Altering the Circuit When Using DTI to Anticoagulate
advertisement

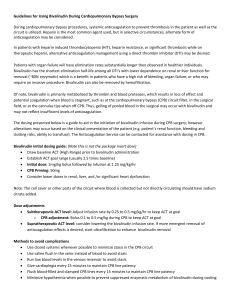
Alteration of the CPB Circuit When Using Direct Thrombin Inhibitors Robert C. Groom, MS, CCP Director of Cardiovascular Perfusion Maine Medical Center Portland, Maine Medical Center groomr@mmc.org Introduction Thrombocytopenia is one of the most common laboratory abnormalities found among hospitalized patients.i Serologically proven Heparin Induced Thrombocytopenia (HIT) is a severe thrombotic disorder that occurs in 1.5 -3% of patients with heparin exposure. Do to the intense activation of the hemostasis mechanism that occurs with cardiopulmonary bypass (CPB), substantial levels of anticoagulation with heparin is requisite to prevent thrombosis within the CPB circuit and within the patient.ii,iii However, re-exposure of HIT patients to heparin results in catastrophic complications and death. Heart surgery patients with HIT may be managed safely using a direct thrombin inhibitor (DTIs) for anticoagulation. However, some modification of the CPB circuit and perfusion techniques is necessary. The aim of this lecture is to: 1) Review alteration of the CPB circuit that are necessary when direct thrombin inhibitors are used in place of heparin 2) Describe patient management strategies and monitoring of anticoagulation during CPB when DTIs are used 3) Discuss challenges that may arise during such procedures . While, none of the currently available anti-coagulants are ideal, according to Poetzsch and Madlener the ideal drug should have the following characteristics: 1). The agent should be effective in minimizing activation of coagulation during CPB. 2) A rapid and simple method of monitoring its anti-coagulating effects should be available to avoid inappropriate under- or over anticoagulation. 3) Rapid and complete reversibility of the anti-coagulating effects is important to minimize postoperative bleeding complications.iv Currently, the most common heparin alternative anticoagulation strategy involves the use of DTIs as a substitute for unfractionated heparin. Bivalrudin and Argatroban are most common agents. Bivalrudin is more frequently used because of its shorter half-life. Of note, an alternative method of managing anticoagulation is the administration of a platelet inhibitor (ie. iloprost or tirofiban) at a dose sufficient to block platelet Groom- 1 Alteration of the CPB Circuit When Using Direct Thrombin Inhibitors aggregation prior to administration of a full dose of unfractionated heparin with continuous infusion of the platelet inhibitor until the heparin has been reversed. CPB Circuit Alterations/Management A CPB circuit comprised of tubing or components that are coated with heparin (ie. Carmeda coating Medtronic, Minneapolis, MN) should not be used. While closed circuits may have a theoretic advantage, both open (hard shell venous reservoir) or closed (collapsible venous reservoir) circuit have been used with success.v Of major concern are the areas of stasis within the circuit that are exposed to blood where the flow of blood is intermittent. These areas must be identified and steps should be taken to prevent prolonged stasis (for more than 15 minutes) in these areas. Common areas where this may occur and strategies to mitigate the stasis are shown in the table below: Area Cardiotomy Reservoir Venous Reservoir Oxygenator shunts Arterial Filter Purge line Arterial Filter bypass bridge Strategy Avoid holding blood in the cardiotomy reservoir Maintain minimum safe level (600-800mls). Remove excess Blood and store in transfer bags with citrate anticoagulant) Open shunts briefly every 10-15 minutes for 3 sec. Keep filter purge open during CPB Remove clamp to bridge for 1 sec every 10-15 minutes Blood Cardioplegia System Cardioplegia Delivery Line Flush continuously / or dose @15min intervals / or flush between doses. Administer dose @15min/or flush between doses Arterial Line and Cannulae Post CPB Flush cannulae by infusion of 50ml of blood every 3 minutes Not uncommon to see clotted pooled blood. Use a pericardial