Archived Webinar Series from the New England Genetics
advertisement

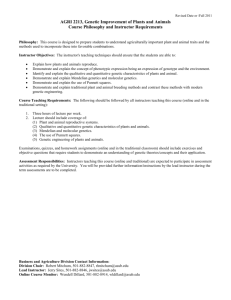
Archived Webinar Series from the New England Genetics Collaborative (NEGC) "It's All About Teamwork: Incorporating Genetics and Family History into the Work of the Patient Centered Medical Home (PCMH)." The NEGC held a webinar series (May-Sept 2015) with the child health improvement partnerships in Maine, New Hampshire, and Vermont to highlight how a team-approach to caring for children with genetic and complex conditions within the Patient Centered Medical Home will improve collaboration, coordination, and satisfaction for families and providers. This series was designed for 1) pediatric and family physicians, 2) clinical teams; and 3) families interested in best practice. We invite you to listen and share these great resources with colleagues! Webinars and handouts are archived here: http://www.negenetics.org/work-groups/medical/medicalhomeactivities. "Effective Care Coordination in the Pediatric Medical Home” with Jeanne McAllister, BSN, MS, MHA an Associate Research Professor of Pediatrics at Indiana University School of Medicine, Children's Health Services Research Division, and Dr. Jill Rinehart, MD of Hagan, Rinehart & Connolly Pediatrics in Burlington, VT. Learning objectives: To understand how and why effective care coordination is essential to improving care Learn why it is important to families, practices and pediatric health care professionals Learn how to implement a system of strengths based, family centered care coordination Example of different stakeholders coming together to support a model for change We asked attendees…what will you do differently after the session? Approach Care Coordination with families as a “new standard of care” Make sure providers working with my clients are up to date with each other Consider implementation of shared care plans with families in my specialty clinic “Care coordination is not for every child every time, but could be for any child at any time.” Jill Rinehart, MD. "Achieving Care Coordination with Shared Plans of Care" with Dr. Jill Rinehart, MD of Hagan, Rinehart & Connolly Pediatrics in Burlington, VT and Jeanne McAllister, BSN, MS, MHA. Associate Research Professor of Pediatrics at Indiana University School of Medicine Learning objectives: Define what a shared plan of care is and what is included in the medical summary. Outline the 10 principles of achieving a shared plan of care. Providing tips on building relationships with specialists to have ongoing and effective communications. We asked attendees…what will you do differently after the session? This gives me a structure to work with to evaluate and enhance our current practices Update care plans to be less medical and more family centered Look at reimbursement codes; push for changes in our EMR "Tips and Tools for Taking an Effective Family Medical and Social History", with Dr. Leah Burke, Director of the Vermont Regional Genetics Center and Dr. Craig Donnelly, Professor of Psychiatry and Pediatrics, Dartmouth-Hitchcock Medical Center Learning objectives: Identify the benefits of taking a family history in the primary care setting Demonstrate how to properly collect and interpret a meaningful family history using the pedigree and other tools Recognize the red flags in family histories in pediatrics We asked attendees…what will you do differently after the session? We are currently working on nursing education related to family history, and the tools in your presentation, especially the “SCREEN” mnemonic and “Rule of Too/Two”, will be very helpful. I have a better understanding of how to do a family assessment; screening will help me better identify outliers; I will take more in-depth psychiatric history. Change the tools I recommend to providers…to the AAP’s “Genetics in Primary Care Institute” and the Genetic Alliance’s “Does It Run In the Family” toolkit “Care coordination is not for every child every time, but could be for any child at any time.” Jill Rinehart, MD. "Incorporating Genetics in the Management of Children in the Primary Care Office" with Dr. Rosemarie Smith and Dr. Wendy Smith, both of Maine Medical Center Pediatric Specialty Care Learning objectives: Using case study, examine clinical situations where genetic testing is indicated o Diagnostic testing o Presymptomatic testing o Medical management Using case study, examine clinical situations where genetic testing is not indicated o Presymptomatic testing o Carrier testing Identify genetic testing resources Review ELSI, consent, financial and insurance issues We asked attendees…what will you do differently after the session? 1. We get asked about screening for "genetic" problems that "run in the family" all the time and this offer a nice strategy for dealing with that. 2. We talk with physicians and medical staff more than with patients/families; this gave me a better perspective on other points of view – PCPs, families dealing with insurance and labeling, etc. 3. Will know to look more carefully at what genetic testing results truly mean for the family About the NEGC: The New England Genetics Collaborative is one of 7 regional organizations across the US dedicated to narrowing the gap between what is and what can be, for individuals with genetic disorders. Funded by HRSA, the NEGC coordinates collaboration among public health, metabolic and genetic clinics, medical homes, academia, and parent groups to support innovation in genetics and improve access to genetic services. This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number 46UMC24093, New England Genetics Collaborative, total award amount $3,000,000 (100% governmental sources). This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government. “Care coordination is not for every child every time, but could be for any child at any time.” Jill Rinehart, MD.