International SCI Pain Extended Data Set
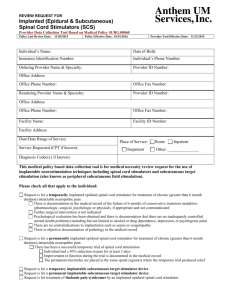
advertisement

The International Spinal Cord Injury Pain Extended Data Set (ISCIPEDS) The working-group consists of: Eva Widerström-Noga, DDS PhD (Chair); Fin Biering-Sørensen, MD, PhD; Thomas N Bryce, MD; Diana D Cardenas, MD, MHA; Nanna Brix Finnerup, MD, PhD; Mark P Jensen, PhD; J Scott Richards, PhD; Elizabeth J Richardson, PhD, MSPH; Philip Siddall, MD, PhD Our interdisciplinary working group consists of members with published research expertise in the area of spinal cord injury (SCI) related pain. The members have expertise with regard to the clinical condition of pain, pain taxonomy, psychophysics of pain, psychology, epidemiology and assessment of pain and represent the Executive Committee of the International Spinal Cord Injury Standards and Data Sets (ASIA/ISCoS; Biering-Sørensen) and major organizations with an interest in SCI-related pain (i.e., the International Spinal Cord Society (ISCoS), American Spinal Injury Association (ASIA), Association of Spinal Cord Injury Professionals (ASCIP), American Pain Society (APS) and International Association for the Study of Pain (IASP)). Most of the committee members have memberships in several of these organizations. Pain after SCI is a significant problem for those who experience it as well as for their healthcare providers because of its persistent nature. Pain in people with SCI is classified in broad categories as nociceptive, neuropathic (at- or below level of injury), other or unknown (Bryce et al., 2012 a,b). Neuropathic pain may be associated with evoked pain, such as allodynia or hyperalgesia (Eide et al., 1996; Finnerup et al., 2001). The neuropathic pains are rarely completely eliminated by available treatment interventions but can be meaningfully reduced in some people (Siddall et al., 2006; Cardenas et al., 2013). Because of the persistent nature of pain associated with SCI, there is a need to understand and assess both pain and associated psychological factors. The clinical presentation of pain after SCI often includes multiple concomitant pain problems that are superimposed upon various physical impairments and consequences of injury. This presents unique challenges in the assessment of both pain and associated psychosocial factors and ultimately for clinical management. The overall purpose of the International Spinal Cord Injury Pain Data Sets (ISCIPDS) is to standardize the collection and reporting of pain in the SCI population. The ISCIPDS contains a basic (ISCIPBDS) and an extended (ISCIPEDS) data set. The ISCIPBDS contains a minimal amount of clinically relevant information concerning pain that can be collected in the daily practice of healthcare professionals with expertise in SCI. The first version of the International Spinal Cord Injury Pain Basic Data Set ISCIPBDS was published in 2008 (Widerstrom-Noga et al., 2008) and a revised version ISCIPBDS v2.0 (Widerstrom-Noga et al., 2014) in 2014. The revised version was shortened to increase its clinical utility and to reflect the new SCI pain taxonomy (Bryce et al., 2012 a,b). It is adopted by the National Institute of Health, National Institute of Neurological Disorders and Stroke (NINDS), Common Data Elements (CDEs) as a supplemental/highly recommended dataset to be collected in clinical SCI pain research (www.commondataelements.ninds.nih.gov/SCI.aspx#tab=Data_Standards) (Jakeman et al., in press) The ISCIPEDS is directly based on the pain problems identified in the ISCPBDS and is primarily intended to provide guidance regarding the assessment of pain, and associated sensory function and psychosocial factors in clinical pain studies and trials. Consistent evaluation of these factors will facilitate research collaboration between clinical centers and thus expedite the development of beneficial treatments. The use of comparable sets of outcome measures in research studies will increase efficiency and facilitate collaborations, translation, interpretation, and application of results. The ISCIPEDS is intended to be collected by researchers or healthcare professionals involved in research studies and who are familiar with SCI. Data should be collected by interview (dependent on the recommended mode of administration for a specific instrument) and examination. The ISCIPEDS includes several important assessment components divided in 4 sections: (1) Pain symptom assessment including individual variables related to the temporal course, severity, unpleasantness, tolerability of pain, as well