sum Blood in the pericardial well or To keep blood evacuate from these areas. plural spaces Bivalirudin has a 25 minute half-live with 80% of it being eliminated by circulating proteases and approximately 20% of the drug by the kidneys. It may be necessary to reduce the continuous infusion rate in patients with renal dysfunction. It is important to note that elimination of the drug is slower at lower temperatures. Approximately 15 to 20 minutes before separation from bypass, the continuous infusion of the drug should be discontinued. Immediately following bypass, ultrafiltration with a 65,000 Dalton filter has been successfully used to increase the removal rate of direct thrombin inhibitors followingvi,vii Use of Groom- 2 Alteration of the CPB Circuit When Using Direct Thrombin Inhibitors hypothermia will prolong the half-life of bivalirudin and must be considered in managing the continuous infusion. Furthermore, it is important to rewarm completely before separation from bypass to allow more rapid elimination of the drug. Argatroban has a half-life of 39-51 minutes which may result in more loss of blood following CPB due to the longer elimination period.v Argatroban is eliminated by the liver and may the drug of choice for patients with compromised renal function. Following separation from bypass the arterial and venous lines should be connected and blood should be circulated and a continuous infusion of the DTI should be administered in the circuit to prevent thrombus formation. The blood in the pump should be processed with a cell saver within fifteen minutes of stopping the continuous infusion to the pump and cessation of circulation of the blood in the circuit. Anticoagulation Monitoring Careful monitoring of anticoagulation is critical when DTIs are used. The type of point of care test used will depend which DTI is used. Optimal anticoagulation tests for various drugs are as follows; Argatroban –ACT Danaparoid-Antifactor Xa level Lepirudin – ECT Bivalirudin- ECT preferred (ACT has been reported). Murphy and Marymount have reported the following recommendations from the ACCP.viii,ix Clotting time must be monitoring during CPB to determine adequate anticoagulation and it is used following CPB to evaluate the elimination of the DTI and the return of hemostasis. Several studies have shown that the ecarin clotting time (ECT) has better correlation than Activated Clotting Time (ACT) with actual drug levels particularly at higher plasma concentrations (r = 0.71 for Groom- 3 Alteration of the CPB Circuit When Using Direct Thrombin Inhibitors Hemochron ACT vs. r = 0.90 for the TIM-ECT) and inhibition of coagulation. The ECT can be performed with the TIM-ECT test card, designed for use with the Thrombolytic Assessment System (TAS, Bayer Diagnostics; Rapidpoint Coag Analyzer, Morrisville, North Carolina).x ECT tests may also be carried out using an ecarin clot activator with the Thromboelastographxi,xii or with the Rotational Thromboelastometry (ROTEM)xiii. However, many centers use a standard ACT point of care test. A clotting time of 2.5 times the baseline ACT value is the widely accepted target. Challenges Management of coagulation during CPB with a direct thrombin inhibitor must be carried out with the utmost precision xiv,xv,xvi. The patient’s sensitivity to heparin must be clearly communicated to all members of the team and vials of heparin should be removed from medication trays in the operating room and care units to prevent inadvertent administration. A continuous infusion of the DTI must be maintained during CPB and be discontinued prior to the planned separation from CPB. It is not uncommon to see clots forming in the pericardial and plural spaces during CPB. The CPB circuit should be frequently inspected for formation of clot in the cardiotomy reservoir, venous reservoir, oxygenator and arterial filter. The perfusion team should anticipate the possible need to replace some or all of these components However catastrophic hemorrhage and associated massive transfusion has been reportedxvii and is likely more common