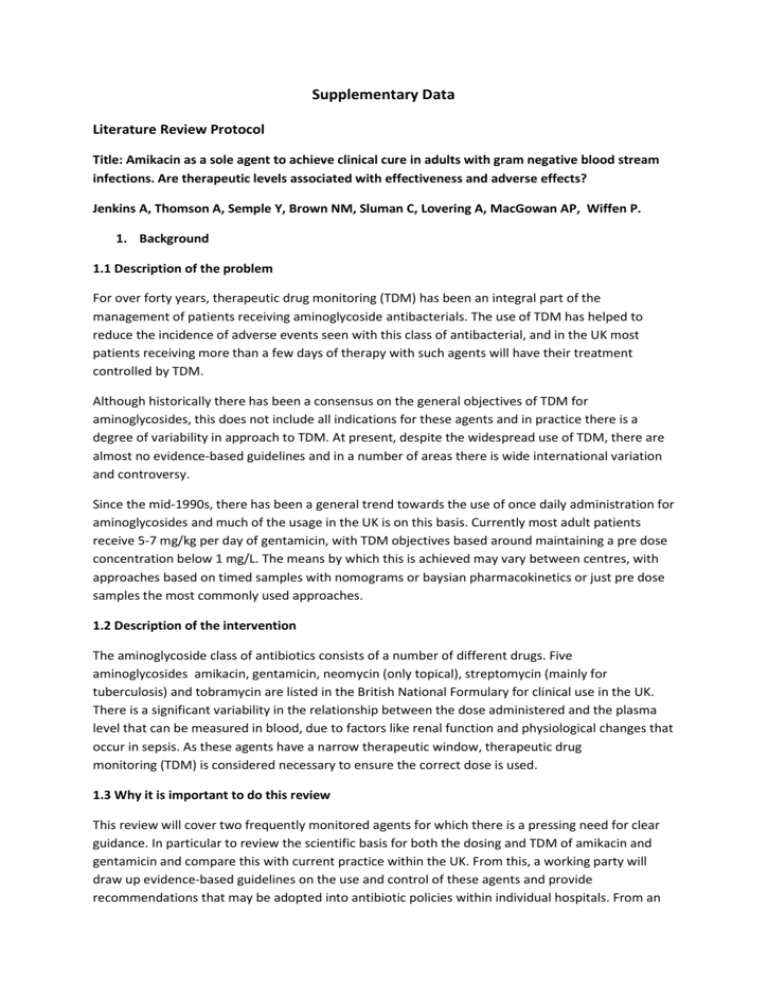
Supplementary Data
advertisement
Supplementary Data
Literature Review Protocol
Title: Amikacin as a sole agent to achieve clinical cure in adults with gram negative blood stream
infections. Are therapeutic levels associated with effectiveness and adverse effects?
Jenkins A, Thomson A, Semple Y, Brown NM, Sluman C, Lovering A, MacGowan AP, Wiffen P.
1. Background
1.1 Description of the problem
For over forty years, therapeutic drug monitoring (TDM) has been an integral part of the
management of patients receiving aminoglycoside antibacterials. The use of TDM has helped to
reduce the incidence of adverse events seen with this class of antibacterial, and in the UK most
patients receiving more than a few days of therapy with such agents will have their treatment
controlled by TDM.
Although historically there has been a consensus on the general objectives of TDM for
aminoglycosides, this does not include all indications for these agents and in practice there is a
degree of variability in approach to TDM. At present, despite the widespread use of TDM, there are
almost no evidence-based guidelines and in a number of areas there is wide international variation
and controversy.
Since the mid-1990s, there has been a general trend towards the use of once daily administration for
aminoglycosides and much of the usage in the UK is on this basis. Currently most adult patients
receive 5-7 mg/kg per day of gentamicin, with TDM objectives based around maintaining a pre dose
concentration below 1 mg/L. The means by which this is achieved may vary between centres, with
approaches based on timed samples with nomograms or baysian pharmacokinetics or just pre dose
samples the most commonly used approaches.
1.2 Description of the intervention
The aminoglycoside class of antibiotics consists of a number of different drugs. Five
aminoglycosides amikacin, gentamicin, neomycin (only topical), streptomycin (mainly for
tuberculosis) and tobramycin are listed in the British National Formulary for clinical use in the UK.
There is a significant variability in the relationship between the dose administered and the plasma
level that can be measured in blood, due to factors like renal function and physiological changes that
occur in sepsis. As these agents have a narrow therapeutic window, therapeutic drug
monitoring (TDM) is considered necessary to ensure the correct dose is used.
1.3 Why it is important to do this review
This review will cover two frequently monitored agents for which there is a pressing need for clear
guidance. In particular to review the scientific basis for both the dosing and TDM of amikacin and
gentamicin and compare this with current practice within the UK. From this, a working party will
draw up evidence-based guidelines on the use and control of these agents and provide
recommendations that may be adopted into antibiotic policies within individual hospitals. From an
extensive search there is only one systematic review of amikacin comparing once daily with multiple
dose administration. No systematic reviews of gentamicin were identified and yet there are several
recent national guidelines that include specific TDM regimens without any apparent high quality
evidence to support these recommendations.
