HIVand conditions handout
advertisement
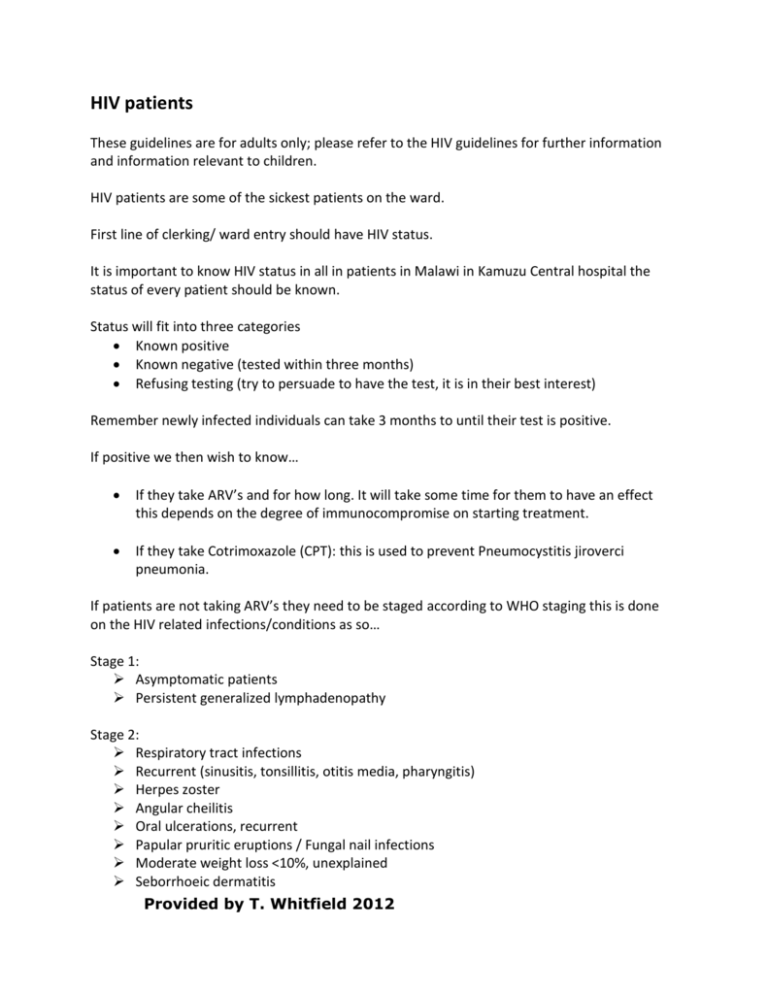
HIV patients These guidelines are for adults only; please refer to the HIV guidelines for further information and information relevant to children. HIV patients are some of the sickest patients on the ward. First line of clerking/ ward entry should have HIV status. It is important to know HIV status in all in patients in Malawi in Kamuzu Central hospital the status of every patient should be known. Status will fit into three categories Known positive Known negative (tested within three months) Refusing testing (try to persuade to have the test, it is in their best interest) Remember newly infected individuals can take 3 months to until their test is positive. If positive we then wish to know… If they take ARV’s and for how long. It will take some time for them to have an effect this depends on the degree of immunocompromise on starting treatment. If they take Cotrimoxazole (CPT): this is used to prevent Pneumocystitis jiroverci pneumonia. If patients are not taking ARV’s they need to be staged according to WHO staging this is done on the HIV related infections/conditions as so… Stage 1: Asymptomatic patients Persistent generalized lymphadenopathy Stage 2: Respiratory tract infections Recurrent (sinusitis, tonsillitis, otitis media, pharyngitis) Herpes zoster Angular cheilitis Oral ulcerations, recurrent Papular pruritic eruptions / Fungal nail infections Moderate weight loss <10%, unexplained Seborrhoeic dermatitis Provided by T. Whitfield 2012 Stage 3: Fever, persistent unexplained, intermittent or constant, >1 month Oral hairy leukoplakia Pulmonary tuberculosis (current) Tuberculosis (PTB or EPTB) within the last 2 years Anaemia, unexplained < 8 g/dl Neutropaenia, unexplained < 500 /mm3 Thrombocytopaenia, chronic < 50,000 /mm3 Severe weight loss >10% and/or BMI <18.5kg/m2, unexplained Diarrhoea, chronic (>1 month) unexplained Oral candidiasis Severe bacterial infections (pneumonia, empyema, pyomyositis, bone/joint, meningitis, bacteraemia) Acute necrotizing ulcerative stomatitis, gingivitis or periodontitis Hepatitis B or C infection Stage 4: Pneumocystis pneumonia Candidiasis of oesophagus, trachea, bronchi or lungs Extrapulmonary tuberculosis Kaposi’s sarcoma HIV encephalopathy Cryptococcal meningitis or other Extrapulmonary cryptococcosis Disseminated non-tuberculous mycobacterial infection Cryptosporidiosis, chronic with diarrhoea Isosporiasis >1 month Disseminated mycosis (coccidiomycosis or histoplasmosis) Symptomatic HIV-associated nephropathy or cardiomyopathy Progressive multifocal leukoencephalopathy Cerebral or B-cell non-Hodgkin lymphoma HIV wasting syndrome (severe weight loss + persistent fever or severe weight loss + chronic diarrhoea) Bacterial pneumonia, recurrent severe Chronic herpes simplex infection (orolabial, genital / anorectal >1 month or visceral at any site) Cytomegalovirus infection (retinitis or infection of other organs) Toxoplasmosis of the brain Non-typhoidal Salmonella bacteraemia, recurrent Invasive cancer of cervix Leishmaniasis, atypical disseminated Provided by T. Whitfield 2012 Cotrimoxoazole therapy (CPT) This drug is used in all HIV positive adults to prevent PCP pneumonia, diarrhoea, malaria and other HIV related diseases. It is given as 480mg BD for life. Contraindications to CPT are… Jaundice Renal failure Developing Stevens-Johnson syndrome Pregnant women cannot take within 14 days of taking Sulfadoxine/Pyrimethamine Starting Antiretroviral therapy After staging anyone who is found to be stage 3 or 4 should be referred to start ARV therapy. In addition ARVs should be given to all patients who are pregnant or breast feeding. CD4 count is measured in patients who are unwell and do not meet stage 3/4 criteria, if the CD4 count is ≤ 350cells/mm3 then the patient is eligible for ARV therapy. ARV therapy ART requires combining 3 different ARVs that act differently in order to avoid development of drug‐resistant HIV. If possible try to keep the patient on a first line regime 1st line regimens: Are easy to prescribe and easy to take, have a low risk of side effects and require no lab monitoring for toxicity. There are 6 different 1st line regimens if a patient has a significant side effect switch them to an alternative 1st line regimen without delay. Alternative regimens are chosen by substituting only the ARV responsible for the side effects. 