Disclaimer - American Society of Exercise Physiologists
advertisement

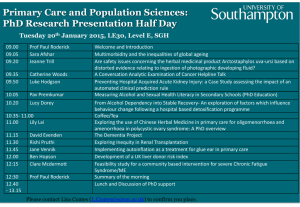
58 Journal of Exercise Physiologyonline December 2014 Volume 17 Number 6 Official Research Editor-in-Chief Journal of the American Tommy Boone, PhD, MBA Review Society Board of Exercise Physiologists Todd Astorino, PhD Julien Baker, PhD ISSN 1097-9751 Steve Brock, PhD Lance Dalleck, PhD Eric Goulet, PhD Robert Gotshall, PhD Alexander Hutchison, PhD M. Knight-Maloney, PhD Len Kravitz, PhD James Laskin, PhD Yit Aun Lim, PhD Lonnie Lowery, PhD Derek Marks, PhD Cristine Mermier, PhD Robert Robergs, PhD Chantal Vella, PhD Dale Wagner, PhD Frank Wyatt, PhD Ben Zhou, PhD Official Research Journal of the American Society of Exercise Physiologists ISSN 1097-9751 JEPonline Post-Exercise Hypotension between Different Protocols of Resistance Training for Beginners M. Macedo1, A. S. Silva², R. R. Olher3, H. J. Coelho Junior2,4, R. Palmeira2, Ricardo Y. Asano2,5 Universitário UNIRG – Gurupi/TO – Brazil, 2Universidade de Mogi das Cruzes – Brazil, 3Universidade Católica de Brasília – Brasília- Brazil, 4Universidade Estadual de Campinas – Campinas – Brazil, 5Faculdade de Ciências e Letras de Bragança Paulista – Brazil 1Centro ABSTRACT Macedo M, Silva AS, Olher RR, Coelho Junior HJ, Palmeira R, Asano RY. Post-Exercise Hypotension between Different Protocols of Resistance Training for Beginners. JEPonline 17(6):58-65. Evidence indicates that resistance training (RT) promotes postexercise hypotension (PEH), which is considered important in preventing hypertension (HTN). But, the most efficient RT protocol to keep blood pressure normal is still unclear. The aim of this study was to analyze and compare the impact of different RT protocols on PEH. Twelve male and female subjects (22.0 ± 1 yrs of age with a mass body index of 24.9 ± 2 m2) participated in this study. The sample size was calculated using the GPower 3.0.10 software for a statistical power of 80% with an alpha of 5% (P≤0.05). The subjects performed in randomized order two experimental RT protocols: (a) the strength training (ST) protocol suggested for beginners (80% 1RM); and (b) the muscular endurance (ME) protocol (65% 1-RM). Heart rate and blood pressure were measured before and every 15 min of recovery after the session (up to 60 min). While both protocols resulted in PEH, the ST protocol produced a longer PEH response than did the ME protocol. Therefore, the findings indicate that for beginners, the ST protocol is more effective in producing PEH. Key Words: Hypotension, Resistance Training, Hypertension 59 INTRODUCTION For several decades, health care organizations have indicated that physical exercise is helpful in the treatment if not the prevention of hypertension. Specifically, the American College of Sports and Medicine (1) and the JAMA (6) have published comprehensive reports, including but not limited to, “Exercise and Hypertension” and the “Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure,” respectively. Regarding the modality of physical exercise, recent meta-analytic data have shown that resistance training (RT) can be an effective tool to decrease blood pressure in subjects with normal blood pressure and in subjects with elevated blood pressure (i.e., hypertension) as well as certain risk factors (e.g., body fat) for cardiovascular disease (CVD) (7,8). Furthermore, RT is very useful in building and maintaining muscle strength and power in adults, which helps to promote an increase in health and quality of life (15,20). In addition to the chronic effects of RT on blood pressure, CVD risks and quality of life, beneficial effects can also be observed immediately after exercise (e.g., such as a decrease on blood pressure levels below the resting levels). For example, Asano and colleagues (2) and and Asano et al. (3) reported that blood pressure levels can decrease below to the resting levels. This phenomenon is called post-exercise hypotension (PEH) (2,3). However, there is no consensus in the literature about which intensity of RT is more efficient in producing PEH (3,11,14,16). Bentes et al. (4) and Mohebbi et al. (14) did not observe a difference in PEH between low (40%) and high intensity (80%) RT. On the other hand, Lizardo and Simões (11) observed a PEH response in diastolic blood pressure (DBP) and mean arterial pressure (MAP) after low intensity session (30%). In turn, Polito et al. (16) observed that the duration of PEH on systolic blood pressure (SBP) was