis, interpretation of KTG, US. 7. Conduct of premature births. 8. Conduct and record of partograme. 4 4. Base knowledges abilities of skill, that themes necessary for the study (intersubject integration) Name of previous disciplines Got skills Anatomy To describe the anatomic structure of woman pelvis, uterus and additions Physiology To describe physiology processes in a womanish organism during births, to give clinical interpretation to reasons of beginning of births. Pharmacology To define preparation and to expect a dose for treatment of breaking pregnancy and anaesthetizing of births. 5. Information for the student 5.1. Table of contents of theme I. DETERMINATION OF CONCEPT, CLASSIFICATION AND FREQUENCY OF MISCARRIAGE Miscarriage is the spontaneous termination of pregnancy in a term since fertilization earlier then 37 weeks. Miscarriage in a term from conception to 22 weeks is named involuntary abortion. CLASSIFICATION OF SPONTANEOUS ABORTIONS It is conducted on the basis of different criteria: 1. Term of pregnancy at involuntary abortion: • early (to 12 weeks) • late (from 12 to 20 weeks) 2. Clinical form of abortion: • threatening • ongoing abortion • incomplete • complete • missed abortion • infected abortion Miscarriage in a term 22-37 weeks name premature births (pre-term delivery). CLASSIFICATION OF PREMATURE BIRTHS 1. Premature births in 22-27 weeks (mass of fetus 500-1000gram, unfavorable prognosis for fetus). 2. Premature births in 28-33 weeks (mass of fetus 1000-1800 gram, doubtful prognosis for fetus). 3. Premature births in 34-37 weeks (mass of fetus 1900-2500gram, sufficiently favourable prognosis for fetus). II. REASONS OF MISCARRIAGE. Reasons are very varied. They can be divided on follow groups: А. Social reasons • unsettled state of domestic life • extremely high or low age of mother • low social status • insufficient feed • professional to harmfulness 5 • action of unfavorable terms of external environment • harmful habits B. Medical reasons. 1. From the side of fetus: • genes and chromosomal anomalies ІІ. From the side of maternal organism: 1. Genetic factors. 2. Features of obstetric-gynaecological anamnesis of mother. 3. Somatic status of woman. 4. Anatomic factors: • hysteromyoma • anomalies of structure of uterus • cervix insufficiency 5. Endocrine disorders: • insufficiency of second phase of menstrual cycle • hyperandrogenia • disorder of fat metabolism • diabetes • dysfunction of thyroid gland 6. Factors of inflammatory genesis: • chronic infections (genital, respiratory system) • infections carried during pregnancy (acute infections of bacterial and viral genesis of any localization) 7. Complication of this pregnancy: • gestosis • twins • anomalies of location of placenta • anaemias of pregnant 8. Immunological disorders, which are characterized by making the organism of mother of the antibodies directed against its own structure: • AFS ( antefosfolipide syndrome) • conflict by system of АВО or factor of rhesus III. SOME KEY POINTS OF ETIOLOGY AND PATHOGENESIS OF MISCARRIAGE CHROMOSOMAL VIOLATIONS Possibility to use them for the study of genesis of the involuntary breaking of pregnancy appeared in connection with development of methods of genetic researches. On the early stages of development of pregnancy of involuntary abortion it is possible to examine as adaptation mined-out in the process of evolution, as a result birth of children with abnormal development is relatively the rare phenomenon. It is considered during many years, that about 50% cases of the involuntary breaking of pregnancy in early terms conditioned by chromosomal anomalies. With age a selection weakens, that is why at extremely high age of parents more frequent there are the anomalies of fetation. HORMONAL DYSFUNCTIONS In etiology of the involuntary breaking of pregnancy in a 1 trimester hormonal violations in the organism of mother. From them hypofunction of ovaries and hyperandrodeny different genesis is most frequently. Mechanism of breaking of pregnancy at inferiority 2 phases of menstrual cycle related not only to insufficiency of progesteron which is synthesized in a yellow body, as progesteron is 6 synthesized in chorion, and in future – in a placenta. Large value in genesis of early abortion is had by insufficient secretory transformation of endometrium Insufficiency of lutes phase can be conditioned: to the declines of honadotropin-relisin hormone, FSH and LH, that results in violation of steroidogenesis in ovaries, and also damage of receptors of еndometrium. Insufficiency of lutes phase at women with unmaturing of pregnancy can be conditioned by not only an inferior steroidogenesis but also frequent abortions, chronic endometritis, defects of development of uterus, infantilism, endometrial synechias. Early abortion can be predefined by the change of normal correlations of gonadotropic hormones in a 1 phase of menstrual cycle. Among endocrine reasons of unmaturing of pregnancy a considerable place occupies hyperandrogenia (21-48%). Reason of unmaturing more frequent is the effaced forms of hyrerandrogenia, which or appear during pregnancy or they can be diagnosed out of pregnancy by the functional tests of loadings. Hyperandrogenia of any genesis pregnancy is often complicated by the stop of developmment and death of fruit. Hyperandrogenia can be over renal (30%), ovaries (12%) and mixed (58%) genesis. One of endocrine factors of unmaturing can be the parafunction thyroid, both increase and decline. Violation of tolerance to glucose (saccharine diabetes) is the most widespread disease of the endocrine system. Depending on weight of diabetes and adequacy of correction of level of glucose of blood, pregnancy can make off the involuntary breaking in any terms, and also death of fetus. Diabetes is accompanied by violation of many aspects of metabolism, and these violations go