2nd Line regimens: These are a lifeline for patients who have confirmed treatment failure on 1st line regimen (usually due to poor adherence in the past). Moving from 1st to 2nd line ART is called switching. 2nd line regimes o Contain a completely different class of ARVs (proteinase inhibitors) o Are more complicated to prescribe and take o Can have more side effects o There are 3 different 2nd line regimens. The appropriate 2nd line regimen is determined by the 1st line regimen that the patient was taking when failing. 3rd Line regimens: Provided by T. Whitfield 2012 These are ‘salvage therapy’ and a last resort for patients failing on second line in spite of good adherence. This requires confirmation of drug resistant virus using genetic analysis in the lab. 3rd line can currently only be initiated on a study basis by a specialised expert ARV clinician. 3rd line regimes o Very expensive o Can have more side effects and be difficult to take Abbreviations of ARV’s 3TC Lamivudine ABC Abacavir AZT Zidovudine d4T Stavudine ddl Didanosine EFV Efavirenz LPV/r Liponivir/ritonavir NVP Nevirapine TDF Tenofivir ZDV Zidovudine Classification of ARVs ARVs are classified according to their action… Nucleoside reverse transcriptase inhibitors include: stavudine (d4T), zidovudine (AZT), abacavir (ABC), lamivudine (3TC) and tenofivir (TDF). Non-nucleoside reverse transcriptase inhibitors include: nevirapine (NVP) and efavirenz (EFV). Protease inhibitors are liponivir and ritonavir (LPV/r). Regimes for ARVs Standard ARVs 1st line (Regimen 1 ‐ 6) and 2nd Line (Regimen 7 ‐ 9) Regime 1 d4T 30mg /3TC 150mg /NVP 200mg Indication This is first line therapy except for those breast feeding, pregnant or already on TB therapy. Provided by T. Whitfield 2012 This regime is started with a starter pack (gradual increase in drugs). Contraindications to regime 1: Jaundice / hepatitis Side effects: Neuropathy Hepatitis/ Skin rash Lipodystrophy Lactic acidosis Treatment failure Switch to regime: 2 5, 6, NS 3 5 5 NS 79 Regime 2 AZT 300mg / 3TC 150mg / NVP 200mg This is standard for children under 15 years of age. This regime is started with a starter pack Contraindications to regime 2: Anaemia <8g/dl, Jaundice / hepatitis Side effects: Anaemia Hepatitis/ Skin rash Lipodystrophy Lactic acidosis Treatment failure Switch to regime: 1 5, 6 43 5 5 NS 79 Regime 3 d4T 30mg / 3TC 150mg/EFV 600mg Contraindications: History of psychiatric illness Side effects: Neuropathy Hepatitis/Skin rash Psychiatric disorder Lipodystrophy Lactic acidosis Treatment failure Switch to regime: 2 5, 6, NS 6 1 NS 5 5 7 Regime 4 AZT 300 mg /3TC 150mg /EFV 600mg Contraindications: History of psychiatric illness, Anaemia <8g/dl Side effects: Anaemia Lipodystrophy Lactic acidosis Provided by T. Whitfield 2012 Switch to regime: 35 5 59 Hepatitis/ Skin rash Psychiatric disorder Treatment failure 6 2 NS 79 Regime 5 TDF 300mg /3TC 300mg /EFV 600mg This regime is 1st choice for pregnant women, breastfeeding women and adults already on TB Treatment. Contraindications: History of psychiatric illness, Renal failure, Child under 12 years Side effects: Renal failure Hepatitis/ Skin rash Psychiatric disorder Treatment failure Switch to regime: lower dose or 2 6 6 NS 8 Regime 6 TDF 300mg / 3TC 300mg/NVP 200mg This regime starts with a starter pack. Contraindications: Jaundice/Hepatitis, Renal failure, Child under 12 years Side effects: Renal failure Hepatitis/ Skin rash Treatment failure Switch to regime: lower dose or 2 5 NS 8 Regime 7 TDF 300mg / 3TC 300mg/ LPV/r 200/50 Contraindications: Renal failure, Child under 12 years Side effects: Renal failure Nausea, vomiting Switch to regime: 8 NS Regime 8 AZT 300mg / 3TC 150mg /LPV/r 200/50 Contraindications: Anaemia <8g/dl Side effects: Anaemia Nausea, vomiting Provided by T. Whitfield 2012 Switch to regime: 7 NS Conditions where different ARVs may be needed Anaemia (<8g/dl) Treatment can be started within 7 days of diagnosis with d4T/3TC/NVP Active TB Treatment should be started within 14 days of diagnosis TB treatment + ARVs can be started on the same day if the patient is stable Don’t delay either TBT or ARVs Treatment: AZT/3TC/EFV or TDF/3TC/EFV Jaundice Refer to District or Central Hospital Start ARVs after investigation and stabilisation Treatment: d4T/3TC/EFV 1st trimester pregnancy Start ARVs in the 2nd trimester with TDF/3TC/EFV In labour (new HIV diagnosis) Start ARVs as soon as possible with TDF/3TC/EFV Renal failure Refer to District or Central Hospital Start treatment within 7 days of diagnosis with AZT/3TC/EFV Monitoring ARVs ARVs should be switched if there is no improvement in CD4 count or patient condition after 2 months of starting ARV therapy. ARVs should also be switched if the patient deteriorates and CD4 count drops despite good compliance. Serious side effects of ARVs Patients should be told to stop ARVs and present to hospital immediately if they develop any of the following symptoms… Yellow eyes/ skin Severe abdominal pain and vomiting Shortness of breath Blistering skin rash involving eyes, genitals or mouth Provided by T. Whitfield 2012 Common complications of ARV treatment Lactic acidosis This severe life threatening condition occurs most commonly with stavudine (d4T) and didanosine (ddI), though also with patients on zidovudine (AZT), abacavir and lamivudine (3TC). It is more likely to occur in female patients and those who are pregnant or obese. Symptoms of lactic acidosis include fatigue, stomach pain, nausea, vomiting and shortness of breath, though symptoms can come on gradually. When assessing these patients increased respiratory rate and tachycardia are early signs. The diagnosis is made by measuring the pH of the blood and the lactate level though this is not always possible in Malawi. A pH <7.35 or lactate > 5 mmol/L indicates a poor prognosis. Individuals without any signs or symptoms may have asymptomatic hyperlactaemia in which it may be simply appropriate to switch ARVs. Treating lactic acidosis involves stopping all ARVs and giving IV fluids at 3 litres a day minimum until symptoms settle. Jaundice/ Hepatotoxicity This is more common in those with pre-existing liver damage (Hepatitis B,C, alcoholics), renal failure or those on protease inhibitor therapy. Severe hepatotoxicity can occur with Nevirapine (NVP) but also with efavarenz (EFV) and abacivir. When treating these patients the ARVs must be stopped and other causes looked for (alcohol, Gall stones etc). Treating what is found appropriately. Stevens-johnsons syndrome This is a blistering skin rash present on most of the surfaces of the skin and involving the mouth, eyes and genitals. This condition can be caused by other illnesses such as streptococcal infection or diabetic drugs. The common cause in Malawi is due to Nervirapine (NVP) therapy though cotrimoxazole (CPT) can also cause this condition. To treat Stevens-Johnson syndrome stop all ARV treatment, ensure the patient is fully hydrated with good urine output, (usually given IV fluid at least 3L per day). Antibiotics such as cefuroxime1g bd are given to cover skin infection and the eyes are covered with tetracycline eye ointment. Potassium per manganite soaks are also prescribed to