2. Objectives
For the two aminoglycosides, to identify therapeutic regimes and drug concentrations that are
consistent with a good therapeutic outcome and to determine the drug exposures that are related
to the adverse events of nephrotoxicity and ototoxicity.
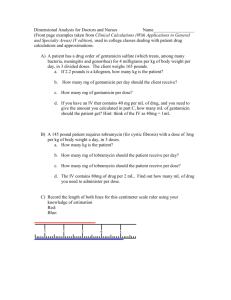
3. Methods
3.1 Criteria for considering studies for this review
3.1.1. Types of studies
Randomised control trials (RCT), controlled clinical trials (CCTs), interrupted time series with at least
three data points before and after implementation of the intervention (ITS), controlled before and
after studies (CBA). Full journal publication is also required.
3.1.2. Types of participants
Adults with proven gram-negative bacteraemia treated with one of two aminoglycosides (amikacin
or gentamicin), aged 18 and above. Participants who are over 75 years, or who have renal
impairment will be included but analysed as a sub group. Renal impairment will be defined as an
eGFR of <60ml/min.
The following participants will be excluded:), cystic fibrosis, pregnancy, burns or mycobacterial
infections.
3.1.3 Types of interventions
Therapeutic drug monitoring (TDM) and dose adjustment for aminoglycoside drugs- gentamicin and
amikacin as a single agents. (This will mean two reviews- one for each drug.)
Comparators- single or combination of agents or different durations of treatment. (Combination
therapy arms will not be analysed but may have useful data from a single agent arm comparator)
3.1.4 Types of outcome measures
3.1.4.1 Primary outcomes
Therapeutic cure defined as reduction of fever, improvement in clinical signs, or reduction in
inflammatory response.
Adverse events defined as toxicity seen as nephrotoxicity and ototoxicity. Nephrotoxicity to be
defined as mild, medium or severe using the RIFLE criteria
TDM results as blood levels reported for cure
TDM results for nephrotoxicity measured by serum creatinine and/or eGFR
Ototoxicity as a report
3.1.4.2 Secondary outcomes
Serious adverse events or death due to all causes
28 day mortality
Other adverse events as reported in the included studies
Length of hospital stay
Change in antimicrobial therapy to an alternative agent.
3.2 Search methods for identification of studies
3.2.1 Electronic searches
Searches will be conducted in Medline, Embase and the Cochrane Central Register of Controlled
Trials (CENTRAL), published in The Cochrane Library
The following search strategy will be used by searching in title, abstract and keywords
#1.
Aminoglycoside* (or: gentamicin, amikacin).
#2.
Pharmacokinetic*
#3.
Pharmacodynamic*
#4.
Efficacy
#5.
Resistance
#6.
Nephrotoxicity
#7.
Ototoxicity
#8.
TDM
#9.
(Therapeutic drug* monitoring
#10.
(antimicrobial assay*)
#11.
(#2 OR #3 OR #4 OR #5 OR #6 OR 7 OR #9 OR #10 )
#12.
(#1 AND #11)
3.2.2. Searching other resources
Reference lists of included studies will be scanned to seek to identify further studies not identified
by electronic searching.
3.3 Data collection and analysis
3.3.1 Selection of studies
Studies meeting the inclusion criteria will be identified by two authors (initials) independently and
any discrepancies resolved by discussion with other authors. Studies which are excluded after an
initial sorting will be recorded with a brief description of the reason for exclusion. Studies will be
restricted to English language only.
3.3.2 Data extraction and management
A data extraction form will be developed to facilitate the collection of data from each included
studies. Data extraction will include the following information:
Lead author and date of publication, dates that the study was conducted
Participant details including numbers, age, gender mix, condition
Setting and geographical location
The dose used, frequency of dose and length of treatment
Numbers of participants with therapeutic cure
Numbers of participants with adverse events
Methods for TDM, including assay and control approaches
Detection of significant under/over dosing with each aminoglycoside
Record of dose or exposure (AUC) and outcome
Record of dose or exposure (AUC) and toxicity
Dosing and TDM in therapeutic cure
Dosing and TDM in participants with adverse events of nephrotoxicity and ototoxicity
Dosing and TDM in renal impairment or altered pharmacokinetics
Time of TDM
Time of report of cure and toxicity
3.3.3. Assessment of risk of bias in included studies
Assessment of risk of bias in included studies
Two authors independently assessed risk of bias for each study and the Cochrane Risk of bias tool for
randomised controlled trials was adapted for this review.3
1. Random sequence generation (checking for possible selection bias). We assessed the
method used to generate the allocation sequence as: low risk of bias (any truly random
process, e.g. random number table; computer random number generator); unclear risk of
bias (method used to generate sequence not clearly stated). Studies using a non-random
process (e.g. odd or even date of birth; hospital or clinic record number) will be excluded.