beyond the scopes of violation only exchange of glucose ANATOMIC REASONS Insufficiency the neck of uterus is principal (to 40%) reason of abortion. Among women which suffer by unmaturing, the defects of development of uterus meet in 10-15% cases. In most women with violation of genesial function of defect of development of uterus unite with hypofunction of ovaries. Hysteromyoma is widespread of high quality tumour to the myometrium, that meets in an obstetric clinic at the patients of senior genesial age. FEATURES OF SOMATIC STATUS OF WOMAN The group of high risk on unmaturing of pregnancy is made by women with the diseases of the vascular system and another chronic diseases of organism. COMPLICATION OF THIS PREGNANCY Among factors which are instrumental in unmaturing of pregnancy, the complications related to pregnancy take considerable seat: a gestosis, anomalies of attachment, is placentas, premature removing a layer by the layer of the normally or low located placenta. IMMUNOLOGICAL ASPECTS OF UNMATURING OF PREGNANCY Pregnancy from immunological positions is an allotransplant, that has on to a 50% stranger maternal organism antigens of paternal origin. INFECTIOUS DISEASES OF MOTHER Among reasons of unmaturing one of the first places is occupied by the infectious diseases of mother. At sharp viral infections in mothers in majority there are spontaneous abortions, stillborn, births of children with anomalies of development. A certain role in unmaturing of pregnancy is had by an infection, that flows latently, chronic infectious diseases (tonsillitis, pyelonephritis and other) and also urogenital infection. FACTORS OF EXTERNAL ENVIRONMENT Risk of ABORTION rises at smoking abuse by an alcohol. The role of caffeine in genesis of abortion remains doubtful. 7 IV. CLINICS AND DIAGNOSTICS OF EARLY AND LATE ABORTION Clinical diagnostics of early and late abortion basis on the following signs: • confirmation of fact of presence of pregnancy (delay of menstruation, doubtful and reliable signs of pregnancy) • appearance of pain symptom, symptom of pathological (bloody) excretions from sexual ways and change from the side of body and neck of uterus Depending on expressed of clinical symptoms distinguish the following stages of the breaking of pregnancy: • threatening abortion • ongoing abortion • incomplete abortion • complete abortion At threatening feeling of weight or insignificant pains is marked in lower departments and in the region of sacrum. Bloody excretions from sexual ways, as a rule, are absent. An uterus is megascopic according to the term of delay of menstruation, changes from the side of vaginal part the necks of uterus are absent. Abortion in the motion is characterized by appearance of spasm pains in the lower departments of stomach, strengthening of degree of expressed of symptom of bloody excretions. The uterus answers on the sizes of term of delay of pregnancy, vaginal part of neck of uterus is shortened, softened, the channel of neck of uterus is exposed (a fruit egg can be in a cervical channel, in this connection the lower pole of him can be accessible for feeling). Abortion in motion can be completed by incomplete abortion, when a fruit egg is partly outcast from the cavity of uterus. Placenta stay too long in an uterus. By an important moment for diagnostics of incomplete abortion there are the anamnestic pointing in the presence of previous (see more high) stages of the wilful breaking of pregnancy. Clinical picture of incomplete abortion is characterized by the presence of insignificant pain that heaves up, in the lower departments of stomach and insignificant moderate bloody excretions, from sexual ways. The body of uterus is not answer the term of delay of menstruation of term of pregnancy (less). Patients with complete of abortion, for medical help, as a rule, does not apply. A diagnosis is foreseen retrospectively throuw on information of anamnesis. At pregnancy, that does not develop, after death of fruit egg retractive activity of uterus is absent, lost fruit egg it is not outcast from an uterus, but is added to the second changes. V. TACTIC OF SUBSEQUENT DIAGNOSTIC AND MEDICAL MEASURES included • information of obstetric-gynaecological anamnesis of woman • fact and term of pregnancy • stages of involuntary abortion VI. USE OF BRIDLES IN EARLY TERMS AT USUAL UNMATURING OF PREGNANCY It is thus expedient to draw on трансвагінальне ultrasonic research, that allows to conduct the detailed analysis of anatomic structure of embryo and structures of fruit egg, necessary for the estimation of character of motion of pregnancy and drafting of prognosis. VII. TREATMENT OF EARLY AND LATE INVOLUNTARY ABORTION The first trimester is a most difficult period and in a great deal determines development of pregnancy. Most researchers consider that ABORTION in a 1 trimester in 90% cases is the display of natural selection, and in therapy of early ABORTION include spasmolysants, vitamin therapy, sedative therapy. TREATMENT OF PREGNANT WITH INSUFFICIENCY of the neck of uterus. Nosotropic treatment is surgical correction. There are different methods and modifications directed on narrowing of internal pharynx by imposition of circular stitch. However, in spite of their 8 variety, a question about the surgical correction not is fully decided. For the surgical correction different modifications of method of Shirodcar , method of Macdonald and other. ТOCOLITIC THERAPY FOR TREATMENT OF LATE WILFUL ABORTION Apply tocolitic (partusisten, bricanil, hinipral) therapy for the correction tone and retractive activity of myometrium. Depending on the degree of expressed of clinical displays of the wilful breaking of pregnancy, possibly both parenterally and peroral introduction of tocolitic. How complex therapy of threatening late it follows to remember ABORTION possibility of parenterally application