as questionnaires related to the pain type and symptom severity. This section is divided into: A. Overall pain (assessments are intended to provide an overall assessment of all pain that a person may experience). B. Each pain problem (assessments are intended to be performed for each separate pain problem identified in the ISCIPBDS); and C. Recommended questionnaires intended to provide supplemental information as appropriate for a specific purpose or interest. (2) Sensory assessment to detect and quantify common sensory abnormalities, including light touch, pinprick, and cold sensation in a neuropathic pain area; (3) Treatments used in the past 12 months and for ongoing treatments, dose (if appropriate), frequency of treatment, any adverse effects, and a rating of global impression of change; and (4) Psychosocial domains and comorbid conditions including outcomes, mediating factors, or comorbid conditions (e.g., depression, anxiety, quality of life). Forms for all assessment variables except for questionnaires can be found in the Appendix. Pain symptoms and signs are particularly important to evaluate in populations, such as SCI, where pain is typically heterogeneous, persistent and often severe. Symptoms and signs associated with neuropathic pain may not only facilitate a better understanding of the clinical condition but may also provide a foundation for subgroup analyses in clinical trials and thus facilitate future mechanismsbased treatment interventions (Baron et al., 2012; Demant et al., 2014 ). The pain symptom measures included in the ISCIPEDS are intended to be simple, and clinically useful. They are divided into measures that can be used to assess overall pain and measures that are more useful if asked for a specific pain problem. There is also a section of recommended pain questionnaires that assess the presence and severity of pain symptoms and have data supporting their utility after SCI. These measures are intended to provide supplemental information as appropriate for a specific purpose or interest. The sensory measures are intended to detect and quantify common sensory abnormalities, including mechanical allodynia, mechanical hyperalgesia, and thermal allodynia commonly associated with neuropathic pain types. Information regarding a persons’ previous and current experience with various treatment interventions is important both for the planning of clinical studies and facilitates screening of potential participants of a clinical trial. The ISCIPEDS is designed to capture information regarding both past (last 12 months) and current treatments. Due to possible recall biases, the effectiveness of past treatments are not captured in detail but only whether a person has had the treatment in the past 12 months and if it was helpful or not, or unknown. For current, ongoing treatments, more details are captured, including the dose (if appropriate), frequency of treatment, any adverse effects, and a rating of global impression of change (Guy 1976). The psychosocial domains that researchers should consider assessing in their studies of SCI pain include outcome variables, mediating variables and comorbid conditions that would be of interest to those seeking to develop, test, or expand biopsychosocial models of SCI-related pain. The ISCIPEDS working group selected those domains, and identified potential measures of those domains, as a function of (a) their relevance to individuals with SCI and chronic pain and (b) the existence of published findings that support the validity of the measures selected in samples of individuals with SCI, and as much as possible (c) their availability in the public domain. There is a vast array of outcomes measures that have been recommended for use in neuropathic pain research (Haanpӓӓ et al., 2011) and in SCI pain research specifically (Bryce et al., 2007). Reviewing all such measures is beyond the scope of the ISCIPEDS. We recommend that researchers carefully examine the appropriateness of any measure they might like to use with respect to utility in the SCI chronic pain population. For example, standard measures for pain-related outcomes may have content that is inappropriate for persons with SCI, or that can be misleading if endorsed (e.g., unusual sensory experiences). The instruments in the ISCIPEDS were selected in part to minimize that problem. The reader is also referred to the SCIRE (www.scireproject.com) and NINDS CDEs (www.commondataelements.ninds.nih.gov/SCI.aspx) websites where an extensive number of outcome measures are evaluated with respect to their applicability and psychometric properties. While the measures reviewed in these loci are not focused only on pain per se, they offer other resources for SCI researchers who want to use the most valid scales, particularly those which are being proposed for adoption across studies. Acknowledgements: We thank William Bauman, Susan Charlifue, and Vanessa Noonan for valuable comments and suggestions. 