2. Allocation concealment (checking for possible selection bias). The method used to conceal
allocation to interventions prior to assignment determines whether intervention allocation
could have been foreseen in advance of, or during recruitment, or changed after
assignment. We assessed the methods as: low risk of bias (e.g. telephone or central
randomisation; consecutively numbered sealed opaque envelopes); unclear risk of bias
(method not clearly stated). Studies that do not conceal allocation (e.g. open list) were
excluded.
3. Blinding of outcome assessment (checking for possible detection bias). We assessed the
methods used to blind study participants and outcome assessors from knowledge of which
intervention a participant received. We assessed the methods as: low risk of bias (study
states that it was blinded and describes the method used to achieve blinding, e.g. identical
tablets; matched in appearance and smell); unclear risk of bias (study states that it was
blinded but does not provide an adequate description of how it was achieved). Studies that
were not double-blind were excluded.
4. Incomplete outcome data (checking for possible attrition bias due to the amount, nature
and handling of incomplete outcome data). We assessed the methods used to deal with
incomplete data as: low risk (< 10% of participants did not complete the study and/or used
‘baseline observation carried forward’ analysis); unclear risk of bias (used 'last observation
carried forward' analysis); high risk of bias (used 'completer' analysis).
5. Size (checking for possible biases confounded by small size). Small studies have been shown
to overestimate treatment effects, probably because the conduct of small studies is more
likely to be less rigorous, allowing critical criteria to be compromised.20,21,22 Small studies
with limited data are subject to large chance effects.23 Studies were considered to be at low
risk of bias if they had 200 participants or more, at unclear risk if they had 50 to 200
participants, and at high risk if they had fewer than 50 participants.
6. Other bias. We identified studies that were sponsored by the Pharmaceutical industry. Any
other biases will be noted.
7. For ITS and CBA studies we will use the revised EPOC risk of bias tool.24 We will score each
study for risk of bias as 'Low' if all criteria were scored as 'Done', 'Medium' if one or two
criteria were scored as 'Unclear' or 'Not Done', and 'High' if more than two criteria were
scored as Unclear' or 'Not Done'.
3.4 Reporting of Results
Details of included studies will be recorded in a characteristics of included studies table based on the
data extracted. Those studies which were considered but excluded will be listed in an ‘excluded
studies’ table together with a brief explanation of the reason for exclusion.
3.5 Measurement of treatment effects
Where data permit, we will calculate numbers needed to treat to benefit (NNTB) as the reciprocal of
the absolute risk reduction (ARR). For unwanted effects, the NNT becomes the number needed to
treat to harm (NNH) and is calculated in the same manner. We will use dichotomous data to
calculate risk ratio (RR) with 95% confidence intervals (CI) using a fixed-effect model unless
significant statistical heterogeneity is found (see below).
If data permit, we plan to analyse according to therapeutic cure and separately for adverse events.
We will use a fixed-effect model for meta-analysis; a random-effects model will be used if there is
significant clinical heterogeneity and it is considered appropriate to combine studies. In addition we
will record therapeutic drug concentrations together with overall results for cure and adverse
effects. An intention to treat analysis will be conducted if data permit.
A summary of findings table for the main outcomes will be presented.
Where data are not available for analysis a description of the findings will be presented
3.6 Sub group analysis
Participants who are over 75 years, or who have renal impairment will be included but analysed as a
sub group.
3.7 Assessment of heterogeneity
We will deal with clinical heterogeneity by combining studies that examine similar conditions. We
will assess statistical heterogeneity visually and with the use of the I² statistic.25 When I² is greater
than 50%, we will consider possible reasons.
4. Acknowledgements
Vittoria Lutje was commissioned by BSAC to complete the searching for studies
5. Contributions of authors
All authors contributed to the design of the review
PW wrote the first draft of the protocol and all authors agreed the final draft
6. Declarations of interest
NMB has served on an advisory board for Discuva Ltd.
PW. Manages his own business, Oxford Systematic Review Services which received some payment
for involvement with this review.
7. Sources of support
This work has been supported by funds approved by the board of the British Society of Antimicrobial
Chemotherapy.
Final version September 2014
Characteristics of Included Studies
Barza 1980 13
Methods
Participants
Interventions
Outcomes
Notes
Prospective, randomised study
90 participants with serious Gram negative infections.
Ages of participants not documented.
Pre-treatment renal function of participants is not
documented and renal impairment is not an exclusion
factor.
Amikacin 5mg/kg every 8 hours or netilmicin 2.5mg/kg
every 8 hours, usually reduced to 2mg/kg every 8 hrs
within 2 days.
Actual body weight was used to calculate dose
Efficacy data not clear.
Nephrotoxicity (assessed in 32 amikacin and 37 netilmicin
pts). Increase creatinine due to amikacin (4),
nephrotoxicity due to netilmicin (3) - one of these
considered to be due to antibiotics.