of sulfate of magnesium (МgSO4), aspirin, indomethacin. PREMATURE LABOR Premature births are births with the spontaneous beginning progress of childbirth and birth by fetus weight more 500 gr in the term of pregnancy from 22 to 37 weeks. In connection with the features of obstetric tactic and nursing of children which borned at the different terms of гестації expediently to select such periods: - 22-27 weeks; - 28-33 weeks; - 34-37 weeks pregnancy. On the modern stage of organization of obstetric help in Ukraine the leadthrough of premature births is optimum in the specialized obstetric permanent establishments in which terms are for the leadthrough of intensive therapy and reanimation of new-born. Expediently providing of rights for woman giving birth in bringing in of near to the presence on births. Principles of conduct of premature births: 1. Estimation of degree of the forecast risk of development of maternal and fetus pathologies with the purpose of determination of level of grant of stationary help. 2. Determination of plan of conduct of births and informed concordance of him with a woman. 3. Control after the state of mother and fetus in births with the conduct of partograma. 4. Prophylaxis of respirator distress -syndrome to 34 weeks pregnancies. 5. Anaesthetizing of births after testimonies. 6. Estimation of the state of child, support of thermal chainlet, leadthrough of primary rest room of new-born, common stay of mother and child from the first hours after birth at nursing of children with small weight. Diagnostics and confirmation of births: Confirmation of births: at pregnant after 22 weeks spasm pains appear at the bottom of stomach and sacrum with appearance of mucous bloody or watery (in the case of effluence of waters round a fetus) excretions from a vagina: - presence 1 fights during 10 minutes, that proceeds 15-20 seconds; the change of form and location of neck of uterus is progressive shortening of neck of uterus and its smoothing. Opening of neck of uterus is the increase of diameter of road clearance of neck of uterus, is measured in centimetres; - gradual lowering of head of fetus to the small pelvis in relation to the plane of entrance in a small pelvis (from data of external obstetric research) Executions sequence at the conduct of premature births 1. During hospitalization of pregnant (woman giving birth) in obstetric permanent establishment in the receiving-surveying separation (a doctor is the gynaecologist of accoucheur): 9 - carefully meets with the exchange card of woman in relation to motion of this pregnancy and supervision of her in womanish consultation. Attention applies on information of general, infectious and obstetric-gynaecological anamnesis, clinical-laboratory indexes of ambulatory inspection of expectant mother; - for the estimation of the state of woman giving birth the inspection is carried out: general review, measuring of temperature of body, pulse, arteriotony, breathing, inspection of internalss after organs and systems; - measuring of height of standing of bottom of uterus, circumference of stomach and sizes of pelvis is carried out. A term concernes pregnancies and date of births, expected mass of fetus: - it asks about feeling of motions of fetus by woman, that gives birth and auscultation and palpitation of fetus is conducted; - external and internal obstetric research is conducted : position, position and type of position of fetus, character of sexual activity, opening of neck, concernes uteruses and period of births, finding of head of fetus in relation to the planes of small pelvis; - from data of anamnesis, exchange card and results of physical and obstetric inspection woman giving birth writes down in history of births risk factors and degree of the forecast fetus and obstetric risk after a scale Copland, sparing attention, above all things, to the factors of risk, the term of pregnancy, obstetric diagnosis, is set, tactic of conduct of pregnant concernes (woman giving birth); - to 34 weeks pregnancies at opening of neck of uterus less than 3 sm, tocolis or treatment of threat of premature births is conducted to absence of аmnionitis, preeclampsia, bleeding, absence of suffering of fetus (to conduct not tocolis more than 24-48 hours). In 2 hours after the beginning of tocolis to confirm the diagnosis of premature births by establishment of smoothing, whether opening of neck of uterus. If premature births make progress - токоліз is abolished. Farther births are conducted on partograma. The prophylaxis of respirator distress syndrome of fetus is conducted: - at the threat of premature births by i/m introduction of dexametason for 6 mg every 12 hours on a course 24 mg, whether betametasone for 12 mg every 24 hours, on a course 24 mg; - in the case of beginning of premature births of introduction of dexametason of i/m for 6 mg every 6 hours (on a course 24 mg), betametasone for 12 mg in 12 hours (on a course 24 mg) (the repeated courses of this prophylaxis are not conducted); - diprospan for 1,7 ml i/m in 24 hours. Observation and medical aid at labor With the purpose of dynamic and evident supervision after motion of births, state of mother and fetus, and also with the purpose of timely prophylaxis of possible complications the record of partograma is used in births . Supervision on the state woman giving includes conservative procedures which are brought by the gynaecologist of accoucheur to partogroma: 1) The state of fetus is estimated: - the heart-throbs of fetus are counted up for 1 minute of each 15 minutes during an active phase and every 5 minutes during the second period of births, these indexes are brought to partpgrama. - if frequency of heart-throbs of fetus less than 110 or more than 170 shots for a minute, it is considered as beginning of development of distress fetus. 