dosedependent of the intensity of RT. Therefore, the aim of this study was to analyze the PEH response on normotensive young adults during different RT protocols that are suggested for beginners lifting weights (e.g., muscle endurance and hypertrophy). If there is a significant PEH response resulting from RT, it would be reasonable to conclude that RT may help to prevent hypertension in young adults as they age (21). METHODS Subjects This study was developed in accordance with the Declaration of Helsinki, in Resolution 196/96 of the National Health Council. All subjects signed a free consent form that contained that explained the research objectives and risks to their integrity during the study. The Ethics Committee of the Centro Universitário-UNIRG approved this experiment. The trial was performed based on a crossover methodology (one group performed both sessions). The sample was composed of 12 subjects (8 males and 4 females; 22.0 ± 1 yrs old, body mass index 24.9 ± 2 m²). The minimum sample size was calculated using the software GPower 3.0.10, for minimum statistical power of 80% with an alpha of 5% (P≤0.05). Potential subjects were excluded from the study if they: (a) had cardiovascular complications, participated in a rehabilitation program 6 months prior to the study, or physical problems that might stop the RT protocol; (b) smoked; or (c) used beta-blockers and/or diuretics. For the safety of the subjects, the pre-exercise resting blood pressure (BP) could not exceed a SBP of 160 mmHg and a DBP of 100 mmHg. Furthermore, if during 60 exercise blood pressure was ≥250 mmHg for systolic or increased 12 mmHg after the warm-up, the exercise protocol was stopped. The subjects performed strength training (ST) and muscular endurance (ME) at random sequence with a minimal interval of 2 wks between sessions. The design of both resistance exercise sessions was based on the strength training guidelines of American College of Sports Medicine (1). The subjects did not perform exercise during the interval sessions. On a first visit, the subjects performed a test of one-repetition maximum (1-RM) in all exercises to be used in protocols for determining the maximum load on each exercise. The procedure began with a warm-up of ~4 to 5 min that was followed by low intensity static stretching. The warm-up was initiated with a load of ~50% of 1-RM. The test began 2 min after the warm-up. The subjects were instructed to perform two full repetitions with maximum range of motion. If the two repetitions were fulfilled in the first attempt or if they were not completed correctly, a second attempt was initiated after a recovery interval of 3 to 5 min with a higher load (first option) or lower (second chance) than previously used. A third and final attempt was repeated if the load corresponding to a single maximum repetition had not been determined. The load recorded as 1-RM was the one in which the subject was able to perform only a single correct and complete repetition. The transition interval between exercises was of 3 to 5 min (5). Experimental Protocols The muscular endurance (ME) session consisted of 65% (low intensity) of 1-RM, 3 sets of 15 repetitions with a resting interval of 60 sec between sets and a moderate cadence (2-sec concentric [CON]: 2-sec eccentric [ECC]). The strength training session consisted of 80% (high intensity) 1-RM, 3 sets of 8 repetitions with a rest interval of 90 sec between sets and a moderate cadence (2-sec CON: 2-sec ECC). The exercises in both sessions were the bench press, high rowing, leg extension, leg curl, triceps curl, and biceps curl. Determination of Cardiovascular Parameters and PEH Systolic blood pressure, DBP, and HR were measured using the INMETRO Brand® Premium RS380 device. Mean arterial pressure (MAP) was determined by the following equation: MAP = (SBP + 2 x DBP) ÷ 3. After arriving at the laboratory, the subjects remained seated in the upright sitting position for 15 min prior to determining the baseline (rest) measurements. At the end of the experiment, the subjects remained in the sitting position to determine the occurrence of PEH. The recovery hemodynamic parameters were measured after 15 min (rec15), 30 min (rec30), 45 min (rec45), and 60 min (rec60) after the end of the exercise. Statistical Analyses To compare SBP, DBP, and HR between the experimental sessions, descriptive statistics was used. The data were presented as average and standard deviation (±SD). The data were submitted to the Shapiro Wilk test for normality. For comparison of the sample-dependent variables between the sessions, the ANOVA split-splot (mixed ANOVA) with Bonferroni correction for intragroup and intergroup comparisons was applied. The level of significance was set at P≤0.05, and the statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 15.0. 