Auditory toxicity (assessed in 15 amikacin and 19
netilmicin pts): amikacin (4) and netilmicin (3).
Vestibular toxicity: (3/16 and 0/15)
TDM levels: amikacin peak 15-25µg/ml, netilmicin peak 69µg/ml.
Timing of peak levels not given.
17/90 bacteraemia patients. Unable to separate these
patients.
Duration of therapy not documented.
Bock 1980 14
Methods
Participants
Interventions
Outcomes
Notes
Prospective randomised study
80 participants with serious Gram negative infections.
Mean ages were for amikacin 58.5years +/- 11.2 years and
for netilmicin 64years +/- 12.2 years.
Renal impairment was not an exclusion criteria.
Amikacin 7.5mg/kg bd or netilmicin 2-2.5mg/kg then
2mg/kg every 8 hours. Lean body weight was used for
dose calculations.
Clinical evaluation (35,36): cure (14,17), improve (12,13),
fail (7,4).
Nephrotoxicity (29,34): definite (1,6), possible (2,4),
doubtful (8,13).
Ototoxicity (23,29): definite (6,1), possible (0,1)
Np pts had vertigo or tinnitus.
TDM levels: amikacin trough ≤ 5µg/ml peak 15-25µg/ml.
Netilmicin trough ≤2µg/ml peak 4-8µg/ml.
Trough levels were taken 30 minutes pre-dose whilst peak
were taken one hour after the infusion.
Mean duration of therapy for amikacin 11.5days+\-
6.88days and for netilmicin 11.1 days +\- 12.2 days.
Chen 2005 19
Methods
Participants
Interventions
Outcomes
Notes
Prospective study
45 participants with cirrhosis followed by a spontaneous
bacterial peritonitis. Mean age for amikacin group 54
years +/- 17 years and for netilmicin 58 years +/- 11 years.
Patients with a serum creatinine greater than 2mg/dl
were excluded from the study.
Amikacin 500mg daily ( or 8mg/kg if body weight was less
than 60 kg) or cefotaxime 1g qds
Clinical outcomes (18,19): cure (15,11), infection relatedmortality (0,3).
Nephrotoxicity (18,19): renal impairment (2,2),
nephrotoxicity (1,1).
TDM levels: trough≤30µg/ml. Timing of samples taken for
trough levels is not documented.
No bacteraemia patients.
Antibiotics were administered for up to five days.
DeMaria 1989 17
Methods
Participants
Interventions
Outcomes
Notes
Randomised, prospective, non-blinded study
122 participants with sepsis or serious Gram negative
infection. Only 10 participants received amikacin.
Age for participants for the aminoglycoside group 59.5
years +/-19.1years and for aztreonam 56.8 years +/- 22.5
years.
Particpants with a serum creatinine greater than 2mg/dl
were excluded.
Participants on ITU received amikacin, those elsewhere
received tobramycin.
Amikacin 15mg/kg/day or tobramycin 4.5mg/kg/day or
aztreonam 1-2g every 8 hours. Dose were calculated using
actual body weight.
The mean duration of therapy was 7.7days for the
aminoglycosides and 9.4days for aztreonam.
Data for amikacin and tobramycin pooled- no evaluable
data.
TDM levels: amikacin trough 5-10µg/ml peak 20-30µg/ml,
tobramycin trough ≤2µg/ml peak 5-10µg/ml.
Samples were taken for trough levels at 30 minutes before
the next dose and peak levels were taken one hour postdose.
Amikacin not analysed separately- no evaluable data.
No bacteraemia patients.
Dillon 1989 4
Methods
Prospective, randomised, open study.
Participants
Interventions
Outcomes
Notes
Not clearly stated.
Mean ages of the PK and standard dose groups were
45.0years (range 18-81) and 49.6 years (range 23-80)
respectively.
Patients with a serum creatinine greater than 1.5mg/dl
were excluded.
Amikacin 7.5mg/kg of ideal body weight bd or amikacin
doses amended to retain levels within recommended
limits
Differences between groups for cure, duration of stay and
duration of therapy were not significant.
Nephrotoxicity: PK group (3), standard group (1).
TDM levels: trough 4-8mg/l peak 25-30mg/l.
Trough levels were taken immediately pre-dose. Peak
levels were extrapolated to given peak concentrations at
time zero.
Pts not retain within range in standard group were
crossed over to PK group.
11/82 had suspected or documented G-ve bacteraemia.
Mean duration therapy for PK dosing 8.9 days +/- 6.4 days
and for standard dosing 7.4 days +/- 4.3 days.
Galvez 2011 5
Methods
Participants
Interventions
Outcomes
Notes
Prospective study
120 participants with severe sepsis or septic shock.
Mean ages for the groups were 61.4 +/- 11 years, 60.7 +/13.4 years and 54.5 +/- 17.1 years.
Amikacin 15mg/kg/day or 25mg/kg/day or 30mg/kg/day.
