PEM|BRS: Procedures Central Lines: For central venous access
advertisement

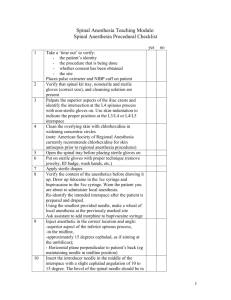
PEM|BRS: Procedures Central Lines: For central venous access, acquired and congenital bleeding disorders are relative contraindications, especially in the IJ and SC veins where hemostasis may be difficult to obtain or may result in airway obstruction. For femoral access, the child’s hip is abducted and externally rotated. A rolled towel can be placed under the ipsilateral hip for improved exposure and to create a firmer surface. Unlike in adults, use of the femoral vein is NOT associated with an increased rate of catheter-related infections compared to other central venous sites. SC Vein is the least common site used for percutaneous central venous cannulation in children due to the increased compliance of their chest wall and the small size of the chest and clavicle, which makes landmark ID more difficult. In addition, there is a high incidence of PTX and subclavian artery injury. The femoral vein is easily identifiable anatomically and does not interfere with airway management or chest compressions during resuscitation. The femoral vein can be identified 1-2 cm medial to the femoral artery pulse in the femoral triangle inferior to the inguinal ligament. When there is a weak or absent pulse, the femoral vein can be assumed to be located halfway between the pubic tubercle and the anterior iliac spine. The patient’s hip should be abducted and externally rotated. The needle is inserted 1-2 cm below the inguinal ligament at a 45 degree angle. The needle is advanced in the direction of the ischial tuberosity but should NEVER pass beyond the inguinal ligament, as this can result in bowel perforation or accumulation of a retroperitoneal hematoma. Regardless of the site, the basic steps in the Seldinger technique are to: Administer local anesthetic, prepare the site, and create a sterile field. Flush the catheters. Identify landmarks. Puncture the vein with the needle attached to syringe. Detach the syringe. Thread the J-wire through the needle and into the vessel. If premature ventricular contractions are triggered, the wire has advanced too far. Occasionally, more sustained arrhythmias can result when the ventricle is “tickled” by the wire tip. Be prepared with a defibrillator. Withdraw the needle over the wire while AT ALL TIMES maintaining control of the tip of the wire. Discard the needle. Make a small incision with a scalpel at the skin without cutting the wire. Dilate the soft tissue with dilator over the wire, again always maintaining control of the exposed wire. 1 Withdraw the dilator and thread the catheter over the wire to the desired depth, again maintaining control of the wire. Withdraw the wire and keep pressure on the catheter to prevent air embolus. Draw back and flush all ports to ascertain that all ports are intravascular. Transduce the pressure at the distal port to ascertain venous placement. For IJ and SC lines, obtain a chest radiograph to confirm that the catheter tip is outside of the right atrium and to look for pneumothorax. Secure the catheter to the skin, usually with silk sutures. Do not forget to use local anesthetic if the area was not anesthetized previously. Place a sterile dressing. The IJV and SV are more easily approached from the right side of the patient. On the right, the IJV follows a straight course and joins the right SV while the left IJV joins the SV at a more acute angle—in addition, the left thoracic duct enters the left SV at its junction with the IJV, which can hinder venous cannulation. Also, the higher left pleural dome increases the likelihood of a PTX. The IJ vein offers the most direct route to the superior vena cava (SVC). The course of the IJ is within the carotid sheath and, therefore, in close proximity to the carotid artery and the vagus nerve. Landmarks include the triangle formed by the two heads of the sternocleidomastoid muscle and the clavicle. Obviously, care should be taken to avoid puncturing the carotid artery, which lies medial to the IJ. The nondominant hand should be used for identification of the carotid artery. The needle should be directed toward the IPSILATERAL nipple. Cut down procedures are generally implemented for saphenous vein cannulation, and is usually an option if femoral vein catheterization has failed. Topical Anesthesia: TAC (tetracaine, adrenaline, and cocaine) is primarly used for lacs on the face and scalp. TAC and LET (Lidocaine, Epinephrine, Tetracaine) are contraindicated in areas of endarteriorlar supply (pinna, nasal alae, penis, and digits). Blanching of surrounding skin indicates onset of anesthesia. Contact with eyes can cause corneal injury. TAC and LET should not be used on mucous membranes or areas of extensive burns or abrasions as excessive uptake into the systemic circulation can cause toxicity. Should be used cautiously in patients with seizures as excessive amounts can cause agitation, tachycardia, seizures, and apnea. Absorption of the cocaine and lidocaine may exacerbate seizures and cardiac arrhythmias. 