2) The common state of mother is estimated: - it is taken temperature body - every 4 hours; the parameters of pulse concerne - every 2 hours; arteriotony - every 2 hours; urine - the amount of - every concernes 4 hours; - the level of albumen and acetone concernes after testimonies; - breathing character concernes periodically. 10 3) Efficiency of childbirth it concernes: - by frequency, duration and intensity of spasm - hourly in a latent phase and every 30 minutes in an active phase; at normal duration of premature births there is a tendency to the increase of speed of opening of neck of uterus which in a latent phase is 0,8 sm/hour; in active - 3.5 sm/hour . - the dynamics of internal obstetric research is every 4 hours; - by the level of lowering of head of fetus - during the leadthrough of every external and internal obstetric research . 4) If the break of fruit bubble took place, attention applies on the color of amnion waters: - the presence of thick meconium testifies to the necessity of careful supervision and possible interference for the grant of help in the case of distress fetus; - absence of effluence of liquid after the break of fruit bubble specifies on diminishing of volume of fetus liquid, that can be related to distress fetus. Anaesthetizing of births on the concordance of woman If woman, that gives birth suffers from pain during labor: - it is psychologically supported and is calmed down; - it is suggested to change position of body; it is encouraged to active motions; it is offered to the partner to massage her the back, to hold her arm and to wipe a person by a sponge between the fights; it is offered to the woman to adhere to the special technique of breathing (deep inhalation and slow exhalation) - in most cases it diminishes feeling of pain; Requirements which behave to the medicinal anaesthetizing: anaesthetic an effect, absence of negative influence on the organism of mother and fetus, simplicity and availability for all establishments. For anaesthetizing of births is used no inhalations (systems) and inhalations анестетики, regional anaesthesia. Systems analgetic is used also to that end (at opening of neck of uterus no more than 5-6 sm). Narcotic analgetic not used. Grant of hand help in the II period of births A right for a woman to choose position which is comfortable is provided in the II period of births, both for her and for a medical personnel. A medical personnel adopts births in a clean dressing-gown, mask, glasses and sterile gloves. In the second period of births the supervision is conducted after the common state of woman giving birth, haemodynamic indexes (arteriotony, a pulse is every 10 minutes) state of fetus, is control of cardiac activity of fetus every 5 minutes, by advancement of head of fetus on a maternity channel. Conduct of the III period of births With the purpose of bleeding prophylaxis during the first minute after birth of fetus intramuscular 10 is entered oxitocin. It is conducted controlled advancement for an umbilical cord only on condition of presence of signs of separation of placenta from an uterus. Thus one hand carries out the careful controlled sipping for an umbilical cord, and the second hand that is directly above pubis, there is an uterus and is some taken from a bosom, that west-to-east relatively controlled advancement. In default of signs of removing a layer by the layer of placenta and external bleeding during 30 minutes after birth of fetus the hand separation of placenta and selection of dung is conducted. The massage of bottom of uterus through the front abdominal wall of woman giving birth is carried out at once after birth of dung. After it it is offered to the woman to empty an urinary bladder. The cannulation of urinary bladder is carried out after testimonies. After birth of dung make sure in that placenta, the shells of fruit bubble are fully remote and an uterus grew short. 11 An early puerperium provides for: review of maternity ways in mirrors, renewal of integrity of crotch in the case of the conducted episiotomy or perineotomy continuous or separate stitches by filament, supervision after the common state of mother, retractive function of uterus and amount of bloody excretions, every 15 minutes during 2nd hours after births in a maternity hall and at next 2 o'clock in a post-natal chamber. Use of ice-bag on the bottom of stomach in an early puerperium is not used. Multiple pregnancy With thedecline in perinatal morbidity and mortality from other causes, multiple pregnancy now warrants special attention from obstetricians. First, they are common, having increased in incidence by 50% in developed countries over the last two decades. Second, they make a disproportionatecontribution to perinatal morbidity and mortality, well in excess of that due to multiplication of singleton risks by fetal number. Next, almost every maternal and obstetric problem occurs more frequently in multiples. Finally, there are a number of intrapartum considerations, including manipulations no longer practised in singletons. Whereas previously maternal management was stressed, the modern approach to managing multiple pregnancy focuses on recognizing fetal risk as stratified by chorionicity, monitoring fetal growth and wellbeing by ultrasound and reducing risks of preterm delivery. Recognizing the specialized nature of multiple pregnancy management, it has been recommended that, like for diabetes, multiple pregnancies be managed within any one hospital by a single consultant-led multidisciplinary team. Incidence The considerable geographical and temporal variation in twinning incidence reflects factors influencing dizygotic or non-identical twinning, which results from multiple ovulation. Twinning occurs in from 4/1000 births in Asia to 54/1000 in Africa, and is common in older mothers, presumably due to their rising follicle-stimulating hormone (FSH) levels. Familial