Doses were based on actual body weight. If this was not
available ideal body weight was calculated.
Duration of therapy was 5 days for the 25 and
30mg/kg/days groups and 10 days for the 15mg/kg/day
group.
Amikacin 15, 25 or 30mg/kg/day. Cmax > 60µg/ml (0%,
39%, 76%). Day 28 CrCl 95.6+/- 47.4, 89.7+/-26.6, 56.4+/18.4ml/min.
TDM levels: amikacin peak levels were measured one
hour post dose.
Gatell 1983 18
Methods
Participants
Interventions
Prospective randomised study.
113 participants with suspected sepsis, urinary or biliary
tract infection or pneumonia.
Mean ages were for amikacin 58+/- 23.2 years and for
tobramycin 59+/- 20.4 years.
7.5mg/kg every 12-24 hours or tobramycin 1.7mg/kg
every 8,12 or 24 hours. Actual body weight was used for
dose calculations.
Outcomes
Notes
Nephrotoxicity in amikacin and tobramycin groups did not
differ by age, sex, initial creatinine levels, duration for
therapy, total dose, mean levels, concurrent drugs and
causative agents. Increase in Cr was similar between the
groups.
Nephrotoxicity (54,59): (13%, 6.8%). Patients with other
potential causes of acute renal failure were excluded from
nephrotoxicity calculations.
Ototoxicity (17,19): (2%,3%)
TDM levels: trough ≤10µg/ml peak 40µg/ml. Tobramycin
trough ≤2µg/ml peak 10µg/ml. Timings of the samples are
not documented.
Pts who developed auditory toxicity were significantly
older, with an abnormally high trough level. In logistic
regression only age was retained as a significant and
independent factor for toxicity.
Includes non-bacteraemic patients.
Duration of therapy for amikacin 9.5+/- 3.9 days and for
tobramycin 9.4+/-3.8 days.
Giamarellou 1991 2
Methods
Participants
Interventions
Outcomes
Notes
Gilbert 1977
Open randomised study
60 participants with urinary tract, respiratory tract, soft
tissue infections, prostatitis, cholangitis or abdominal
abscess.
Participants range from 23-81 years in the bd group and
20-76 in the od group.
Patients with renal insufficiency, serum creatinine greater
than 180µmol/l were excluded.
Amikacin 7.5mg/kg bd or 15mg/kg/day calculated using
actual body weight.
Clinical response: cure (76.7%, 97%), improved (6%, 3%),
failure (16.6%, 0%).
Nephrotoxicity: (2,2).
Ototoxicity (1,1)
TDM levels: trough ≤10µg/ml peak 40µg/ml. Troughs
were taken immediately pre-dose whilst peaks were taken
60 minutes after the start of infusion.
Discrepancy between groups with more pneumonias in bd
group which responded poorly to amikacin. od group
included lots of UTIs which responded very well.
No bacteraemic patients.
Mean duration of therapy was 10.4 and 9.6 days in the bd
and od groups.
9
Methods
Participants
Prospective randomised study.
30 participants with urinary tract infections with an age
Interventions
Outcomes
Notes
range of 16-86 years. Patients with 'impaired renal
function' were excluded from the study.
Amikacin 9mg/kg/day in 3 divided dose or gentamicin 34mg/kg/day in 3 divided doses using actual body weight.
Bacteriological response: cure (10,9), persistence (0,1),
superinfection (2,1), re-infection (2,2), relapse (1,2).
Nephrotoxicity: (2,2)
Auditory toxicity (0,0)
Vestibular toxicity (0,0)
TDM levels: amikacin no range. Gentamicin peak 48µg/ml. Peaks levels were measured one hour after the
start of a 30 minute infusion. No information documented
on the timing of trough levels.
No bacteraemic patients
Duration of treatment was 7-14 days.
Holm 1983 10
Methods
Participants
Interventions
Outcomes
Notes
Ibrahim 1990
Prospective randomised study
135 participants with septicaemia, urinary tract infection,
pneumonia or other infection. Participants had an mean
age of 64 years with a range of 17-94.
Patients with renal impairment (serum creatinine greater
than 400 µmol/l or creatinine clearance less than
10ml/min) were excluded.
Amikacin 7.5mg/kg bd or gentamicin 1mg/kg tds based on
actual body weight.
No difference in cure rates between amikacin and
gentamicin treated pts with verified infections.
Nephrotoxicity: (3/49,9/46)
Ototoxicity (3/38,5/31)
TDM levels: amikacin peak 35mg/l. Gentamicin 2mg/l. The
timing of sampling is not documented. Age range: 17-94.
Duration therapy is a short as possible- 'usually not more
than seven days'.
68/135 patients had septicaemia.
6
Methods
Participants
Interventions
Outcomes
Prospective randomised study in two parts. First part
looks at netilmicin (not relevant to this review). Second
part looks at amikacin.
40 participants with pelvic inflammatory disease received
amikacin. Age range 17-43 years. Exclusion criteria are not
documented.