prevent skin infection. Provided by T. Whitfield 2012 Immune reconstitution syndrome (IRS) This is caused when the immune system becomes over-aggressive as it recovers due to ARVs and attacks an already existing infection. This usually occurs within days to week of starting ARVs. Often immune reconstitution syndrome can unmask a previously unknown infection or worsen a disease that was improving. Common infections in IRS TB Kaposi sarcoma Cryptococcal Meningitis Herpes zoster Hepatitis Treat the underlying infection and continue the ARVs. Psychiatric disorders Efavirenz (EFV) can cause a range of psychiatric disorders from insomnia to severe dellusions this is especially likely if there is pre-existing psychiatric disorder. It should be withdrawn in people with psychiatric disorders. Abacavir and lamivudine(3TC) should also be avoided in people with psychiatric disorders. Peripheral Neuropathy This is a common side effect of Stavudine (d4T), didanosine (ddI) and zidovudine (AZT). The patient will complain of numbness from the feet upwards, they should have their ARV regime switched. HIV related illness Skin and mucosal problems Dermatophytes This is a fungal rash usually found on hairy or sweaty regions of the skin such as the groin, axilla, scalp and face. This condition can occur in non-reactive patients but is more common in HIV. Provided by T. Whitfield 2012 The rash is often itchy, greasy and scaly. It is treated with an antifungal cream such as clotrioxazole or miconazole in the first line and with ketoconazole tablets 200mg BD 7days if these are ineffective. Candida oral/oesophageal This presents with white/red plaques anywhere in the mouth cavity. Oesophageal candidiasis will cause pain and difficulty swallowing (dysphagia). Oral candidiasis may be treated first patients treat with nystatin solution 4ml QID for 10-14 days. If there is persistent candidiasis or a suggestion of oesophageal candidiasis then fluconazole 200mg for 14 days should be given. Herpes Zoster Chicken pox is primary disease causing widespread vesicular rash. Can remerge as shingles in immunocompromised, this follows a dermatomal distribution (doesn’t cross the patients midline) and begins with pain followed by the rash. Look for secondary infection especially if it involves the eyes. The shingles is caught before the blisters burst then acyclovir 800mg 5 times a day for 7 days can improve symptoms. Tinea corporis, cruris, pedis Round red plaques with a scaly edge on the body, head or feet but may be widespread across the body. Treat with Whitfield’s ointment, Gentian-violet paint or clo-trimazole cream twice daily for 3-4 weeks. Griseosulfin tablets 500mg bd for 3-4 weeks can be used as second line if no response. Neurological problems Meningitis All below present with the symptoms of meningitis such as headache, neck pain, reduced GCS, seizures and photophobia. Ensure airway ABV approach in all patients and if confusion/fits/ ↓GCS ensure blood sugar checked. Acute bacterial meningitis Provided by T. Whitfield 2012 The symptoms and presentation are as above. Always suspect this in patients with low GCS and treat immediately if any suspicion. Treatment is cefuroxime 2g bd with lumbar puncture to confirm diagnosis. TB meningitis This is more common in immunosuppressed individuals and has a poor prognosis. It is difficult to confirm a diagnosis of TB meningitis, on LP acid fast bacilli are rarely seen there is elevated lymphocytes, low sugar and raised protein. The biggest clue for diagnosis is a history of progressive illness with fever and night sweats over a few weeks. Chest x-ray may be appropriate to look for pulmonary TB. Treatment for TB meningitis is 9/12 of standard TB therapy. Steroids at a dose of prednisolone 1mg/kg/day for one month should be given and then tailored down over several weeks. sterioscan be given to improve the