61 RESULTS During exercise, the ME session demonstrated an increase in HR compared to the baseline measure. In turn, the ST session demonstrated a trend that was not statistically significant (P>0.05). There were no significant changes after the end of exercise (Figure 1.) Figure 1. Mean and Standard Deviation of Heart Rate (HR) during the ME and ST Sessions Compared to Rest (P≤0.05). Although the SBP demonstrated a trend in producing PEH in both sessions, the responses were not significantly different from each other (P>0.05) (Figure 2). Figure 2. Mean and Standard Deviation of Systolic Blood Pressure (SBP) during the ME and ST Sessions Compared to Rest (P>0.05). 62 During recovery, PEH was observed at 15 min, 30 min, and 45 min in the ST session. In turn, ME resulted in PEH only at the 15 min point of recovery. When the sessions were compared in the same time, no significant difference was observed (Figure 3). Figure 3. Mean and Standard Deviation of Diastolic Blood Pressure (DBP) during the ME and ST Sessions Compared to Rest (P≤0.05). The subjects’ MAP responses indicated significant changes (P≤0.05) in PEH at 15 min, 30 min, and 45 min of recovery for the ST session. There were no statistical differences in MAP for the ME session (Figure 4). Figure 4. Mean and Standard Deviation of the Mean Arterial Pressure (MAP) during the ME and ST Sessions Compared to Rest (P≤0.05). 63 DISCUSSION The primary finding in this study indicate that the ST session promoted PEH for a longer time on DBP in sedentary young adults than the ME session. Also, the data indicate that ST resulted in PEH via the subjects’ MAP response, which occurred after the ME session. To our knowledge, this is the first study to demonstrate prolonged PEH on DBP after high intensity RT in comparison with low intensity RT in healthy young adults. Other studies (11,16) have observed no differences between high and low RT (4) or PEH just after a low intensity RT session without significant changes after high resistance exercise. This discrepancy in the results may be explained by the differences between the subjects of the different studies. In the present study, all the subjects were sedentary for at least 6 months while the other studies (4,11,16) evaluated practitioners of resistance exercise (4,11,16). In spite of the studies that evaluated subjects with normal levels of blood pressure, the adaptations in the cardiovascular system subsequent to engaging in RT programs may have decreased the effects of a single session. This point cannot be ruled out. The changes in DBP and MAP after exercise may be explain by the balance between cardiac output (CO) and peripheral vascular resistance (PVR) (18). Changes in blood volume, due to the shift of plasma liquid to the interstitial space, may also have facilitated the spreading of blood. This overall effect may be directly linked to the decrease in venous return and, therefore, the decrease in cardiac preload (12,18). As a result, the changes in CO and PVR are likely the primary reason for the decrease in DBP and MAP (18). Then, too, since high intensity exercise has been demonstrated to increase nitric oxide (NO) more so than low intensity exercise (2,3), an increase in NO may have worked to either maintain or decrease PVR and the resulting changes in DBP and MAP. Some studies (13,19) has shown that inhibition of NO lead to increase on MAP (~15%) and PVR (~64%). The fact that the RT and PEH research findings differ in volume and intensity as well as in the order of the RT exercises makes it difficult to interpret the best relationship of these variables to PEH. There are several limitations in regards to the findings in this study. First, the lack of a control session to analyze the resting values vs. the exercise values should be evaluated. Second, the determination of blood pressure for a longer period of time after the sessions and, third, the fact that the time and/or consumption of food were not standardized prior to data collective need clarification as possible confounding variables. CONCLUSIONS While both sessions (protocols) resulted in PEH, the ST session produced a longer PEH response than did the ME session. Thus, in terms of the likelihood of preventing hypertension, the findings indicate that the ST protocol is more effective. Address for correspondence: Ricardo Yukio Asano, PhD, University of Mogi das Cruzes, 200 Dr. Cândido Xavier de Almeida Souza Avenue. Mogi das Cruzes, 08770490, Brazil. E-mail: ricardokiu@ig.com.br Telephone: (55) 11 97011-5500 Fax: (55) 11 40331129 64 REFERENCES 1. American College of Sports Medicine. Position stand. Exercise and hypertension. Med Sci Sports Exerc. 