Amikacin 14mg/kg/day (od or two divided doses) or
netilmicin 6.6mg/kg/day (od or two divided doses). Dises
were calculated using actual body weight.
Nephrotoxicity: no significant rise in serum creatinine was
Notes
observed in either group.
od groups experienced less phospholipidosis.
Auditory toxicity: low frequency(1,2,0,2), high frequency
(3,4,3,9)
TDM levels: no recommended range. No action taken in
response to levels. Samples were taken at 8 and 11.5
hours after the end of the infusion.
No bacteraemia patients.
Mean duration of therapy was 7 days for both groups.
Kiel 2008 7
Methods
Participants
Interventions
Outcomes
Notes
Prospective randomised study
40 participants with febrile neutropenia in haematology or
oncology patients. Mean age for extended interval is 51
years and for conventional dosing 54 years.
Patients with a creatinine clearance less than 30ml/min
were excluded.
Amikacin 15mg/kg/day in one or two divided doses.
Dosing was based on actual body weight unless pt was
greater than 120% of ideal body weight, in which case
adjusted body weight was used.
Nephrotoxicity: (1/20, 2/20)
TDM levels: no range. No timings of peak and trough were
specified.
No evaluable data. 11/20 of the 'od' group were changed
to conventional dosing due to the serum conc falling
below the pre-specified interval.
Duration of therapy 1.3days for extended and 5.5days for
conventional therapy groups.
Lerner 1986 11
Methods
Participants
Interventions
Outcomes
Notes
Prospective randomised study
106 participants with suspected or documented infection
that seemed likely to require an aminoglycoside. Mean
age for the amikacin group was 41+/-17 years and for
gentamicin 48+/-22 years. Patients with impaired renal
function were included.
Amikacin 6mg/kg every 8 hours or gentamicin 1.7mg/kg
every 8 hours.
Nephrotoxicity: 0/52, 8/54.
Ototoxicity: 7/52, 6/54.
Vestibular toxicity: 4/34, 3/33.
There was a modest association between nephrotoxicity
and elevated mean trough levels.
TDM levels: amikacin trough <10µg/ml peak 15-30µg/ml.
Gentamicin <2.5µg/ml peak 4-8µg/ml.
Trough levels were taken 30 minutes pre-dose. Peak levels
taken 15-30 minutes intravenous infusion and 60-75
minutes after intramuscular injection.
Mean duration of therapy was 11days for amikacin and 10
days for gentamicin.
Bacteraemia in 19/106 patients
Maigaard 1978
15
Methods
Participants
Interventions
Outcomes
Notes
Maller 1993
Prospective randomised study
57 participants with a complicated urinary tract infection.
Mean age of 69 years (range 27-87). Patitents with renal
impairment were not excluded.
Amikacin 7.5mg/kg bd im or netilmicin 2mg/kg bd im.
Doses based on actual body weight.
Therapeutic results: cure (16,20), persistence/relapse
(3,5), reinfection/superinfection (9,4).
CrCl: pre-treatment: ({81.5+/-6.7}, {74.6+/-4.8}), posttreatment: ({78.6+/-5.1}, {76.2+/-4.3}).
TDM levels: no recommended range but levels reported.
Troughs were measured at 12 hours whilst peaks levels
were measured at one hour,
Duration of therapy was 7-10 days.
No bacteraemia patients
8
Methods
Participants
Interventions
Outcomes
Notes
Open comparative study randomised by centre.
316 participants with suspected or verified Gram negative
infection with a mean age of 62 years.
Amikacin 11mg/kg/day (od or bd) or 15mg/kg/day (od or
bd) or 7.5mg/kg bd according to renal function. Actual
body weight was used to calculate the dose.
Patients with a creatinine clearance less than 25ml/min
were excluded.
Satisfactory clinical response: od- 92/101, bd 89/99.
Nephrotoxicity: 7/111, 8/102 more common in men
Auditory toxicity: 1/54, 0/51
vestibular toxicity: 1/23, 1/23
TDM levels: 12 hour trough <10mg/l, 24 hour group
trough <5mg/l. Tmining of peak levels is not documented.
Mean duration of therapy for once daily groups is 5.4+/2.2days and 5.9+/-3.7 days for bd groups.
Noone 1989 16
Methods
Participants
Prospective randomised study
202 participants with known or suspected Gram negative
sepsis. Age range for amikacin patients was 19-97 years
and for netilmicin 22-90 years. Patients with renal
impairment were included however those on dialysis were
not included in nephrotoxicity analysis.
Interventions
Outcomes
Notes
Amikacin 7.5mg/kg bd or netilmicin 3.5mg/kg every 12
hours. Doses based on actual body weight.
Outcome: success (74/82, 68/86), failure (8/82, 18/86).
Beneficial effect with amikacin is probably due to
beneficial activity against Ps. aeruginosa
Nephrotoxicity: 4/96, 11/91. More netilmicin patients had
pre-existing renal conditions. (23/96 and 35/91)
Auditory toxicity: 7/53, 8/51.
