A 7-year-old girl came to the clinic complaining of toothache on her

A 7-year-old girl came to the clinic complaining of toothache on her lower right teeth.
She was accompanied by her mother. According to her mother, at birth she was diagnosed to have “hole on her heart”. The mother also claimed that her daughter had no sleep for the last 3 nights due to pain and been treated by antibiotics and analgesics previously. She went to a dentist and the dentist filled the toot with “temporary” filling. The mother claimed that the daughter was reasonably cooperative during previous treatment.
HISTORY TAKING
History of complaint should include the history of pain including site, onset, characteristic, severity, radiation, recurrence, alleviating factor, aggravating factor, associated symptoms such as swelling and presence of salty taste. Treatment received by patients including type of treatments and efficacy of treatments. The mother claimed that the girl cannot sleep for the last 3 nights due to pain. The pain has been treated by analgesics and antibiotic previously. There is also temporary filling on that tooth done by a dentist and the girl was reasonably cooperative during the treatment. Her mother requests for management of her child's problems.
In past medical history, her mother informed that the girl has “hole” on her heart at birth.
Further information regarding this should be asked such as treatments that have been received for example history of surgery of prosthetic heart valve, frequency and location of follow-up, any medication taken as well as any symptoms associated with heart problems experienced by patients for instance shortness of breath, cyanosis, lethargy, fever and malaise. Besides that, the last attack of these symptoms and its management should also be asked. In addition, any history of infective endocarditis and its management should also be asked.
Besides patient’s information regarding heart problem, other diseases such as blood dyscriasis, kidney disease, any allergies to medication, food and material such as latex gloves and metals as well as other types of medication taken besides medication for heart problems should also be asked. History of hospital admission should also be asked. If it is present, the causes, time, site of admission and treatment received must be asked.
In past dental history, the information needed include are the last dental visit and the treatment received. Besides that, further information regarding temporary filing on 85 should be
asked such as when and why it was done. The behaviour of the patients during dental treatment should be assessed. History of extraction should be asked including complications such as prolonged bleeding and infection. Plaque control of patient should be assessed including risk factors for caries development such as diet consumption.
Family history of congenital heart disease and significant hereditary disease should be asked amongst parents, siblings or grandparents. Any significant risk factor in the family should be considered.
Diet history is important to be asked including sweet food consumption, bottle feeding in the aspect of frequency, type of drinks and amount of drinks. Any parafunctional habit such as thumb sucking and bruxism should be asked.
Extraoral examination including face, temporomandibular joint (TMJ), lips, mouth opening, lymph nodes, any abnormalities at the neck, et cetera should be examined.
Abnormalities in the presentation of skin such bluish colur, any swelling should be noted as it might be the manifestation of heart disease.
Upon intraoral examination, the complaint site which is at lower right side, 85 (O) and 46 are in question. At 85, there is presence of temporary restoration which is still intact. Further assessment including condition of adjacent structure, presence of sinus tract , tenderness to percussion, tenderness to palpation, presence of deep periodontal pocket, mobility, pulp vitality, bleeding should be carried out. Presence of caries should be observed with the signs of inflammation.
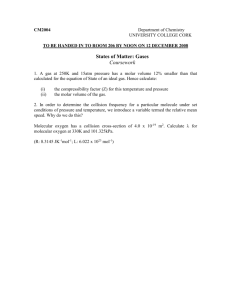
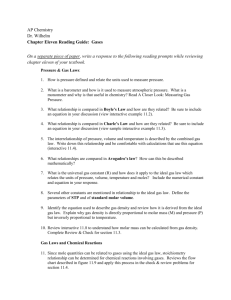
INVESTIGATION
Radiographs are essential for accurate diagnosis. The principle in taking radiograph in children must be to minimise exposure to ionising radiation while aiming to provide the most appropriate treatment. Orthopantomogram (OPG) of the patient shows that all developing permanent teeth are present except for all third molars. All permanent first molars have erupted.
All permanent incisors have erupted. Other permanent teeth still not erupt.
Periapical radiograph of the patient shows radiolucency on 55 which may indicate caries involving enamel, dentin and pulp. There is radiopacity on 85 which may indicate restoration at enamel, dentin pulp area. There is also radiolucency on 26 which may indicate caries involving
enamel and dentin area. There is also radiolucency on 16 which may indicate caries involving enamel and dentine area. There is radiolucency on 46 which indicate caries involving enamel and dentin area. There is also widening of periodontal ligament (PDL) space at distal and mesial of 85.
Pulp sensibility testing must be carried out on 85 and 46. However, this is highly related to cooperation of patients. Thus, dental officers must ensure that result obtained true.
Tenderness on percussion and palpation of the teeth should be noted. Cold test, hot test and electrical pulpal test might be carried out.