GCS. Cryptococcal Meningitis (CCM) This occurs soley in immunocompromised individuals the onset of symptoms is gradual over several weeks. The opening pressure on lumbar puncture is very high and often squirts across the room. The diagnosis is made by india ink staining of yeasts in the CSF or positive CRAG antigen in the CSF or blood. Treating CCM is with fluconazole 1200mg od for 2/52, then 800mg for 8/52 then 200mg od for life. Amphoteracin B 1mg/kg od every day for 7 days can also be added to this regime if available but can cause renal failure so ensure U+E checked beforehand. Repeat LPs can be done daily to relive symptoms of raised ICP, up to 20ml taken each time. Space occupying lesions These occur more commonly in HIV they present with focal neurology often like a stroke with weakness/numbness on one side of the body but with a more gradual onset, headache, vomiting and fits. Space occupying lesion is best confirmed by CT or MRI scan, unfortunately this is not possible in most instances in Malawi. Provided by T. Whitfield 2012 Steriods can be used to reduce cerebral oedema in life saving situations though they can cause false recovery of symptoms making people believe their treatment is working when another diagnosis should be sought. Common causes of space occupying lesion in HIV patients are Toxoplasma: Tested for with toxoplasma antigen test, it is likely if the CD4 count <50cells/mm3. It is often treated blindly in patients with suspected SOL and CD4 count <150 cells/mm 3. Toxoplasma is treated with Sulphadiazine and pyrimethamine (SP) 4 tablets Bd then 2 tablets BD for at least four weeks. Cryptococcoma: diagnosed and treated as for cryptococcal meningitis. Lymphoma: often disseminated lymphadenopathy, needs to be diagnosed on biopsy, can look similar to Tuberculoma. Tuberculoma: Difficult to diagnose without TB elsewhere in the body. Often it is treated when the there is evidence of TB elsewhere. If the CD4 count>150 cells/mm3 or there is no response to SP then TB treatment can be tried. Respiratory problems Bacterial pneumonia The patient will have symptoms of a productive cough of green sputum with shortness of breath and fever. Chest x-ray will show consolidation/infiltrates confined to a specific lung area, unless atypical pneumonia which can show reticulo-nodular shadowing in the upper lobes. White cell count is usually elevated. If there is severe pneumonia then treat intravenously with cefuroxime 1g od or x-pen 3MU TID and chloramphenicol 1g TID. Severe pneumonia often needs oxygen. Mild pneumonia may be treated with oral antibiotics such as amoxicillin 500mg TID adding erythromycin or doxycycline if ineffective. Pneumocystis jiroveci (carinii) pneumonia (PCP) This disease tends to characterized by progressive shortness of breath over a few weeks with a dry cough or fever. Chest x-ray will show a ground glass appearance initially focused around the hilar region. Provided by T. Whitfield 2012 Cd 4 count will be < 200 cells/mm3 and the white cell count tends to be normal. If the diagnosis is uncertain between PCP and bacterial pneumonia then it is appropriate to treat both. PCP is treated with oxygen to improve sats, co-trimoxazole (CPT, Bactrim) 4x 480mg tablets TID for 21 days followed by a life time of preventative CPT (480mg bd). 40mg prednisolone is given bd for 5 days then od for five days then 20mg for five days then gradually weaned down by 5mg every 3 days. Second line therapies for PCP include clindamycin 300mg tid for 3 weeks or primaquinine 300mg od for 3 weeks. Tuberculosis This presents with a chronic cough productive often bloody cough with TB symptoms such as weight loss, fever and night sweats. Chest x-ray may show widespread dense consolidation or cavitation in the presence of a patient who looks not too unwell. A reticulo-nodular (small spotty) pattern can be seen in patients with millary