1. PAIN SYMPTOM ASSESSMENT: A. Overall pain (assessment includes all pain problems but could also be assessed for each pain problem (previously identified by the ISCIPBDS) if appropriate). __________________________________________________________________________________ VARIABLE NAME: Number of days with pain in the last 7 days including today DESCRIPTION: This variable specifies the total number of days with pain during the last 7 days, including today. CODES: 0 – none 1 – one day 2 – two days 3 – three days 4 – four days 5 – five days 6 – six days 7 – seven days Unknown “Today” is the day the individual answers the question regardless time of day. The duration of pain during the day does not matter in answering this question. __________________________________________________________________________________ COMMENTS: VARIABLE NAME: Average pain intensity of the worst pain in the last week DESCRIPTION: A 0 – 10 Numerical Rating Scale (ranging from 0 = “No pain” to a maximum of 10 = “The most intense pain imaginable”) of average pain intensity for the worst pain problem the respondents experience). Please note that “last week” specifically refers to the last seven days including today. CODES: 0, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 COMMENTS: Pain intensity is the most common pain domain assessed in research and clinical settings. Although different rating scales have proven to be valid for assessing pain intensity, including the Numerical Rating Scale (NRS), the Verbal Rating Scale (VRS), and the Visual Analogue Scale (VAS), the 0 – 10 NRS has the most strengths and fewest weaknesses of available measures (Jensen & Karoly, 2000). Moreover the 0 – 10 NRS has been recommended by the IMMPACT consensus group for use in pain clinical trials (Dworkin et al., 2005) and by the 2006 NIDRR SCI Pain outcome measures consensus group (Bryce et al., 2007). The seven day time frame was selected to balance the need to assess pain over a long enough epoch to capture usual pain, against the need to keep the time frame short enough to maximize recall accuracy. The instruction and endpoints used were designed to differentiate between pain intensity and pain unpleasantness (Dannecker et al., 2007). For example, the intensity of pain is how strong the pain feels and the unpleasantness of pain is how disturbing the pain is. In order to better understand the difference between pain intensity and unpleasantness one can substitute the word “sound” for “pain”. Pain intensity is analogous to the loudness of a sound while unpleasantness is analogous to the aversiveness of a sound not necessarily related to its loudness. __________________________________________________________________________________ VARIABLE NAME: Average pain unpleasantness in the last week DESCRIPTION: A 0 – 10 Numerical Rating Scale (ranging from 0 = “Not at all unpleasant” to a maximum of 10 = “The most unpleasant pain imaginable”) of average pain unpleasantness for (up to) three pain problems (the three worst pain problems respondents experience). Please note that “last week” specifically refers to the last seven days including today. CODES: 0, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 COMMENTS: Pain is a result of sensory, cognitive, and affective dimensions, and the emotional dimension can be evaluated separately from intensity (Price et al., 1987). Although different rating scales have proven to be valid for assessing pain intensity, including the Numerical Rating Scale (NRS), the Verbal Rating Scale (VRS), and the Visual Analogue Scale (VAS), the 0 – 10 NRS has the most strengths and fewest weaknesses of available measures (Jensen & Karoly, 2000). The instruction and endpoints used were designed to differentiate between pain intensity and pain unpleasantness (Dannecker et al., 2007). For example, the intensity of pain is how strong the pain feels and the unpleasantness of pain is how disturbing the pain is. In order to better understand the difference between pain intensity and unpleasantness one can substitute the word “sound” for “pain”. Pain intensity is analogous to the loudness of a sound while