2 Umbilical Lines: The UA can be accessed within the first 24 hours of life and occasionally up to 7 days. The UV can be accessed up to 2 weeks of life. Both the UA and UV can be used for administration of medication or fluids. The umbilical cord should be cut transversely 0.5-2cm from the base to identify the vessels. The catheter should be passed cephalad for 4-5cm or until blood return is noted. Lower extremity ischemia can be caused by vasospasm of the UA and can be relieve with warm compresses applied to the contralateral extremity triggering a reflex vasodilation in the affected extremity. Umbilical cannulation must not be attempted in neonates with an omphalocele, omphalitis, suspicion of NEC, or peritonitis. For a high UA line, the estimated insertion depth is 1cm + distance from should to umbilical stump. For a low UV line, advance 1 cm beyond distance where blood return first occurs. For a high UV line, the insertion depth is 2/3 of the shoulder to umbilicus distance. The UA connects with the internal iliac artery then the abdominal aorta (so on x-ray, it goes caudally before cephalad). The UV joins with portal vein and the inferior vena cava. The correct position of the UVC is just above the diaphragm or, in acute resuscitations, just proximal to the umbilical stump. Umbilical vessel catheterization is a sterile procedure, and the initial steps are the same for both umbilical artery and vein. Differences in the steps for catheterizing the umbilical artery and vein include the technique for dilating each vessel, catheter advancement, some potential pitfalls, and determination of the proper placement. An umbilical artery is technically more difficult to cannulate because it is smaller, thicker-walled, and usually vasoconstricted compared to the umbilical vein. The umbilical vein needs to be cannulated only to the minimum distance that establishes adequate blood return (usually approximately 2 to 4 cm past the skin) in the setting of cardiopulmonary arrest. The UAC catheter tip lies at the level of the 3rd and 4th lumbar vertebrae for the low position. The catheter tip is above the diaphragm at the level between the 6th and 9th thoracic vertebrae for the high position. A 2000 Cochrane Review suggested that the high position is the preferred placement because it is associated with fewer clinical vascular complications and longer duration of service. UAC distance (cm) = 3 x birthweight (kg) + 9 UVC distance (cm) = [3 x birthweight (kg) + 9]/2 + 1 The tip of the UVC should be in the inferior vena cava, above the level of the ductus venosus and hepatic veins (above the diaphragm), below the level of the right atrium, with the catheter tip between T8-T9. 3 Lumbar Puncture: The lateral recumbent position and the sitting position can be used in all age groups while performing an LP. The puncture site is identified by lining up the upper aspects of the superior posterior iliac crests and finding the L3-L4 or L4-L5 interspace. The needle should be directed parallel to the bed but slightly cephalad (toward the umbilicus) in the lateral recumbent position. Topical anesthetic, subcu 1% lido, and “sucrose dipped pacifiers” have all shown efficacy in reducing pain during this procedure. Foreign Body in Airway: For a choking patient under 1 year of age, you deliver 5 back blows between the shoulder blades followed by 5 chest thrusts on the sternum. Abdominal thrusts (Heimlich maneuver) are indicated in older patients and are performed with the patient sitting or standing if conscious, or lying down if the patient is unconscious. A blind finger sweep is not recommended in the ED, but rather direct visualization of the airway by direct laryngoscopy and removal of the FB with Magill forceps. Foreign Bodies in Ear: Irrigation should never be used with vegetable matter that can expand, with button batteries, or if there is a possibility of TM perforation. In most cases, allowing FB’s to stay in the external auditory canal while the patient waits for referral is safe. Exceptions include if the FB is associated with infection and presence of a button/disk battery. IO Access: The entry site is half-way between the anterior and posterior border of the tibia, 1-2cm distal to the tibial plateau. The needle should be perpendicular to the bone and angled slightly away from the joint space. Gradual pressure with a rotational motion is applied until you feel a sudden decrease in resistance. The most common