TB. Pleural effusion is very common in TB and when tapped will show an exudate with a lymphocyte predominance. TB is treated with regular TB combined medication regime for 6 months. Gastrointestinal problems The Malawi HIV guidelines recomned a stepwise approach to managing HIV patients with diarrhoea. The first priority in management is to correct dehydration by giving oral rehydration salts 5ml/kg every 4 hours and after every episode of diarrhea or IV fluids if severe dehydration or unable to drink. Step 1: This involves treating all bacterial causes of diarrhea as well as isopora and ciclospora. In HIV patients bacterial diarrhoea is commonly caused by Salmonella, Shigella, typhoid and Campylobacter all of which can cause bloody diarrhea, fever and abdominal pain. Treat these individuals with co-trimoxazole 960 mg TID for 7 days. If bacterial diarrhea is suspected and no improvement seen give ciprofloxacin 500mg bd. Step 2: Treats amoebic dysentery, giardia, microspore and clostridium diarrhoeas Amoebic dysentery produces chronic bloody diarrhea with abdominal pain but no fever. Provided by T. Whitfield 2012 Giardia causes a persistent watery diarrhea going on for several weeks Treatment for these organisms is with metronidazole 400-500mg TID for 7-14 days. Step 3: Treats microspore and helminth causes of diarhoea and involves giving albendazole 400mg BD for 14 days. Malignancy in HIV Kaposi Sarcoma This condition is characterised by single or multiple purple patches or nodes mainly mouth, skin, conjunctiva, lung, and gastrointestinal tract. There may be enlarged lymph nodes or oedema present also. The diagnosis is usually clear given skin and oral mucosal findings. Consider KS even without skin or oral lesions if no response to TB therapy within 4 weeks The treatment of KS involves analgesia, symptomatic relief and ARVs. If chemotherapy is needed depends on the stage of the KS. For KS stage T0 (skin KS without oedema) chemotherapy can be delayed and only given if there is no improvement after 3 months on ARVs For KS stage T1 (KS in mouth or internal organs, nodular skin KS, skin KS with oedema): Immediate chemotherapy is needed. Contraindications for chemotherapy: Severe PN Hb<10g/dl Platelet count <50/mm3 Jaundice Pregnancy 1st Line chemotherapy: Vincristine Each cycle consists of 6 doses. It must not leak when given IV as infiltration into the tissues causes burns, document therapy and response in the patients health passport. Look for progress of the lesions at every visit. The dose is 2mg IV. Provided by T. Whitfield 2012 Review the progress after each cycle, stop the chemotherapy if there is severe neuropathy or constipation. If the lesions have cleared the therapy can also be stopped. If the lesions are improving give another cycle if there is no improvement or worsening disease give second line therapy. 1) Initial cycle: 1 dose every 7 days for 6 weeks 2) Second cycle: 1 dose every 14 days for 12 weeks 3) Final cycle: 1 dose every 28 days for 6 months 2nd Line chemotherapy: Vincristine and Bleomycin Over a life time an adult can have no more than 400 units of Bleomycin. Bleomycin should be stopped immediately if any sign for lung fibrosis (incl. cough, shortness of breath) are seen. Bleomycin is given in one combined dose of 15 units every 14 days until 400 units is reached or until a good response is seen. The patient will receive vincristine at the appropriate cycle at the same time. The patient will need to be referred for 3rd line chemotherapy (doxorubicin) if there is still little response this is to be done at a specialist centre. Cervical cancer There are no early symptoms of cervical cancer therefore active screening is needed in all HIV patients. The patient should be referred to gynaecology clinic if there is abnormal vaginal discharge, pain during sex or abnormal bleeding. Provided by T. Whitfield 2012