predisposition to multiple ovulation can be demonstrated ultrasonically, although a gene has yet to be identified. In contrast, monozygous or identical twinning, which results from early cleavage division of a single blastocyst, occurs with a constant incidence of 3.9/1000. Perinatal wastage Perinatal mortality in twins is nearly four times higher and in triplets six times higher than in singletons. Cerebral palsy is nearly three times more common in twins, and more than 10 times as common in triplets as in singletons. These figures are per baby, whereas themore relevant figurein counselling parents is thechanceof their multiple pregnancy producing any one baby with these complications. Thus a twin pregnancy has eight times and a triplet pregnancy nearly 50 times the chance of a singleton of producing a baby with cerebral palsy. This high perinatal wastage is largely attributable to the increased chance overall of prematurity and intrauterine growth restriction and of complications specific to monochorionic twins. Chorionicity and zygosity Two thirds of twins aredizygous (DZ) and one third MZ. However, chorionicity, not zygosity, mediates the degree of perinatal risk in any individual multiple pregnancy. Ultrasonic determination of chorionicity Chorionicity can be determined on ultrasound with 100% accuracy in the first trimester, by counting the constituent layers of the dividing membranes. Demonstration by colour Doppler of a functional artery-to-artery anastomosis is more challenging but provides definitive proof of monochorionicity. Chorionicity should be determined on ultrasound in all multiple pregnancies. This is because chorionicity is relevant to: (1) counselling parents about perinatal risks; (2) counselling parents about their risk of genetic and structural abnormality; (3) invasive testing and managementof discordant abnormality; (4) feasibility of multifetal pregnancy reduction; (5) risk of sequelae in the presence of fetal 12 compromise; (6) early detection and management of twin–twin transfusion syndrome. It should be done at the first ultrasound, as it is most accuratein thefirst trimester; fortunately all ART pregnancies have an early scan, as do the increasing number undergoing nuchal screening. Miscarriage Twins have a high incidence of spontaneous early pregnancy loss, one study suggesting 12% of human conceptions start off as twins. Studies of ultrasound or abortal pathology indicatethat twins arefound twiceas commonly in the first trimester as at birth. First trimester resorption of one previously ultrasonically viable twin knownas the ‘vanishing twin’phenomenonis estimated to occur in over 20% of twins. Spontaneous first trimester loss of one or more fetuses in high-order multiple pregnancies is common, with nearly 40% of pregnancies in which three sacs are seen in early pregnancy delivering twins. When one twin dies in utero in the mid-trimester, a fetus papyraceus, its squashed paper-like remains may be found among the placenta after delivery. Invasive procedures Invasive procedures in twins are complex and should only be performed in fetal medicine centres. Great care is taken to avoid mislabelling and misidentification of an affected twin. Whilethis may befacilitate d in thepr esenceof discordant gender or structural abnormality, it is good practicealways to map thetopography in terms of location within the uterus, placental site, cord insertion and plane of the dividing septum. This is a prerequisite for interpretation of discordant results and for selective feticide. Ideally the operator doing the diagnostic procedure should also undertake any selective feticide to minimize uncertainty and obviate any need for confirmatory invasivete sting. In structurally concordant MC twins, only one needs sampling for prenatal diagnosis, but the operator should be certain of this on first trimester scanning. With this exception, it is important to ensure that both fetuses are sampled separately. With amniocentesis this is best achieved by two separate ultrasound-guided procedures as farawayas possible from the dividing septum, although there are series using single-entry techniques with low rates of complications. With fetal blood sampling, the intrahepatic vein can be sampled to avoid confusing the cord origins. Most operators consider chronic villus sample (CVS) contraindicated in DC twins, because of a 1–5% rateof contamination, and thus potential for false positive and negative results through inadvertently sampling thesametwin twice. Otherwise DNA fingerprinting and/or confirmatory amniocentesis may be necessary in DC twins with concordant-sex karyotypes at CVS. Miscarriage rates after amniocentesis in twins seem higher than in singletons, although the lack of randomized trials or large cohorts preclude estimation of the procedure-related risk. Maternal responses All the normal physiological adaptations such as increased cardiac output, glomerular filtration rate and renal blood flow are increased in multiple pregnancy. Red cell mass increases approximately 300 ml more than in singletons, but because this is disproportionately less than the one third increase in plasma volume, haemoglobin values fall. Iron stores are diminished in 40% of women with twins, so that routine haematinic supplementation is recommended, particularly given the increased risk of post-partum haemorrhage and Caesarean section. Hyperemesis gravidarum is more likely and severe cases may respond to steroid therapy or odansetron. All the minor complications of pregnancy such as backache, oedema, varicose veins, reflux, haemorrhoids etc. are also increased, both as a result of the physical effects of greater uterine size and also of greater placental hormone production. Gestational diabetes is increased in most studies. Pre-eclampsia is two to three times more common in multiple than singleton