FOR 85 and or 46:
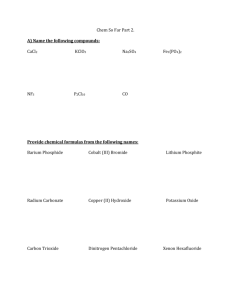
Differential Diagnoses :
Acute Irreversible pulpitis
Acute periapical abscess
Acute periapical periodontitis
Pulp necrosis
Definitive diagnosis
Acute irreversible pulpitis o Disturb sleep o Recurrent pain even after temporary filling o No periapical radiolucency o Widening of Periodontal Ligament (PDL)
Treatment options
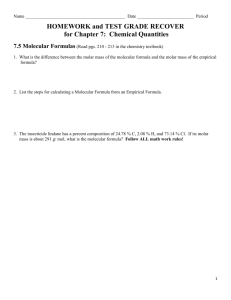
CONDITIONS
Vital pulp status
TREATMENT OPTIONS
Pulpotomy +/- Stainless Steel Crown
(SSC)
Partial pulpotomy +/- SSC
Non-vital pulp status Pulpectomy +/- SSC
Extraction (balancing & compensating) space maintainer
No associated systemic diseases Pulpotomy +/- Stainless Steel Crown
(SSC)
Partial pulpotomy +/- SSC
Pulpectomy +/- SSC
Extraction (balancing & compensating) space maintainer
With associated systemic disease (Ischemic heart disease)
Treatment aims :
Relieve pain
Remove active disease
Preserve tooth structure
Maintain space
Restore function
Modify risk factor
Preserve vitality
Improve oral hygiene
Extraction (balancing & compensating) space maintainer
DISCUSSION
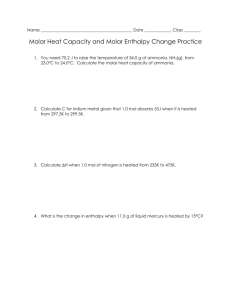
Antibiotics prophylaxis
According to American Heart Association (AHA) Guidelines regarding antibiotic prophylaxis, cardiac conditions associated with highest risk of adverse effect from endocarditis for which prophylaxis with dental procedure is reasonable.
The heart conditions that need antibiotic prophylaxis including prosthetic cardiac valve or prosthetic material used for cardiac valve repair, previous infective endocarditis, certain specific and serious Congenital Heart Disease (CHD) such as unrepaired cyanotic CHD with prosthetic heart material or device whether placed by surgery or by catheter intervention during first 6 month after the procedure because endotheliazation of prosthetic material occurs within six months after the procedure and/or repaired CHD with residual defects at the site or adjacent to the site of a prosthetic patch or prosthetic device which inhibit endotheliazation. In addition, cardiac transplantation recipients who develop cardiac valvulopathy also need to have antibiotic prophylaxis.
Dental procedures that require antibiotic prophylaxis are those procedures involving manipulation of gingival tissues, the apical region of teeth or perforation of oral mucosa. Dental procedures are extraction, routine cleaning, scaling and root debridement, periapical root canal treatment, fitting orthodontic bands, placing subgingival medications, biopsy and suture removal.
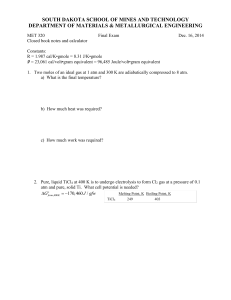
Regimen: Single Dose 30 to 60 minutes before procedure
SITUATION
ORAL
AGENT
Amoxicillin
UNABLE
TAKE ORALLY
TO Ampicillin
OR
Cefazolin or ceftriaxone
ALLERGIC TO
PENICILLINS OR
AMPICILLIN-
ORAL
Cephalexin*
OR
Clindamycin
OR
Azithromycinor clarithromycin
ADULTS
2g
2g IM or IV
1g IM or IV
2g
600mg
500mg
CHILDREN
50mg/kg
50mg/kg IM or IV
50mg/kg IM or IV
50mg/kg
20mg/kg
15mg/kg
ALLERGIC TO
PENICILLINS OR
AMPICILLIN-
UNABLE
TAKE ORALLY
TO
Cefazolin or ceftriaxone
OR
Clindamycin
1g IM or IV
600mg
50mg/kg IM or IV
20mg/kg IM or IV
First permanent molars of poor prognosis
A child can often present with a developing dentition affected by one or more first permanent molars of poor prognosis which may need an enforced extraction or require some consideration toward elective extraction in the form of balancing or compensating extractions.
In this case, one of the treatment options of 46 if it were the cause of toothache in the patient with congenital heart disease is the extraction of 46. According to the guideline for the extraction of first permanent molars in children, the management of first permanent molar, there are a number of factors that may influence the decision making process. These include a child’s social background, their likely ability to cooperate with restorative or orthodontic treatment,
prevention and oral hygiene practice within family, as well as any local difficulties in accessing
NHS restorative or orthodontic treatment.