TDM levels: trough ≤10µg/ml peak 20-30µg/ml. Netilmicin
trough ≤4µg/ml peak 10-15µg/ml. Peak samples were
taken one hour after intramuscular injection or 20
minutes after intravenous infusion.
Mean duration of therapy was 10.4 days for amikacin and
8.5 days for netilmicin.
Smith 1977 12
Methods
Participants
Interventions
Outcomes
Notes
Footnotes
od- once daily
bd- twice daily
tds- three times a day
qds- four times a day
pts- participants
Prospective randomised double blind study
71 participants with the possible or documented Gram
negative infection. Mean age for amikacin patients was 63
years (range 29-91) and for gentamicin the mean was 56
years (range 20-92). Patients with renal impairment were
not excluded from the study.
Amikacin 8mg/kg or gentamicin 2mg/kg. Levels taken and
following doses calculated by nomogram. Doses were
calculated using actual body weight
Efficacy: favourable response (30/39, 25/32). Nonsignificant difference.
Nephrotoxicity: (5/62,7/62). An additional 4 pts in each
group developed possible toxicity.
Auditory toxicity: (2/34, 3/30).
TDM levels:amikacin peak 20-40µg/ml. Gentamicin peak
5-10µ/ml. Peak levels were obtained one hour post-dose.
Mean duration of therapy of amikacin was 8.7 days (range
4-20) and for gentamicin, 8.9 days (range 4-23).
Characteristics of Excluded Studies
Bartal 2003 26
Beaucaire 1995 27
Buring 1988 28
Contrepois 1985 29
Cox 2011 30
Damas 2006 31
De Broe 1984 32
De Broe 1991 33
de Champs 1994 34
Dupont 2000 35
Feld 1977 36
Finley 1982 37
Francetic 2008 38
Garraffo 1990 39
Karachalios 1998 40
Kern 1999 41
Klastersky 1986 42
Lerner 1977 43
Marik 1991 44
Neville 1995 45
Oliveira 2009 46
Piccart 1984 47
Raad 2003 48
Reed 1992 49
Santré 1995 50
Van der Auwera 1991 51
Vanhaeverbeek 1993 52
Wiland 2003
53
Cannot separate amikacin from gentamicin
Not randomised
Review paper
Healthy volunteers
Not RCT
Not amikacin alone
Prophylaxis
Prophylaxis
Paediatrics
Combination therapy
No TDM
Combination therapy
Not RCT
Not RCT
Amikacin levels measured but not acted upon.
Combination therapy
Combination therapy
Children included in study population
Population from 1 year, no separate data for adults
Not amikacin
Not RCT
Combination therapy
Not amikacin
Not RCT
Not RCT
Not RCT
Amikacin levels measures and reported as an average but not acted
upon.
Not RCT
Excluded studies
26
27
28
29
Bartal C, Danon A, Schlaeffer F, Reisenberg K, Alkan M, Smoliakov R, et al. Pharmacokinetic
dosing of aminoglycosides: a controlled trial. American Journal of Medicine 2003;194-8.
Beaucaire G. Evaluation of the efficacy and safety of isepamicin compared with amikacin in
the treatment of nosocomial pneumonia and septicaemia. J Chemother 1995;7 Suppl 2:16573.
Buring J E, Evans D A, Mayrent S L, Rosner B, Colton T, Hennekens C H. Randomized trials of
aminoglycoside antibiotics: quantitative overview. Rev Infect Dis 1988;10:951-7.
Contrepois A, Brion N, Garaud J J. Renal disposition of gentamicin, dibekacin, tobramycin,
netilmicin, and amikacin in humans. Antimicrobial Agents and Chemotherapy 1985;520-4.
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
Cox Z L, Nelsen C L, Waitman L R, McCoy J A, Peterson J F. Effects of clinical decision support
on initial dosing and monitoring of tobramycin and amikacin. American journal of Health
System Pharmacy 2011;624-32.
Damas P, Garweg C, Monchi M, Nys M, Canivet J L, Ledoux D, et al. Combination therapy
versus monotherapy: a randomised pilot study on the evolution of inflammatory parameters
after ventilator associated pneumonia. Critical Care 2006;R52.
De Broe M E, Paulus G J, Verpooten G A, Roels F, Buyssens N, Wedeen R, et al. Early effects
of gentamicin, tobramycin, and amikacin on the human kidney. Kidney International
1984;643-52.
De Broe M E, Verbist L, Verpooten G A. Influence of dosage schedule on renal cortical
accumulation of amikacin and tobramycin in man. Journal of Antimicrobial Chemotherapy
1991;41-7.
de Champs C, Franchineau P, Gourgand J M, Loriette Y, Gaulme J, Sirot J. Clinical and
bacteriological survey after change in aminoglycoside treatment to control an epidemic of
Enterobacter cloacae. Journal of Hospital Infection 1994;219-29.