sites used are the proximal tibia, the distal tibia, and then the distal femur. The proximal tibia is used in patients until 4 years of age. After that age, the proximal tibia is more difficult to penetrate manually, and therefore the distal tibia or femur should be used. With the newer auto-injection devices, access can be obtained in patients of all ages at all sites. IO lines can be used in children of any age. IO lines should not be placed in children with osteogenesis imperfecta or osteoporosis, and bones that are fractured or infected should not be used. An overlying burn or cellulitis is a relative contraindication. In infants < 2 mo of age, the distal femur is the preferred IO site because the proximal tibia is often too thin. For the distal femur site, the IO catheter is inserted midline, 2-3cm above the femoral epicondyles. 4 The proximal tibia is an excellent site until about 4 years of age when the cortex becomes more difficult to penetrate. The site is medial and 1-2cm distal to the tibial tuberosity, on the flat part of the tibia. The distal tibial site is entered 1 cm superior to the medial malleolus, on the flat part of the tibia. Confirmation of IO placement includes: 1) Needle that stands firmly without moving 2) Aspiration of bone marrow (only possible about 50% of time—aspirated marrow can be sent for all blood tests except a CBC) 3) Easy flushing with saline Complications of IO lines include: 1) Not penetrating cortex or going into and through the other side. Large volumes of infused fluid could cause compartment syndrome. 2) Osteomyelitis 3) Cellulits (both 2 & 3) are directly related to duration of use, therefore, discontinue promptly when more definitive access obtained. 4) Fat embolism 5) Growth plate injury Dislocations: Dislocations of Digits: The longer arm of the PIP joint accounts for higher frequency of dislocations when compared to the DIP joint. Although digit dislocations are evident on physical exam, appropriate x-rays should be obtained before and after reduction to evaluate the nature of the dislocation, the alignment of the digiti and presence of any associated fractures. Digital block anesthesia should be performed before the reduction. For the purpose of closed reduction, the joint should be hyperextended while gentle longitudinal traction is applied for a dorsal dislocation. The joint should be immobilized with a splint for 1-2 weeks. An anterior shoulder dislocation is the most common joint dislocation in adolescents. In reduction by gravity, while the patient is in the prone position, the dislocated shoulder should be placed in forward flexion and slight external rotation and 5 kg weights applied to wrists for downward traction. During scapular manipulation, the superior aspect of the scapula should be pushed laterally and the scapular tip medially when downward traction by weight is applied to the affected extremity. You can also use the external rotation technique with the elbow flexed and using longitudinal traction on the humerus. TMJ is often displaced anteriorly; before attempting reduction, radiographs should be considered if there is any suspicion of fracture. A local intra-articular or IM administration of lido may help with the reduction by relaxing the lateral pterygoid and temporalis muscles. Manual reduction is done by placing the thumb against the lower posterior molars and wrapping the fingers around the angle and body of the mandible while applying slow steady pressure first downward and then posteriorly. The person 5 performing the procedure should wrap their thumbs in gauze or a splint to protect themselves from being bitten. Dislocation associated with fracture should be referred to an oral surgeon and the ED physician should not attempt a reduction of the dislocation. Hypothermia: Mild hypothermia: core body temp 34-35 C Moderate hypothermia: core body temp 30-34 C Severe hypothermia: core body temp < 30 C Passive rewarming techniques are indicated for rectal temperatures at or above 30 C and include the following: removing wet clothing, warming the room, using warm or insulating blankets. Active rewarming is indicated for rectal temperatures < 30 C (severe hypothermia) and may include bladder, gastric, peritoneal, and/or thoracic lavage using saline warmed to 40-41 C. In patients with cardiac arrest or dysrhythmias not responsive to conventional management, cardiac bypass may be necessary. Hypothermic patients should have their core body temperature monitored with a rectal probe. When the core temp falls below 30 C, the incidence of cardiac arrhythmias increases and at 28 C ventricular fibrillation may result. J waves (elevation of the J point—also called Osborn Waves) on the ECG may be seen in moderate or severe hypothermia—their presence