unpleasantness is analogous to the aversiveness of a sound not necessarily related to its loudness. __________________________________________________________________________________ VARIABLE NAME: Number of days with manageable/tolerable pain in the last 7 days including today DESCRIPTION: This variable specifies the total number of days with pain during the last 7 days, including today. CODES: 0 – none 1 – one day 2 – two days 3 – three days 4 – four days 5 – five days 6 – six days 7 – seven days Unknown COMMENTS: “Today” is the day the individual answers the question regardless time of day. The duration of manageable/tolerable pain during the day does not matter in answering this question. Manageable or tolerable pain is a construct reported by Zelman et al., 2004, and not specific to pain after SCI. Focus group methodology has suggested that manageable or tolerable pain is pain that permits concentration on something other than the pain, perhaps by using a treatment or self-remedy that “takes the edge off” pain and allows performance of daily activities or “getting something done.” Other factors associated with manageable pain are lower levels of negative mood, feeling well enough to socialize and not experiencing excessive adverse effects of ongoing treatments including medication. __________________________________________________________________________________ B. Each pain problem (to be assessed for each pain problem previously identified by the ISCIBPDS) __________________________________________________________________________________ VARIABLE NAME: Pain intensity in present moment DESCRIPTION: A 0 – 10 Numerical Rating Scale (ranging from 0 = “No pain” to a maximum of 10 = “The most intense pain imaginable”) of present pain intensity for (up to) three pain problems (the three worst pain problems respondents experience). Please note that “present” specifically refers to this moment. CODES: 0, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 COMMENTS: Pain intensity is the most common pain domain assessed in research and clinical settings. Although different rating scales have proven to be valid for assessing pain intensity, including the Numerical Rating Scale (NRS), the Verbal Rating Scale (VRS), and the Visual Analogue Scale (VAS), the 0 – 10 NRS has the most strengths and fewest weaknesses of available measures (Jensen & Karoly, 2000). Moreover the 0 – 10 NRS has been recommended by the IMMPACT consensus group for use in pain clinical trials (Dworkin et al., 2005) and by the 2006 NIDRR SCI Pain outcome measures consensus group (Bryce et al., 2007). __________________________________________________________________________________ VARIABLE NAME: How long does your pain usually last? DESCRIPTION: This variable provides an estimate of the duration of pain. Some pain types are very brief and may be felt several times per day. This question refers to the duration of each separate pain event. CODES: One minute or less More than one minute but less than one hour At least one hour, but less than 24 hours At least 24 hours but not continuous Constant or continuous Unknown COMMENTS: The duration of pain can be defined when a specific pain follows a predictable pattern. If no predictable pattern for a specific pain exists, the answer “unknown” is given. VARIABLE NAME: When during the day is the pain most intense? DESCRIPTION: This variable identifies the diurnal peak in pain intensity. CODES: Morning Afternoon Evening Night Unpredictable; pain is not consistently more intense at any one time of day “Morning” is between 6.01 am and 12.00 am (06.01 and 12.00); “Afternoon” is between 12.01 am and 6.00 pm (12.01 and 18.00); “Evening” is between 6.01 pm and 12.00 pm (18.01 and 24.00); “Night” is between 0.01am and 6.00 am (00.01 and 06.00) __________________________________________________________________________________ COMMENTS: C. Recommended questionnaires Instruments for the assessment of pain type or pain symptom severity are listed in Table 1. Nociceptive pain assessment The assessment for nociceptive pain will be assessed as in non-SCI populations. __________________________________________________________________________________ 2. SENSORY ASSESSMENT ______________________________________________________________________________ VARIABLE NAME: Dynamic light touch DESCRIPTION: Sensation rated as normal (compared to a control area in a non-affected skin area), absent (no sensation felt), hypoesthesia (decreased sensation compared to control area), hyperesthesia (increased sensation