Dupont H, Carbon C, Carlet J. Monotherapy with a broad-spectrum beta-lactam is as
effective as its combination with an aminoglycoside in treatment of severe generalized
peritonitis: A multicenter randomized controlled trial. Antimicrobial Agents and
Chemotherapy 2000;2028-33.
Feld R, Valdivieso M, Bodey G P, Rodriguez V. Comparison of amikacin and tobramycin in the
treatment of infection in patients with cancer. Journal of Infectious Disease 1977;61-6.
Finley R S, Fortner C L, de Jongh C A, Wade J C, Newman K A, Caplan E, et al. Comparison of
standard versus pharmacokinetically adjusted amikacin dosing in granulocytopenic cancer
patients. Antimicrobial Agents and Chemotherapy 1982;193-7.
Francetic I, Kalenic S, Huic M, Mercep I, Makar-Ausperger K, Likic R, et al. Impact of
aminoglycoside cycling in six tertiary intensive care units: prospective longitudinal
interventional study. Croat Med J 2008;49:207-14.
Garraffo R, Dellamonica P, Drugeon H B, Etesse H, Lapalus P. A new approach to optimal
antibiotic dosage regimen by coupling pharmacokinetics and killing curve parameters.
Methods and Findings in Experimental and Clinical Pharmacology. 1990;325-32.
Karachalios G N, Houpas P, Tziviskou E, Papalimneou V, Georgiou A, Karachaliou I, et al.
Prospective randomized study of once-daily versus twice-daily amikacin regimens in patients
with systemic infections. International Journal of Clinical Pharmacology and Therapeutics
1998;36(10):561-4.
Kern W V, Cometta A, Bock R, Langenaeken J, Paesmans M, Gaya H. Oral versus intravenous
empirical antimicrobial therapy for fever in patients with granulocytopenia who are
receiving cancer chemotherapy. NEJM 1999;312-8.
Klastersky J, Glauser M P, Schimpff S C, Zinner S H, Gaya H. Prospective randomized
comparison of three antibiotic regimens for empirical therapy of suspected bacteremic
infection in febrile granulocytopenic patients. Antimicrobial Agents and Chemotherapy
1986;263-70.
Lerner S A, Seligsohn R, Matz G J.. Comparative clinical studies of ototoxicity and
nephrotoxicity of amikacin and gentamicin. The American Journal of Medicine June;62:98104.
Marik P E, Lipman J, Kobilski S, Scribante J. A prospective randomized study comparing onceversus twice-daily amikacin dosing in critically ill adult and paediatric patients. Journal of
Antimicrobial Chemotherapy 1991;753-64.
Neville L O, Brumfitt W, Hamilton Mjmt, Harding I. Teicoplanin vs vancomycin for the
treatment of serious infections: A randomised trial. International Journal of Antimicrobial
Agents 1995;187-93.
46
47
48
49
50
51
52
53
Oliveira J F, Silva C A, Barbieri C D, Oliveira G M, Zanetta D M, Burdmann E A. Prevalence and
risk factors for aminoglycoside nephrotoxicity in intensive care units. Antimicrob Agents
Chemother 2009;53:2887-91.
Piccart M, Klastersky J, Meunier F, Lagast H, Laethem Y, Weerts D. Single-drug versus
combination empirical therapy for gram-negative bacillary infections in febrile cancer
patients with and without granulocytopenia. Antimicrobial Agents and Chemotherapy
1984;870-5.
Raad II, Escalante C, Hachem R Y, Hanna H A, Husni R, Afif C, et al. Treatment of febrile
neutropenic patients with cancer who require hospitalization: a prospective randomized
study comparing imipenem and cefepime. Cancer 2003;1039-47.
Reed R L I, Ericsson C D, Wu A, Miller-Crotchett P, Fischer R P. The pharmacokinetics of
prophylactic antibiotics in trauma. The Journal of Trauma 1992;21-7.
Santré C, Georges H, Jacquier J M, Leroy O, Beuscart C, Buguin D, et al. Amikacin levels in
bronchial secretions of 10 pneumonia patients with respiratory support treated once daily
versus twice daily. Antimicrobial Agents and Chemotherapy 1995;264-7.
Van der Auwera P. Pharmacokinetic evaluation of single daily dose amikacin. Journal of
Antimicrobial Chemotherapy 1991;Supplement C 63-71.
Vanhaeverbeek M, Siska G, Douchamps J, Herchuelz A. Comparison of the efficacy and safety
of amikacin once or twice-a-day in the treatment of severe gram-negative infections in the
elderly. International Journal of Clinical Pharmacology, Therapy and Toxicology
1993;31(3):153-6.
Wiland P, Szechcinski J. Proximal tubule damage in patients treated with gentamicin or
amikacin. Polish Journal of Pharmacology 2003;631-7.
Figure S 2: Risk of bias summary: review authors' judgements about each risk of bias item
for each included study.