increases the likelihood of VF. Oral/Nasal Airways: Oropharyngeal airways are used in unconscious patients. The tip of the oropharyngeal airway should reach the angle of the mandible when the flange is at the central incisors. NP airway choice: the tip should reach the lobule of the ear when the opposite end touches the ipsilateral naris. Facemasks should be the smallest size that completely covers the nose and mouth. The ventilator rate of the child should be 16-20 breaths/min. Peripheral Vascular Access: Vascular access should NOT delay or interfere with airway management in a critically ill child. Venous access should be avoided in areas distal to an injury. Areas of edema, overlying burns, or cellulitis should also be avoided. May try an EJ when other sites have been unsuccessful. EJ passes posteriorly over the SCM from the angle of the jaw. Place patient in trendelenburg with lateral neck rotation (positioning contraindicated in suspected neck injury) 6 Enterostomy Tube Replacement: Contraindications to replacing enterostomy tubes include recently placed tubes with an immature fistula tract (within 8 weeks of initial operative procedure), or the presence of peritoneal signs. May use hegar dilators or foley catheters to dilate site. Tracheostomy Tube Replacement: Respiratory distress in a patient with a tracheostomy indicates tube obstruction until proven otherwise. It is important to ascertain and understand the indication for patient’s tracheostomy. Can use ETCO2 colorimetric or capnographic devices to check placement. Do not fall into the mistake of assuming a tube in the stoma means the tube is in place—check for placement using exam and noninvasive monitoring techniques. Clearing a potentially obstructed tube: instill 1-2 cc of NS, and insert the largest suction catheter that will fit—once patient starts coughing, it is in deep enough, suction for 5 seconds (not more than 10) at 100 mm Hg. Stop if bradycardia or cyanosis develops. If suction unavailable, may try replacing the obturator into position or a smaller tube into the trach tube to dislodge the obstruction. If the obstruction still cannot be cleared, the tube must be exchanged. Ventilator Management: The problem with pressure-controlled ventilation is that a change in lung compliance will result in a change in tidal volume. Agitation or secretions may dramatically decrease the delivered gas volume. The advantage is that the risk of barotrauma and pneumothorax is reduced. The problem with volume-controlled ventilation is that the risk of pneumothorax and barotraumas is higher. The advantage is that tidal volume is preserved, regardless of changes in patient’s lung compliance. The first manifestation of a pneumothorax in this mode may be a rise in the pressure observed during the inspiration of a tidal volume. You can combine these modes using PRVC (pressure-regulated/volume controlled ventilation). Here, gas is delivered to the airway until a maximum pressure is achieved, and inspiration is continued until a predetermined tidal volume is delivered. In the ventilation of a lung with near-normal compliance and diffusion characteristics, the I:E ratio is 0.5. In a poorly compliant lung with impaired diffusion, the I:E ratio may be prolonged to 2-3 (termed, “inverted”). This is not without its consequences—when you increase length of inspiration, you decrease length of expiration. The resulting increase in MAP may decrease cardiac output. Shortened expiration may lead to gas trapping. 7 In status asthmaticus, you use permissive hypercapnea (keep arterial pH > 7.2 and pCO2 60-70) in order avoid large pressures and short E times which would otherwise increase PTX risk. Use this also for congenital diaphragmatic hernia. Initial ventilator settings: TV: 10 cc/kg (infant and toddler); 8cc/kg (child); 7 cc/kg (adolescent) Rate: 20 bpm (infant and toddler); 12 child; 10 adolescent Peak pressure: 25-30 cm H2O PEEP: 5 cm H2O Pressure support: 10 cm H2O I time: 0.8 sec (infant), 0.9 sec (toddler); 1 sec (child and adolescent) Pneumo/Hemothorax: Aggressive fluid resuscitation and administration of blood products are important for patients with massive hemothorax BEFORE significant evacuation is begun. An initial amount of blood drainage of 15cc/kg or subsequent drainage of 4cc/kg/hr x 4 hr is an indication for an open thoracotomy. An open PTX is managed FIRST with occlusion of the chest wall defect with a 3-sided dressing, followed rapidly by tube thoracostomy at an alternate site. The sole presentation of a tension PTX in a child may be respiratory distress followed by overt signs of shock. Hernia Reduction: Contraindication to manual reduction of inguinal hernia: child extremely ill with signs of toxicity from gangrenous bowel or peritoneal irritation. In a female, if an incarcerated inguinal hernia will not reduce, an incarcerated ovary is likely. Subungual Hematoma: A subungual hematoma > 30% warrants evacuation. Felon Management: For felons, use the volar longitudinal incision—start 5mm distal to the DIP joint and extend to end of the phalanx—cut down only to the dermis, explore, irrigate, drain, pack, dress, splint. Pacemakers: Placement of a magnet over the pulse generator of a pacemaker turns off all programmed functions and forces the pacemaker to pace at a fixed rate regardless of the heart’s activity. Any symptomatic patient with a pacemaker dysfunction requires transcutaneous pacing. 