that thromboembolism in the cardiac surgery setting. An autotransfusion device with a calcium chelating anticoagulant (CPDA or ACD) should be available for blood loss following separation from CPB. The team should anticipate excessive bleeding after separation from bypass and have appropriate topical hemostatic agents, sufficient replacement blood components, point of care testing to determine platelet, plasma, and red cell replacement requirements and rapid volume infusion capability. i Warkentin T, Levine MN, Horsewood P, Roberts RS, et al. Heparin-induced thrombocytopenia in patients treated with low molecular weight or unfractionated heparin. N Engl J Med 1995;332:1330-5. ii Edmunds LH Jr. Blood-surface interactions during cardiopulmonary bypass. J Cardiovasc Surg 1993; 8:404–410. iii Slaughter TF, LeBleu TH, Douglas JM Jr, Leslie JB, Parker JK, Greenberg CS. Characterization of prothrombin activation during cardiac surgery by hemostatic molecular markers. Anesthesiology 1994; 80:520–526. iv Poetzsch and Madlener Management of Cardiopulmonary Bypass Anticoagulation in Patients with Heparin-Induced. Thrombocytopenia chapter in Heparin Induced Thrombocytopenia 3 rd Edition Warkentin TE and Greinacher A ISBN: 0-8247-5625-8. Marcel Dekker, Inc., Cimarron Road, Monticello, New York 12701, U.S.A. 2004. Groom- 4 Alteration of the CPB Circuit When Using Direct Thrombin Inhibitors v Veale JJ, McCarthy HM, Palmer G, and Dyke CM. Use of Bivalirudin as an Anticoagulant During Cardiopulmonary Bypass. JECT. 2005;37:296–302. vi Saravanan P, Rege K, and Falter F. Use of continuous venovenous hemofiltrationfor reversal of anticoagulation with Lepirudin Post Cardiopulmonary bypass in a patient with HIT. J Card Vasc Anes 21;2007:269- 72. vii Koster A, Merkle F Hansen R et al. Elimination of recombinant hurudin by modified ultrafilteration during subbing simulated CPB Asssessing different filter systems Anesth Analg 2000: 91;265-269. viii Murphy GS and Marymont JH. Alternative Anticoagulation Management Strategies for the patient with Heparin-Induced Thrombocytopenia undergoing cardiac surgery. J thorac Cardiovasc Anes 2007;21:113-26. ix Warkentin T , GreinacherA HIT Recognition, treat and prevention. The seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004: 126:311S-37S. x Cho L, Kottke-Marchant K, Lincoff AM etal. Correlation of Point-of-Care Ecarin Clotting Time Versus Activated Clotting Time With Bivalirudin Concentrations. The American Journal of Cardiology 2003;91: 1110-1012. xi Carroll RC, Chavez JJ, Simmons JW, Snider CC, Wortham DC, Bresee SJ, Cohen E. Measurement of patients' bivalirudin plasma levels by a thrombelastograph ecarin clotting time assay: a comparison to a standard activated clotting time. Anesth Analg. 2006 May;102(5):13169. xii Koster A,Buz S, Krabatsch T, Dehmel F, Hetzer R, Kuppe H and Dyke C. Monitoring of Bivalirudin Anticoagulation During and After Cardiopulmonary Bypass Using an Ecarin-Activated TEG® System. Journal of Cardiac SurgeryVolume 23, Issue 4, pages 321– 323, July/August 2008 xiii Schaden E, Schober A, Hacker S, Kozek- Langenecker S. Ecarin modified rotational thromboelastometry a point of care alternative to monitor the direct thrombin inhibitor argatroban. Central European Journal of Medicine Wien Klin Wochenschr DOI 10.1007/s00508-013-0327-1 xiv Dyke CM, Koster A, Veale JJ, Maier GW, McNiff T , Levy G. Preemptive use of bivalrudin for urgent on-pump coronary artery bypass grafting in patients with potential HIT. Ann Thorac Surg 2005;80:299-303 xv Koster A, Spiess B, Chew D. Effectivenesss of bivalirudin as a replacement for heparin during CPB in patients undergoing CABG . Am J Cardiol 2044;93:356-9. xvi Koster A, Yeter A, Buz S etal. Hemostatic activation during normothermic CPB with Bivalirudin; results of the second pilot study to assess”on-pump” CABG with bivalirudin J Thorac Cardiovasc Surg 2005;129:1391-4. xvii Gasparovic H, Natahan NS, Fitzgerald D, and Aranki SF. Servere Argatroban induced coagulatopathy in a patient with a history of HIT. Ann Thorac Surg 2004;78e89-91. Groom- 5