compared to control area), allodynia (the touch provokes pain), other (changed sensation that cannot be categorized otherwise). If allodynia is present the pain is rated on a 0 – 10 Numerical Rating Scale (ranging from 0 = “No pain” to a maximum of 10 = “Pain as bad as you can imagine”). COMMENTS: Can be assessed by light stroking the skin with an innocuous moving stimuli, e.g. a cotton wisp, cotton wool tip, or a brush (e.g. Somedic standardized brush, Sweden) of approximately 2 cm with a speed of 1-2 cm/sec. (Rolke et al. 2006). __________________________________________________________________________________ VARIABLE NAME: Pinprick DESCRIPTION: Sensation rated as normal (compared to a control area in a non-affected skin area), absent (no sensation felt), hypoalgesia (decreased pain sensation compared to control area), hyperalgesia (increased pain sensation compared to control area), other (changed sensation that cannot be categorized otherwise). If hyperalgesia is present the pain is rated on a 0 – 10 Numerical Rating Scale (ranging from 0 = “No pain” to a maximum of 10 = “Pain as bad as you can imagine”). COMMENTS: Can be assessed using a disposable safety pin or calibrated monofilaments (Rolke et al., 2006) __________________________________________________________________________________ VARIABLE NAME: Cold DESCRIPTION: Sensation rated as normal (compared to a control area in a non-affected skin area), absent (no sensation felt), hypoesthesia (decreased sensation compared to control area), hyperesthesia (increased sensation compared to control area), allodynia (the cold provokes pain), other (changed sensation that cannot be categorized otherwise). If allodynia is present the pain is rated on a 0 – 10 Numerical Rating Scale (ranging from 0 = “No pain” to a maximum of 10 = “Pain as bad as you can imagine”). COMMENTS: Can be assessed using a cold thermoroll (Somedic Sweden) of 20 or 25C, a piece of cold metal, an ice cube or an acetone droplet. For determination of cold detection and cold pain thresholds, thermal tests can be performed using thermo testers (TSA, Medoc, Israel or MSA, Somedic, Sweden) (Rolke et al. 2006). __________________________________________________________________________________ 3. TREATMENTS __________________________________________________________________________________ VARIABLE NAME: Past treatment DESCRIPTION: This variable specifies treatments for pain received in the past and treatment response. Person to indicate (“Check”) each treatment that they have received in the past for their pain. Where possible, the person also indicates whether it was helpful (“Yes”) or not helpful (“No”). If the person, cannot remember or is uncertain about effectiveness they indicate “Uncertain”. The section can be completed to indicate treatments and response for all types of pain overall or multiple forms for specific pain types. Due to the fact that the management of pain in SCI is challenging with a wide range of treatments being tried, including pain medications, such as opioids, non-steroidal anti-inflammatory drugs, acetaminophen, tricyclic antidepressants and anticonvulsants, as well as physical therapy and alternative treatment approaches, such as massage, marijuana, acupuncture and hypnosis (Cardenas and Jensen 2006, Murphy and Reid 2001, Norrbrink Budh and Lundeberg 2004), self-management (Umlauf 1992), as well as relaxation and psychotherapy, procedural and surgical interventions the list provided is very long to cover most possibilities. __________________________________________________________________________________ COMMENTS: VARIABLE NAME: Current treatment DESCRIPTION: This variable specifies the current treatments for pain, timing of treatment, response and side effects. COMMENTS: Person to indicate current treatments for pain, including dose (“Dose”) (if medication) and frequency (“How often”). Effectiveness is assessed using the Patient Global Impression of Change (“PGIC”); (Guy, 1976, Bryce et al., 2007). Any side effects or adverse events (“Side effects/adverse events”) related to the treatment are also to be noted. The section can be completed to indicate treatments and response for all types of pain overall or multiple forms for specific pain types. __________________________________________________________________________________ 4. PSYCHSOCIAL AND COMORBID CONDITIONS A number of psychometric instruments are available for assessing pain relevant domains and these are listed in Table 2. __________________________________________________________________________________ Reference list Amtmann D, Cook KF, Johnson KL, Cella D. (2011). The PROMIS initiative: involvement of rehabilitation stakeholders in development and examples of applications in rehabilitation research. Arch Phys Med Rehabil 92(10 Suppl): S12-9. PMID: 21958918. Amtmann D, Kim J, Chung H, Bamer AM, Askew RL, Wu S, Cook KF, Johnson KL. (2014). Comparing CESD-10, PHQ-9, and PROMIS depression instruments in individuals with multiple sclerosis. Rehabil Psychol 59(2): 220-9. PMID: 24661030. Baron, R., Förster, M., Binder, A. Subgrouping of patients with neuropathic pain according to painrelated sensory abnormalities: a first step to a stratified treatment approach. Lancet Neurol 2012; 11(11): 999-1005. Bouhassira D, Attal N, Fermanian J, Alchaar H, Gautron M, Masquelier E, Rostaing S, Lanteri-Minet M, Collin E, Grisart J, Boureau F. (2004). Development and validation of the Neuropathic Pain Symptom Inventory. Pain 108(3): 248-57. PMID: 15030944. Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, Cunin G, Fermanian J, Ginies P, Grun-Overdyking A, Jafari-Schluep H, Lantéri-Minet M, Laurent B, Mick G, Serrie A, Valade D, Vicaut E. (2005). Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 114(1-2): 29-36. PMID: 15733628. Bryce TN, Budh CN, Cardenas DD, Dijkers M, Felix ER, Finnerup NB, Kennedy P, Lundeberg T, Richards JS, Rintala DH, Siddall P, Widerström-Noga E. (2007). Pain after spinal cord injury: an evidence-based review for clinical practice and research. Report of the National Institute on Disability and Rehabilitation Research Spinal Cord Injury Measures meeting. J Spinal Cord Med 30(5): 421-40. PMID: 18092558. Bryce TN, Biering-Sørensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T, Norrbrink C, Richards JS, Siddall P, Stripling T, Treede RD, Waxman SG, Widerström-Noga E, Yezierski RP, Dijkers M. (2012a). International spinal cord injury pain classification: part 1. background and description. Spinal Cord 50(6):413-7. PMID: 22182852. Bryce TN, Biering-Sørensen F, Finnerup NB, Cardenas DD, Defrin R, Ivan E, Lundeberg T, Norrbrink C, Richards JS, Siddall P, Stripling T, Treede RD, Waxman SG, Widerström-Noga E, Yezierski RP, Dijkers M. (2012b). International Spinal Cord Injury Pain (ISCIP) Classification: part 2. initial validation using vignettes. Spinal Cord 50(6): 404-12. PMID: 22310319. Bryce TN, Richards JS, Bombardier CH, Dijkers MP, Fann JR, Brooks L, Chiodo A, Tate DG, Forchheimer M. (2014). Screening for neuropathic pain after spinal cord injury with the spinal cord injury pain instrument (SCIPI): a preliminary validation study. Spinal Cord 52(5): 407-12. PMID: 24614856. Cardenas DD, Jensen MP. (2006). Treatments for chronic pain in persons with spinal cord injury: a survey study. J Spinal Cord Med 29(2): 109-17. PMID: 16739554. Cardenas DD, Nieshoff EC, Suda K, Goto S, Sanin L, Kaneko T, Sporn J, Parsons B, Soulsby M, Yang R, Whalen E, Scavone JM, Suzuki MM, Knapp LE. (2013). A randomized trial of pregabalin in patients with neuropathic pain due to spinal cord injury. Neurology 80(6): 533-9. PMID: 23345639. Charlifue S, Post MW, Biering-Sørensen F, Catz A, Dijkers M, Geyh S, Horsewell J, Noonan V, Noreau L, Tate D, Sinnott KA. (2012). International Spinal Cord Injury Quality of Life Basic Data Set. Spinal Cord 50(9): 672-5. PMID: 22450884. Connor KM, Davidson JRT. (2003). Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress and Anxiety 18(2): 76-82. PMID: 12964174. Dannecker EA, George SZ, Robinson ME. Influence and stability of pain scale anchors for an investigation of cold pressor pain tolerance. J Pain. 2007 Jun;8(6):476-82. Demant, D.T., Lund, K., Vollert, J., Maier, C., Segerdahl, M., Finnerup, N.B., Jensen, T.S., Sindrup, S.H. The effect of oxcarbazepine in peripheral neuropathic pain depends on pain phenotype: a randomised, double-blind, placebo-controlled phenotype-stratified study. Pain 2014; 155(11): 221517. Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, Carr DB, Chandler J, Cowan P, Dionne R, Galer BS, Hertz S, Jadad AR, Kramer LD, Manning DC, Martin S, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robbins W, Robinson JP, Rothman M, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Wernicke J, Witter J; IMMPACT. (2005). Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 113(1-2): 9-19. PMID: 15621359. Dworkin RH, Turk DC, Revicki DA, Harding G, Coyne KS, Peirce-Sandner S, Bhagwat D, Everton D, Burke LB, Cowan P, Farrar JT, Hertz S, Max MB, Rappaport BA, Melzack R. (2009). Development and initial validation of an expanded and revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2). Pain 144(1-2): 35-42. PMID: 19356853. Eide PK, Jørum E, Stenehjem AE. (1996). Somatosensory findings in patients with spinal cord injury and central dysaesthesia pain. J Neurol Neurosurg Psychiatry. 