8 If cardioversion or defibrillation is required in a patient with a pacemaker or defibrillator, the paddles are placed as far from the pulse generator as possible. Splints: Sugar-Tong: fractures of the wrist and distal forearm Volar: Buckle fractures or sprains Thumb-Spica: scaphoid, 1st metacarpal, or first proximal phalynx Long arm: Elbow or proximal forearm Ulnar Gutter: 4th & 5th metacarpals (slight flexioin at IP joints, 90 flexion at MCP & slight extension at the wrist) Radial Gutter: 2nd & 3rd metacarpal Finger splints: apply from MCP joint around to dorsum of wrist and maintain IP joint flexion Presentation of Cardiac Tamponade: Signs of cardiac tamponade include: tachycardia, hypotension, tachypnea, narrow pulse pressure, and pulsus paradoxus. The combination of Beck’s Triad (muffled heart tones, JVD, and hypotension) is uncommonly seen. Suturing: The half-buried horizontal mattress stitch, also referred to as a corner stitch, is the preferred stitch for closing a wound flap. Because this stitch passes through the dermis of the flap, it creates less tension and, therefore, preserves the distal flap that may consist only of a thin layer of epidermis with poor vascular supply. The remainder of the wound should be closed with horizontal mattress stitches that help eliminate tension on large or gaping wounds. The basic principles of wound repair are to restore anatomy, avoid infection, and achieve hemostasis. A running suture is used for rapid percutaneous closure of long, uncomplicated wounds that align easily and are at a low risk for infection. This technique provides even tension along the length of the wound and easy suture removal. The first step is to place a single interrupted stitch at the edge of the wound, followed, without cutting the suture after the first knot is tied, with the placement of repeated running sutures at 45-degree angle bites along the entire wound. The loop of the final bite is kept loose and is used as a free end to tie the knot. Subcuticular running sutures generally are placed to close linear lacerations on the face and reduce scarring. Using absorbable sutures, a single anchoring stitch is placed at one end of the wound, followed by multiple sequential mirror-image bites at the same subcutaneous plane taken horizontally for the full length of the laceration. Both vertical and horizontal mattress sutures can be used to reduce wound tension and achieve eversion of wound edges, but these types of sutures are associated with a higher risk of ischemia of the wound edges. A vertical mattress suture is placed by taking a bite at a distance from the wound edge, crossing through the dermal tissue, and exiting through the skin at the opposite side at an equal distance. This is considered the far-far 9 portion of the suture. This is followed by turning the needle 180 degrees to reverse the direction of the suture loop and taking a smaller bite closer to the wound edge on the same side. The needle is brought out at the side of the original stitch, and the knot is tied to approximate the wound edges. This is considered the near-near portion. Both points of needle entry and exit are in the same straight line. The horizontal mattress suture is started by placing a stitch in the usual manner and bringing it out at the opposite side. The second bite is taken 0.5 cm from the first exit site and brought back to the original starting site at the same distance for the knot to be tied. The v-shaped laceration with the flap is closed by using a half-buried horizontal mattress suture, where the needle is introduced through the skin of the nonflap portion and passed horizontally through the dermal portion of the flap (buried), with the suture loop completed by bringing the needle out through the skin on the opposite side of the nonflap portion of the wound. In some instances, it is advisable to extend the v-shaped laceration to a V-Y laceration to reduce tension at the flap. There is no such thing as a half-buried vertical mattress suture. Orofacial Nerve Blocks: V1/Opthalmic Division Supplies: Forehead, upper eyelid, nasal bridge and tip Point