2004;36:533-553. 2. Asano RY, Sales MM, Coelho JM, de Moraes, JFVN, Pereira LA, Campbell CSG Simões HG. Exercise, nitric oxide, and endothelial dysfunction: A brief review. JEPonline. 2012;15(1).7686. 3. Asano RY, Sales MM, Browne RAV, Moraes JFVN, Coelho Júnior HJC, Moraes MR, Simões HG. Acute effects of physical exercise in type 2 diabetes: A review. World J Diabetes. 2014;5: 659-665. 4. Bentes CM, Costa PB, Neto GR, Costa e Silva GV, Salles BF, Miranda HL, Novaes JS. Hypotensive effects and performance responses between different resistance training intensities and exercise orders in apparently health women. Clin Physiol Funct Imaging. 2014 5. Brown LE, Weir JP, Oliveira HB, Bottaro M, Lima LCJ, Fernandes Filho J. Recomendação de procedimentos da Sociedade Americana de Fisiologia do Exercício. Revista Brasileira Ciência e Movimento. 2003;11:95-110. 6. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, Jones DW, Materson BJ, Oparil S, Wright Jr JT, Roccella EJ. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 Report. JAMA. 2003;289:2560-2572 7. Cornelissen V, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors a meta-analysis of randomized, controlled trials. Hypertension. 2011;58:950-958 8. Cornelissen VA, Smart, NA. Exercise training for blood pressure: A systematic review and meta‐analysis. J Am Heart Assoc. 2013;2(1):e004473. doi: 10.1161/JAHA.112.004473. 9. VI Diretrizes Brasileiras De Hipertensao. Arquivo Brasileiro de Cardiologia. 2010;95:1(supl. 1):1-51. 10. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MR, Lee IM, Swain DP. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med Sci Sports Exerc. 2011; 43(7):1334-1359. 11. Lizardo JHF, Simões HG. Efeitos de diferentes sessões de exercícios resistidos sobre a hipotensão pós-exercício. Revista Brasileira de Fisioterapia. 2005;9:289-295. 12. Macdonald JR. Potential causes, mechanisms, hypotension. J Hum Hypertens. 2002;16:225-236. and implications of post exercise 65 13. Miller RR, Vismara LA, Zelis R, Amsterdam EA, Mason DT. Clinical use of sodium nitroprusside in chronic ischemic heart disease. Effects on peripheral vascular resistance and venous tone and on ventricular volume, pump and mechanical performance. Circulation. 1975;51(2):328-336. 14. Mohebbi H, Rahmaninia F, Sheikholeslami VD, Faraji H. The effects of the intensity and volume of resistance exercises on the post-exercise blood pressure, heart rate and rate pressure product. J Med Sci Islamic Azad University of Mashhad. 2009. 15. Montero-fernández N, Serra-rexach JA. Role of exercise on sarcopenia in the elderly. Eur J Phys Rehabil Med. 2013;49:131-143. 16. Polito MD, Simão R, Senna GW, Farinatti PTV. Efeito hipotensivo do exercício de força realizado em intensidades diferentes e mesmo volume de trabalho. Revista Brasileira de Medicina do Esporte. 2003:9 17. Ratamess NA, Alvar BA, Evetoch TK, Housh TJ, Kibler WB, Kraemer WJ. Progression models in resistance training for healthy adults [ACSM Position Stand]. Med Sci Sports Exerc. 2009:41(3):687-708. 18. Rezk CC, Marrache RCB, Tinucci T, Mion Jr D, Forjaz C. Post-resistance exercise hypotension, hemodynamics, and heart rate variability: Influence of exercise intensity. Eur J Appl Physiol. 2006;98(1):105-112. 19. Stamler JS, Loh E, Roddy MA, Currie KE, Creager MA. Nitric oxide regulates basal systemic and pulmonary vascular resistance in healthy humans. Circulation. 1994:89(5):2035-2040. 20. Stenholm S, Tiainen K, Rantanen T, Sainio P, Heliövaara M, Impivaara O, Koskinen S. Long‐term determinants of muscle strength decline: Prospective evidence from the 22‐year mini‐Finland follow‐up survey. J Am Geriatr Soc. 2012:60(1):77-85. 21. Tirosh A, Afek A, Rudich A, Percik R, Gordon B, Ayalon N, Shai I. Progression of normotensive adolescents to hypertensive adults a study of 26,980 teenagers. Hypertens. 2010:56(2):203-209. Disclaimer The opinions expressed in JEPonline are those of the authors and are not attributable to JEPonline, the editorial staff or ASEP.