pregnancies and likely to be more severe. There is no good evidence that it is increased in MC compared to DC pregnancies. Unlike other high-risk groups, uterine artery Doppler screening has low sensitivity. Management is based on standard principles, save that the risks of iatrogenic prematurity with delivery apply to two fetuses. After delivery, the difficulties coping with the demand of two or more babies are considerable, with 13 depression, stress and relationship difficulties more common in mothers of multiples than singletons. Given the high perinatal wastage in multiple pregnancy, there is often the added burden in the post-natal period of coping with bereavement. Antenatal classes dedicated to multiples have a role in preparing parents not just for differences in antenatal care and delivery, but also for the extra demands of breast feeding and coping. Intrauterine growth restriction Ultrasound is the primary tool for monitoring growth in multiple pregnancies for two reasons. First, they are at high risk of intrauterine growth restriction (IUGR), with 25% of twins being small for gestational age at birth. In most cases IUGR will be discordant affecting one twin only. Second, abdominal palpation and symphysis– fundal height measurement are unreliable as indices of individual fetal growth as, instead, they reflect total intrauterine growth. There is no agreement on the ideal frequency of ultrasound examinations in twins, but a conservative policy for detecting IUGR in DC twins is four weekly scanning from 24 weeks, with further scans and/or Doppler measurements as indicated. MC twins should be scanned at fortnightly intervals from 16 weeks, both to allow early diagnosis and thus treatment of twin–twin transfusion syndrome, and to pre-empt intrauterine death from IUGR through timely delivery (or pre-emptive cord occlusion prior to viability) to protect the healthy co-twin. There is controversy as to whether singleton or twin biometric charts should be used. Preterm labor This is themajor causeof neonatal death in multiplepr egnancy. The median gestational ages at delivery in twins and triplets of 37 and 34 weeks, respectively, are not so much a concern in terms of survival, as the proportion delivering less than<30 weeks (c. 7 and 15%, respectively). Although plurality substantially increases the chance of preterm delivery, once in the neonatal unit an individual baby’s prognosis is the same or better than gestational age- and weight-matched singletons. Parents should be informed of the symptoms and signs of threatened preterm labour and the advisability of early presentation. Management of preterm labour in multiple pregnancies differs little from that of singletons, other than the consequences of prematurity affecting a greater number of babies. The following discussion concentrates on those aspects, which pertain especially to multiple pregnancy. Prevention Preterm labour in multiple pregnancy, as with polyhydramnios, is attributed to uterine over-distension. Accordingly, there are no specific preventative measures aside from fetal reduction in high-order multiples. Although hospitalization for bed rest has been practised in the past, there is little evidence to support its use. Indeed, meta-analysis of six randomized controlled trials suggests that bed rest in twins increases the chance of preterm delivery.With the exception of progesterone, prophylactic tocolytics are of no benefit in singletons, and thus it is not surprising that randomized trials similarly report no clear benefit in twins. There was no reduction in preterm birth or related outcomes in the only trial of 17hydroxyprogesterone caproate in twins. Management: β2 mimetics are no longer used for tocolysis, given their cardiovascular side effects and in particular pulmonary oedema for which multiple pregnancy was a risk factor. Although atosiban and nifedipine seem equally effective in delaying preterm labour, there is increasing concern in twin pregnancies about the adverse cardiovascular effects of nifedipine. Nine of the 14 reported cases of pulmonary oedema associated with tocolytic calcium channel blockers were in twins; therefore nifedipine should not be used in multiple pregnancies. Glucocorticoids should be used in multiple pregnancies at risk of delivery < 34–36 weeks in the next 7–14 days. Consistent with this, retrospective studies suggest that multiple pregnancy attenuates the beneficial effect of antenatal steroids. The possibility that a larger dose is required remains to be tested. Repeated prophylactic steroids are 14 not recommended. First, retrospective data show that fortnightly steroids from 24 weeks did not reduce the incidence of respiratory problems in twins. Second, there is concern that these may impair fetal growth and/or brain development. Finally, they may prevent indicated courses working, as only the first course has been shown to be beneficial. Twin–twin transfusion syndrome Chronic TTTS occurs in 15% of MC twins and is responsible for 15–20% of perinatal death in twins. The pathophysiology involves chronic net shunting of blood from the donor to recipient twin. The donor becomes growth restricted, oliguric and develops anhydramnios (’stuck twin’) and the recipient becomes polyuric with polyhydramnios and can go on to develop cardiac sequelae and hydrops. TTTS usually presents in the mid- but sometimes the third trimester, with gross discordance in amniotic fluid volume, with polyhydramnios in the recipient’s and oligohydramnios in thedonor ’s sac. Theusual placental configuration comprises unbalanced deep artery to vein anastomoses with absent or inadequate compensation along superficial anastomoses. Thus Doppler detection of a compensatory artery-to-artery anastomosis antenatally substantially reduces the chance of developing TTTS, and where it does develop, predicts better