of exit from skull: Supraorbital foramen Landmarks for block (supraorbital): Inject 0.5 to 1 cm depth medial to supraorbital notch V2/Maxillary Division Supplies: Lower eyelid, upper lip, anterior maxillary teeth Point of exit from skull: Infraorbital foramen Landmarks for block (infraorbital): Insert needle anterior to first maxillary premolar while marking infraorbital foramen (0.5 cm below infraorbital notch) with finger; inject at depth of 1 to 2 cm V3/Mandibular Division Supplies: Mandible, lower lip, chin, mandibular teeth Point of exit from skull: Mandibular foramen Landmarks for block (inferior alveolar): Grasp mandible between index finger and thumb of nondominant hand, marking coronoid notch with the intraoral digit; hold syringe along occlusal plane of the mandible, aiming slightly superior in adolescents and adults and slightly inferior in younger children; inject at depth of 1 to 1.5 cm 10 Mental Nerve Supplies: Lower lip and chin Point of exit from skull: Mental foramen Landmarks for block (mental): Insert needle over mandible along a line that crosses the supraorbital and infraorbital foramen and the premolars (palpate mental foramen); inject at a depth of 0.5 cm A line can be drawn from the supraorbital notch, through the pupil of the eye, through the infraorbital notch and foramen, across the maxillary and mandibular premolars, and through the mental foramen. In this way, all three branches of the trigeminal nerve can be easily located. For an infraorbital block, the index finger of the nondominant hand is used to palpate a depression about 0.5 cm below the infraorbital notch, which marks the site of the infraorbital foramen. The thumb or fingers of the same hand are used to retract the upper lip. The dominant hand is used to insert the needle into the mucolabial fold just anterior to the apex of the first premolar tooth. The needle should be advanced no more than 1 to 2 cm from the insertion point toward the infraorbital foramen and along the axis of the tooth. The tip of the index finger helps to guide the needle and prevent advancement of the needle to the orbital cavity. Once the tip of the needle is positioned above the infraorbital foramen, 1 to 2 mL of anesthetic is injected. An alternative approach involves injecting the anesthetic through the skin directly into the infraorbital foramen. However, caution must be exercised with this approach because the nerve may be damaged if the needle is advanced into the foramen itself. Injection of local anesthetic at a depth of 1 to 1.5 cm into the coronoid notch of the mandible along the occlusal plane produces an alveolar nerve block; the needle should be directed slightly superior to the occlusal plane in adolescents and adults and slightly inferior to the occlusal plane in younger children. The alveolar nerve is the largest branch of the mandibular division, or V3, of the trigeminal nerve and provides innervation to the mandibular teeth, lower lip, and chin on the involved side. Local anesthetic administration medial to the supraorbital notch provides a supraorbital block, with anesthesia of the ipsilateral forehead. Injection of local anesthetic into the mental foramen provides anesthesia to the lower lip and chin on the ipsilateral side. Supraperiosteal infiltration provides anesthesia to a single tooth. A buccal approach is used to advance the needle 1.5 cm into the mucolabial fold of the corresponding tooth. One to two milliliters of anesthetic is infiltrated along the periosteum at the apex of the root. Due to the porosity of the maxilla, supraperiosteal infiltration is effective for the maxillary teeth throughout life. However, because the mandible is significantly denser and less porous in adults, this form of anesthesia useful only for maxillary teeth in older adolescents and adults. 11 Orofacial anesthesia involves local or regional infiltration of an anesthetic agent to provide pain relief or to prevent pain associated with repair of facial injuries or infections. The decision to use local infiltration or a regional block is based on the location and type of injury or infection, concern regarding distortion of landmarks with local infiltration, damage to or distortion of normal block landmarks by injury or infection, and level of cooperation of the patient. An absolute contraindication to orofacial anesthesia is a documented allergy to local anesthetic agents. Injection of anesthesia into or through infected or grossly contaminated tissues is relatively contraindicated. Small, clean wounds are usually amenable to local infiltration. Regional nerve blocks generally require the use of less anesthetic, usually only 1 to 2 mL for orofacial blocks, reducing the risk of toxicity or adverse reactions. Significant wounds to cosmetically