In some condition, the enforced extraction of one first permanent molar should be accompanied by the elective balancing or compensating extraction of another. Balancing extraction is defined as the removal of the first molar from the contra-lateral side of the same dental arch. Meanwhile, compensating extraction refers to removal of the first molar from the same side of the opposing dental arch. The factors that influence whether a first molar is recommended for either a balancing or compensating extraction are firstly in the case which first molar requires enforced extraction, secondly the overall condition and long term prognosis, thirdly the teeth present within the developing dentition particularly third molars and lastly the underlying malocclusion of the patient.
As a general rule, compensating extraction of an upper first molar is often recommended when extraction of the lower is required. This is to prevent over-eruption of an unopposed upper first molar and prevention of mesial movement of the lower second molar. There is, however little definitive data with regard to these effects in the literature. Balancing the extraction of healthy first molars is not generally recommended in either arch and there is little evidence that unilateral extraction will adversely affect the centerline. Ideally, the first permanent molar extractions should be followed by successful eruption of the second molars to replace them and ultimately, the third molars to complete the molar dentition. However, achieving this can be complicated by a number of factors. The factors that might complicate the process are firstly the timing of first molar extraction. This factor will have an important influence on the subsequent eruptive position of the second molar particularly in the lower arch. Secondly, the third molar development cannot always be confirmed at the time extraction decisions have to be made. In addition, consideration also needs to be given to the consequences of first molar extraction for developing occlusion especially in the presence of an underlying malocclusion.
In many cases, at least one first permanent molar may require enforced extraction because of its poor condition and unfavorable long-term prognosis. At this stage, a decision should also be made regarding the need for elective extraction of any other teeth. This decision will be influenced primarily by their condition and the underlying occlusion. Before any extraction decisions are made, good quality radiographs are required to show the presence, condition and developmental stage of all teeth in the dentition. If any teeth in the permanent dentition are
missing or in a poor eruptive position, this can significantly affect the decision-making process.
Ideally, an orthodontic opinion should be obtained preferably from the orthodontist responsible for future treatment, whenever this is practically possible. In the absence of a definitive opinion and if the use of local anaesthetic is practical, enforced extraction should be carried out and advice sought regarding further elective extractions. On the other hand, if the general anaesthesia is the only option, advice on elective extractions should be obtained beforehand if at all possible to prevent the risk of multiple anaesthesia.
Regarding the ideal timing for extraction of first permanent molar in developing dentition, in the upper arch the developmental position of an unerupted second permanent molar generally ensures that this tooth will achieve a good occlusal position following extraction of the first permanent molar. While in the lower arch, achieving a good occlusion is more dependent upon the timing of the first permanent molar extraction. Generally, whenever practical the lower first molar should be extracted when there is radiographic evidence of early dentin calcification within the second molar root bifurcation within the second molar root bifurcation. This usually occurs within a chronological age range of 8 to 10 years. If the first molar is extracted before the age of eight years, there is often no radiographic evidence of third molar development. In addition in the lower arch the second premolar can drift distally into the extraction space, tip and rotate and the labial segments can retrocline with an accompanying increase in the overbite.
Otherwise, if the first molar is extracted during the later stages of second molar eruption, the second molar may tip mesially and rotate mesio-lingually producing spacing and poor occlusal contacts while the erupted second premolar can migrate distally.
Extraction of a first permanent molar is rarely the extraction of choice. However favorable spontaneous development of the dentition and space closure can be expected in the majority of cases. It is also possible to achieve good results following the removal of these teeth using fixed appliances although treatment times tend to be increased. It is not advisable to extract a healthy premolar for orthodontic purposes if the first permanent molar in the same quadrant is heavily restored. A number of general guidelines on treatment planning first permanent molar extraction cases for a number of malocclusions are available. As a general rule, if in doubt, get the patient out of pain, try and maintain the teeth and refer for an orthodontic opinion.
From orthodontic perspective, in class I cases if a lower first permanent molar is compromised, a balancing extraction in the lower arch and a compensating upper first permanent molar extraction should be considered. This is particularly important for mixed dentition case. Otherwise if an upper first permanent molar is compromised, a balancing extraction in the upper arch should be considered to prevent a midline shift if deemed to be necessary. However a compensating first permanent molar extraction in the lower arch is generally not required.
Meanwhile in class II division 1 cases, if a compromised lower first permanent molar is extracted the upper first permanent molar may be in occlusion with the lower second primary molar or second premolar tooth. This contact will usually prevent the upper first permanent molar from over erupting, therefore a compensating upper first permanent molar extraction may not be required. If an upper first permanent molar is compromised, it may be ideal to maintain the compromised upper first permanent molar until the upper second permanent molar has fully erupted. In certain cases, a temporary restoration or endodontic dressing may be required depending on the associated symptoms.
In class II division 2 cases, lower arch extractions are best avoided and it is best to consult orthodontic opinion before extracting in the lower arch. Meanwhile if upper first permanent molar is compromised, it may be preferable to maintain the compromised upper first permanent molar until the upper second permanent molar is fully erupted. Last but not least, in class III cases, a specialist orthodontic opinion is warranted prior to extracting any permanent teeth. In appropriate extraction of teeth can severely hamper future orthodontic treatment in this case.