prognosis. Untreated, perinatal loss rates in the mid-trimester exceed 80%, with survivors at risk both of neurological morbidity acquired in utero or at birth and of cerebral palsy. Perinatal mortality rates have fallen to around 50% over thelast decade due to a range of treatments comprising serial amnioreduction, septostomy, fetoscopic laser ablation of placental anastomoses and cord occlusion. Twin reversed arterial perfusion sequence This rare condition (1:35,000 pregnancies) arises in MC twins withtwocords linked by a large arterio-arterial anastomosis such thatflowfromone, the ‘pump twin,’ supplies the other, the ‘perfused’ twin, in a retrograde fashion. The term ’twin reversed arterial perfusion’ (TRAP) sequence is preferred to the older ‘acardiac monster’, so named as reversed deoxygenated arterial supply is associated with only rudimentary development of upper body structures such as thehe art, faceand arms. Perinatal mortality in thepump twin is up to 55%, dueto polyhydramnios and cardiac failure. Although polyhydramnios may be alleviated by amnioreduction or sulindac therapy, definitive treatment requires occlusion of the perfused twin’s cord, which can now be achieved by a variety of fetoscopic or ultrasound-guided techniques. Techniques such as radiofrequency ablation and interstitial laser which occlude intrafetal rather than cord vessels give the best results, with a pump twin survival rate of > 80%. Monoamniotic twins One percent of identical twins liein thesamesac, so that they almost all develop cord entanglement in the first trimester. Their high perinatal mortality rate of up to 30– 50% is attributed to cord accidents both at delivery and in the last half of pregnancy. Perinatal mortality has fallen in recent series to 10–25% due to elective preterm delivery, mandatory Caesarean section and intensive fetal monitoring. Prophylactic maternal sulindac therapy to reduce fetal urine output and thus amniotic fluid volume has been successfully used in over 20 cases in our centre to split the twins’ excessive movements through relativeoligohydramnios and thus reducetherisk of cord tautening. Monoamniotic placenta are characterized by a high frequency of large artery to artery anastomoses, which explains why they rarely get TTTS and also why single intrauterine death frequently progresses to double fetal death. Delivery Timing The antepartum stillbirth rate in twins exceeds that of singletons, both per fetus and, in particular, per pregnancy. Thus whileawaiting ther esults of a randomized trial in progress, it seems prudent to recommend elective delivery at 37–38 weeks when neonatal morbidity is lowest. Thelar gerisein stillbirths seen in population data at 38 weeks is artifactual, reflecting gestational age at delivery not at intrauterine death. There is an argument for delivering MC twins earlier, based on their high rate of unexplained death rate in utero and thede sireto avoid the consequences of fetal death to its co-twin. Twins are not a contraindication to induction. 15 Vaginal delivery Mode of delivery has traditionally been decided on the presentation of the first twin (cephalic in 70%, breech in 30%), and fetal growth and well-being. Caesarean section has been advised where the first twin is breech, based on extrapolation from the term breech trial, and the desire to avoid the rare interlocking with head entrapment of a presenting breech above a second cephalic twin. The presentation of the second twin is of little relevanceuntil after thebirth of thefirst. Parturients with a previous Caesarean section are probably best delivered by repeat Caesarean, because of greater risks of scar dehiscence/rupture due both to uterine distension and to intrauterinemanipulation of these cond twin. For vaginal delivery, continuous cardiotocography (CTG) of both twins is facilitated by use of a dual channel recorder and/or a combination of internal and external electrodes. Anintravenous line is sited, antacids given and blood drawn for cross matching, in view of the increased incidence of Caesarean section and post-partum haemorrhage. Augmentation may be used as in singletons. An epidural is strongly advised in case internal manipulation of the second twin is needed. Caesarean section There is an increasing trend to Caesarean. Essentially the risks of vaginal delivery are increased in twins compared to singletons, as are the risks of Caesarean section. A large international randomized trial is underway to resolvetheoptimal modeof delivery in twins. In the interim, it seems reasonable to offer women Caesarean section where otherwise suitable for vaginal delivery. This is based on (1) a high intrapartum section rate in twins, with evidence from other trials suggesting that maternal morbidity from elective section is comparable where the emergency rate exceeds one in three and (2) increasing recognition that the second twin has a chance of intrapartum-related death some five-fold higher than first twin or singletons. 5.2. Theoretical questions: 1. What is abortion and preterm labor? 2. What are the classification of abortion? 3. What causes abortion and labor? 4. What are the stages of spontaneous abortion? 5. What are clinical characteristics of abortion threat, inevitable abortion, incomplete abortion, complete abortion and preterm labor? 6. What is the different between incomplete abortion and complete abortion? 7. What is pregnancy that does not develop? 8. What is usual abortion? 9. What are signs pregnancy that does not develop? 10. What kind of examinations are performed to women with threatening abortion and preterm labor? 11. What methods of treatment for abortion and preterm labor do we use? 12. What methods of examinations and tests are preformed at inevitable abortion? 13. What tests do we use for pregnancy after complete abortion? 14. What are methods of treatment of inevitable abortion? 