important areas, such as lacerations through the vermilion border, may be better served with regional anesthesia to avoid distortion of key landmarks. Multiple wounds in the same nerve distribution may be repaired with fewer injections, less time, less anesthetic, and less discomfort using a single regional block. Preparatory steps can increase the likelihood of success of orofacial nerve blocks. Depending on the patient’s age, degree of anxiety, and level of cooperation, consideration should be given to the use of distraction, restraints, medical anxiolysis, or procedural sedation before beginning the procedure. For those blocks administered via the intraoral route (supraperiosteal infiltration, infraorbital, inferior alveolar), the application of topical mucosal anesthesia before performing the block can reduce or eliminate the pain of needle insertion. The area initially is dried with a gauze pad, followed by application of topical mucosal anesthetic (20% benzocaine or 5% to 10% lidocaine) to the insertion site. Local anesthesia should be achieved within 30 to 90 seconds. A 27-gauge needle generally is recommended for injection in orofacial blocks; the use of larger-bore needles increases the pain associated with the procedure. Use of warmed and buffered anesthetic solutions can further minimize the patient’s discomfort. Following infiltration of 1 to 2 mL of anesthetic, at least 5 minutes is required to achieve regional anesthesia. Failure to achieve anesthesia can result from improper technique, anatomic variation, insufficient anesthetic volume, or inadequate time before performing the procedure. Other complications of orofacial anesthesia include intravascular injection of anesthetic, improper needle position causing injury to adjacent structures, and allergic reaction to the anesthetic. Suprapubic Bladder Aspiration: Collection of a urine specimen is indicated for a febrile infant younger than 2 months of age as part of evaluation for possible sepsis. Suprapubic bladder aspiration (SPA) or transurethral bladder catheterization (TUC) are the two standard methods used. The simplest and most efficient of these methods is TUC, but if this is not possible due to anatomic or technical difficulties, SPA should be considered. Before undertaking this approach, it is prudent to maximize the likelihood of success by ensuring that urine is present in the bladder. Administration of an intravenous bolus of normal saline before an attempted SPA is an appropriate course of action. Antibiotics can then be administered 12 after collection of the urine sample. Repeated attempts at TUC in the presence of labial adhesions, use of urine from the diaper, and manual lysis of the adhesions are inappropriate. A urine bag may be considered if SPA is beyond the technical abilities of the clinician. SPA has been in use since the early 1950s. If urine is obtained, the sensitivity for detection of urinary tract infection by this procedure approaches nearly 100%, making it the diagnostic gold standard. Due to the invasiveness, pain, and greater failure rate for SPA compared to TUC (successful attempts range from 23% to 90%), TUC has become the method of choice for children younger than 2 years of age. Although studies have found that TUC is less painful, the approach through a relatively nonsterile urethra does introduce a greater likelihood of bacterial contamination of the urine specimen. Beyond 2 years of age or after the child is toilet trained, the clean-catch technique is used for urine collection because of its relative ease and noninvasiveness. Specimens collected by urine bag can be used to screen for urinary tract infection in children between 2 months and 2 years of age when they are not sick enough to require immediate antibiotics. If the specimen is positive (presence of leukocyte esterase or nitrite, bacteria evident on microscopic examination of a Gram stain specimen, or detection of more than 5 white blood cells on a noncentrifuged urine specimen), then repeat urine specimen collection is indicated via TUC or SPA to confirm the infection. Antibiotics for presumed urinary tract infection should not be started on the basis of findings from specimens collected by urine bag alone. Indications for SPA are: difficulty in accessing the urethra in children younger than 2 years of age due to labial adhesions, foreskin adhesions, or any other technical problem that prevents collection of urine by TUC. Fecal incontinence in a child who has gastroenteritis is a relative indication. Contraindications include some genitourinary tract abnormalities, infection of the abdominal wall at the collection site, bleeding diathesis, and neutropenia. Studies have shown that pain associated with SPA can be reduced with the use of