15. What instruments are used for curettage of uterine walls? 16. What drugs do we use for treatment of threatening abortion, inevitable abortion and preterm labor? 17. What are possible complications during and after operative treatment of inevitable abortion? 18. What are peculiarities of postoperative care? 19. What are operation techniques of curettage? 16 20.What objective signs of childbirth and its efficiency in the II period of births? 21.What features of conduct of the II period of births? 22.Than is the III period of births, his duration characterized? 23.Does active tactic of conduct of the III period of births consist in what? 24.Does expecting tactic of conduct of the III period of births consist in what? 5.3. Practical works (task) which are executed on employment: In the gynaecological separation: 1. To collect anamnesis, execute internal vaginal research and research by mirrors. 2. To estimate a clinical form and stages of involuntary abortion. 3. To estimate involuntary abortion after the term of pregnancy. 4. To diagrammatize medical measures depending on the stage of involuntary abortion. In the maternity separation: 1. To collect anamnesis, execute external research of woman giving birth, draw conclusion about the period of births, which she is in. 2. To define finding ahead, position, position, type of fetus, degree of insertion of head by external methods. 3. To estimate the state by the fetus method of auscultation. 4. To conduct the prophylaxis of respirator distress-syndrome of fetus. 5. To estimate the state of neck of uterus at worn and premature families. 6. To estimate the state of new-born after a scale Аpgar (in the case of demonstration of births). In an educational room: 1. To rotin on a phantom methods of estimation of degree of insertion of head by the method of internal obstetric research 2. To rotin on a phantom technique of obstetric help in the II period of births. 3. To demonstrate on a phantom active tactic of conduct of the III period of births. 4. To demonstrate on a phantom expecting tactic of conduct of the III period of births (signs of removing a layer by the layer of placenta, selection of the removed layer by a layer placenta). 5. 5.4. Materials for self-control А. Questions for self-control: 1. What possible reasons of involuntary abortions in the early and late terms of pregnancy and premature births? 2. What moments of biotmechanism of births do you know? 3. What medical tactic for the prophylaxis of respirator distress-syndrome? 4. What signs of beginning of premature births? 5. How many periods have births? 6. What features in every period of births? 7. What of you know the methods of anaesthetizing of births? Б. Tasks for self-control 1. In the obstetric separation the pregnant is delivered in a term 25-26 weeks. Complaints about rhythmic pain down stomach and in small of the back, which every 6-7 minutes are, lasts 3040 seconds. It is set at internal obstetric research, that the neck of uterus is smoothed out, opening 4 sm. What is called this condition? 17 A. Preterm labor B. Early abortion C. Late abortion D. Complete abortion E. Incomplete abortion В. Теsts . 1. Remote effects of artificial abortions are A. Uterine wall perforation B. Incomplete removal C. Traumas of the urinary bladder D. Traumas of the rectum E. Disorder of menstrual function 2. Abortion is made according to the desire of a women until A. 12 weeks B. 16 weeks C. 20 weeks D. 22 weeks E. 28 weeks 3. The sign of full remove of conceptus is A. Pain B. Bleeding C. No bleeding D. Smaller size of the uterus E. Opening of cervix 4. Interrupting of pregnancy in late term can be performed depending on indications to A. 22 weeks B. 24 weeks C. 26 weeks D. 28 weeks E. 32 weeks 5. After abortion the control A. Discharge from genitalia B. Pulse rate C. Arterial pressure D. Temperature E. All mentioned 6. Dilation of the cervical canal is done by A. Speculum B. Retractor C. Hegars dilators D. Forceps E. Curettes 7. We use for uterine sound A. Process of the uterine cervix B. Dilation of the cervical canal C. Examination of the cervical canal D. Examination of length and form of the uterine cavity E. Curettage 18 8. Interrupting of pregnancy in late term is done by A. Oxytocin B. Methylergometrin C. 5% Iodone solution D. Iodonate E. 20% Glucose solution Literature Basic 1. Бодяжина В.И., Жмакин К.Н., Кирющенков А.П. Obstetrics. IT IS, 1998. -С. 107-113. 2. Запорожан В.М. Obstetrics and gynaecology - 2000. - С. 172-177. 3. Айламазян Е.К. Obstetrics. С-Petersburg, 1998. - С. 113-116. Additional 1. Obstetrics and gynaecology / Степанковская Г.К., Л.В., Михайленко Е.Т. и др.; под ред. Г.К. Стспанковской. К.: 1997. - С. 187-190. 2. Дуда И.В., Дуда В.И. Obstetrics. - Минск -1997. - С. 80-92. Тимошенко 19 1. After the term of pregnancy involuntary abortions divide on: A. Early В. Late С. Second D. Primary Е. Correct answers A, В* 2. Early abortions arise up: А. To 8 weeks of pregnancy В. To 10 weeks of pregnancy С. To 12 weeks of pregnancy * D. To 14 weeks pregnancies Е. To 16 weeks of pregnancy 3. Late abortions arise up: А. From 8-10 weeks of pregnancy В. From 12-20 weeks of pregnancy* С. From 20-24 weeks of pregnancy D. From 25-28 weeks of pregnancy Е. From 28-30 weeks of pregnancy 4. Premature births are breaking of pregnancy in a term: A. 5-10 weeks pregnancies В. 12-14 weeks pregnancies С. 14-18 weeks pregnancies D. 18-22 weeks of pregnancy Е. 22-37 weeks of pregnancy* 5. All belongs to the clinical forms of involuntary abortion, except for: А. Threat abortion В. Abortion, that began С. Abortion in motion D. Complete, incomplete Е. Premature families * 6. To reasons, unmaturing of pregnancy take: А. Socially demographic В. Medical (from the side of embryo, mother) С. Endocrine, immunological violations D. Factors of inflammatory genesis Е. All transferred*