topical anesthetics and that the success of SPA is related to the patient’s hydration status. SPA success rates have increased when the procedure is used in conjunction withultrasonography. Ultrasonography allows for determination of bladder volume and guidance for aspiration by showing where the bladder is closest to the abdominal wall. The minimum recommended bladder measurements for successful collection of urine are 2 cm or more in transverse and anteroposterior diameters or at least 10 mL of measured bladder urine volume. Under sterile conditions, the patient’s abdominal wall is prepped with appropriate antiseptic and the patient is held in the frogleg position. Local anesthesia with injection or cream is recommended to reduce pain. The bladder is percussed to determine if it is full before attempting SPA. The entry point is 1 to 2 cm above the symphysis-pubis in the midline. Use of a 22-gauge 1.5-inch needle attached to a 3- to 5-mL syringe is recommended. The direction of insertion is 10 to 20 degrees from perpendicular, angled toward the umbilicus. The plunger on the syringe is pulled back after the skin is pierced to create negative pressure until urine returns. If this is not successful, the needle can be directed more perpendicularly without removing it. If this attempt is also unsuccessful, 13 the patient should be hydrated and the attempt may be repeated in 30 to 60 minutes. Complications of SPA are rare and include intestinal penetration, infection of the abdominal wall, and transient hematuria. These can be avoided by proper identification of landmarks and use of sterile technique. Rare cases have been reported of bladder wall thickening after SPA in patients who have bleeding diatheses. Development of abdominal wall abscess has been reported in neonates who have fever and transient neutropenia. There is no evidence of bacteremia after SPA in patients who have documented urinary tract infection. When ultrasonographic guidance is used, care must be taken to avoid applying excessive pressure with the probe onto the bladder to prevent early micturition, which can be prevented by manual pressure on the urethral meatus. Tissue Adhesives: Tissue adhesives are an alternative to suturing for low-tension wounds that are linear and less than 4 cm in length, do not abut mucosal surfaces, and are not grossly contaminated. Multiple studies have shown equivalent rates of wound dehiscence and infection in wounds closed with tissue adhesive compared with suture closure if the wounds are appropriately chosen. Tissue adhesives should not be used on wounds that cross joints (because they are considered high tension) or on the hands (because frequent washing can prematurely break down the tissue adhesive). Similar cosmetic outcomes are achieved with tissue adhesive and suture closure. Because no sutures or staples need to be removed, no follow-up visit is required. As always, parents should be instructed return with the child if there are signs or symptoms of infection. Wound cleansing and debridement are the most important steps to prevent secondary infection. For the boy described in the vignette, the wound can be cleaned after administration of a topical anesthetic such as LET (lidocaine, epinephrine, and tetracaine). Irrigation into an open wound without local anesthesia is painful and likely would make the toddler uncooperative for further care, including application of the tissue adhesive. The wound needs to be dry and well approximated for appropriate application of tissue adhesive. Cyanoacrylate tissue adhesive bonds the epithelial layer of skin when the monomer chemically changes to a polymer in the presence of moisture of the skin surface. This exothermic reaction, resulting in heat generation (that may be felt by the child), is exacerbated by the presence of blood or irrigation fluid. If the wound is not well approximated, tissue adhesive enters it and keeps the edges apart. Some practitioners recommend approximating the wound with tape strips before applying tissue adhesive, rather than approximating it manually, which decreases the chance of gluing the holder to the patient. When the wound is in the facial area, the clinician should take care to prevent tissue adhesive from dripping into the eyes by positioning the patient so the adhesive rolls away from the eye. Alternately, the clinician can place a barrier of petrolatum or antibiotic ointment between the eye and the laceration. Tissue adhesive may be removed with a petrolatum-based product if it inadvertently enters the wound or adheres to an unintended surface. A systematic analysis indicated that use of tissue adhesive is less time-intensive than suturing, with a labor time of 8.6 minutes for sutures and 4.0 minutes for tissue adhesives. 14