60(4): 411-5. PMID: 8774406. Finnerup NB, Johannesen IL, Sindrup SH, Bach FW, Jensen TS. (2001). Pain and dysesthesia in patients with spinal cord injury: a postal survey. Spinal Cord 39(5): 256-62. PMID: 11438841. EuroQol Group. (1990). EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 16(3): 199-208. PMID: 10109801. Freynhagen R, Baron R, Gockel U, Tölle TR. (2006). painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin 22(10): 1911-1920. PMID: 17022849. Guy W. ECDEU Assessment manual for psychopharmacology, Revised 1976. US Government Printing Office; 1976. Rockville, MD. Haanpää M, Attal N, Backonja M, Baron R, Bennett M, Bouhassira D, Cruccu G, Hansson P, Haythornthwaite JA, Iannetti GD, Jensen TS, Kauppila T, Nurmikko TJ, Rice AS, Rowbotham M, Serra J, Sommer C, Smith BH, Treede RD. NeuPSIG guidelines on neuropathic pain assessment. Pain. 2011 Jan;152(1):14-27. Biering-Sørensen F, Ala'i S, Anderson K, Charlifue S, Chen Y, DeVivo M, Flanders A, Jones L, Kleitman N, Lans A, Noonan V, Odenkirchen J, Steeves J, Tansey K, Widerström-Noga E. Jakeman L.Common Data Elements for Spinal Cord Injury Clinical Research: a National Institute for Neurological Disorders and Stroke Project (in revision for Spinal Cord). Jensen MP, Karoly P. (2000). Self-report scales and procedures for assessing pain in adults, In: Handbook of pain assessment (2nd Edition), Guilford Press, New York. Jensen MP, Gammaitoni AR, Olaleye DO, Oleka N, Nalamachu SR, Galer BS. (2006). The pain quality assessment scale: assessment of pain quality in carpal tunnel syndrome. J Pain 7(11): 823-32. PMID: 17074624. Krause SJ, Backonja MM. (2003). Development of a neuropathic pain questionnaire. Clin J Pain 19(5): 306-14. PMID: 12966256. Kronke K, Spitzer RL, Williams JB. (2003). The Patient Health Questionnaire-2: validity of a twoitem depression screener. Med Care 41(11): 1284-92. PMID: 14583691. May LA, Warren S. (2001). Measuring quality of life of persons with spinal cord injury: substantive and structural validation. Qual Life Res 10(6): 503-515. PMID: 11789551. May LA , Warren S. (2002). Measuring quality of life of persons with spinal cord injury: external and structural validity. Spinal Cord 40(7): 341-350. PMID: 12080462. Miller R, Kori S, Todd D. Tampa Scale of Kinesiophobia (TSK). (1991). Unpublished report. Murphy D, Reid DB. (2001). Pain treatment satisfaction in spinal cord injury. Spinal Cord 39(1): 446. PMID: 11224014. Norrbrink Budh C, Lundeberg T. (2004). Non-pharmacological pain-relieving therapies in individuals with spinal cord injury: a patient perspective. Complement Ther Med 12(4):189-97. PMID: 15649832. Price DD, Harkins SW, Baker C. (1987). Sensory-affective relationships among different types of clinical and experimental pain. Pain 28(3): 297-307. PMID: 2952934. Rolke R, Baron R, Maier C, Tölle TR, Treede RD, Beyer A, Binder A, Birbaumer N, Birklein F, Bötefür IC, Braune S, Flor H, Huge V, Klug R, Landwehrmeyer GB, Magerl W, Maihöfner C, Rolko C, Schaub C, Scherens A, Sprenger T, Valet M, Wasserka B. (2006). Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain 123(3): 231-43. PMID: 16697110. Siddall PJ, Cousins MJ, Otte A, Griesing T, Chambers R, Murphy TK. (2006). Pregabalin in central neuropathic pain associated with spinal cord injury: a placebo-controlled trial. Neurology 67(10): 1792-800. PMID: 17130411. Spitzer RL, Kroenke K, Williams JB. (1999). Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. Spitzer RL, Kroenke K, Williams JB, Löwe B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166(10):1092-7. PMID: 16717171. Umlauf RL. (1992). Psychological interventions for chronic pain following spinal cord injury. Clin J Pain 8(2): 111-8. PMID: 1633374. Zelman DC, Smith MY, Hoffman D, et al. Acceptable, manageable, and tolerable days: patient daily goals for medication management of persistent pain. Journal of pain and symptom management 2004;28:474-87; Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. (1995). Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 62(3): 363-72. PMID: 8657437. Ware JE, Snow KK, Kosinski M, Gandek B. (1993). SF-36® Health Survey Manual and Interpretation Guide. Boston, MA: New England Medical Center, The Health Institute. Watson D, Clark LA, Tellegen A. (1998). Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 54(6):1063-70. PMID: 3397865. Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov. Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN. (1992). Quantifying handicap: a new measure of long-term rehabilitation outcomes. Arch Phys Med Rehabil 73(6): 51926. PMID: 1622299. Widerström-Noga E, Biering-Sørensen F, Bryce T, Cardenas DD, Finnerup NB, Jensen MP, Richards JS, Siddall PJ. (2008). The international spinal cord injury pain basic data set. Spinal Cord 46(12): 818-23. PMID: 18521092. Widerström-Noga E, Biering-Sørensen F, Bryce TN, Cardenas DD, Finnerup NB, Jensen MP, Richards JS, Siddall PJ. (2014).The International Spinal Cord Injury Pain Basic Data Set (version 2.0). Spinal Cord 52(4): 282-6. PMID: 24469147. Table 1. Instruments for determining pain type and/or pain symptom severity. Domain Instrument Pain Type (screening onlynot for individual assessment) Douleur Neuropathique 4 questions (DN4) Pain Quality Construct Measured Neuropathic pain type Intended Population General Mode of Length administration Self or 7 items for Examiner Self; 10 items for Examiner References Spinal Cord Injury Pain Instrument (SCIPI) Pain Quality Assessment Scale (PQAS) Neuropathic pain type SCI Self or Examiner 4 or 7 items Bryce et al., 2014 Pain symptom severity General Self 20 items Jensen et al. (2006) Short form McGill Pain Questionnaire 2 (SF-MPQ-2) Pain symptom severity General Self 22 items Dworkin et al. (2009) Neuropathic Pain Symptom Inventory (NPSI) Pain symptom severity Neuropathic pain Self 12 items Bouhassira et al. (2004) Bouhassira, et al. (2005); Hallstrom, et al. (2011). Availability Free for non-funded academic users . Visit www.proqolid.org/instrum ents/neuropathic_pain_4_q uestions_dn4 Free for use. Can be accessed in the appendix of article by Bryce et al., 2014. Free for non-funded academic users . Visit www.proqolid.org/instrum ents/pain_quality_assessm ent_scale_and_revised_pai n_quality_assessment_scal e_pqas_and_pqas_r Free for academic users if used in studies not funded by commercial companies. Visit www.proqolid.org/instrum ents/short_form_mcgill_pa in_questionnaire_sf_mpq_ 2?fromSearch=yes&text=y es. Copyright. Free for nonfunded academic users. Visit www.proqolid.org/instrum ents/neuropathic_pain_sym ptom_inventory_npsi Neuropathic Pain Questionnaire (NPQ) Pain symptom severity Neuropathic pain Self 12 items Krause and Backonja (2003) PainDETECT (PD-Q) Pain symptom severity Neuropathic pain Self 10 items Freynhagen et al. (2006) Free for use. Can be accessed in the appendix of article by Krause and Backonja, 2003. Copyright. Free. See www.pfizerpatientreported outcomes.com/therapeuticareas/pain/neuropathicpain Table 2. Psychosocial instruments available for assessing pain relevant domains. Domain Depression Anxiety Instrument Patient Health Questionnaire-9 (PHQ-9) Construct Measured Depression symptoms Intended Population Primary care; core measure in SCI model system General Mode of Length administration Self 9 items; 8-item and 2-item versions available Self 8 items References Availability Spitzer et al., 1999; Kroenke et al., 2003. Free via Pfizer www.phqscreeners.c om/ Amtmann et al., 2011; Amtmann et al., 2014. Free via Assessment Center. Visit www.assessmentcent er.net to complete a request for online pdf versions of available instruments. Free via Pfizer www.phqscreeners.c om/ PROMIS Depression Short Form Depression; minimizes somatic confounds Generalized Anxiety Disorder-7 (GAD-7) PROMIS Anxiety - Short Form Anxiety symptoms Primary care Self 7 items Spitzer et al., 2006. Anxiety symptoms General Self 8 items Amtmann et al., 2011. Tampa Scale of Kinesiophobia (TSK) Fear of pain/re-injury Developed for low back pain; used across chronic pain populations Self 17 items Miller et al., 1991; Vlaeyen et al., 1995. Free via Assessment Center. Visit www.assessmentcent er.net to complete a request for online pdf versions of available instruments. Items can be found in the article by Vlaeyen et al. Quality of Life/ Satisfaction with Life PTSD Checklist – Civilian Version (PCL-C) PTSD symptoms General Self 20 items Weathers et al., 2013. To obtain this scale, visit the VA National Center for PTSD website to complete the online request form:www.ptsd.va.g ov/professional/asses sment/adult-sr/ptsdchecklist.asp Short-Form-36 (SF-36) Perceived functional health and well-being Healthrelated quality of life General medical Self or Examiner 36 items; 8 sub-scales Ware et al., 1993. To obtain licensing, visit: www.sf-36.org General medical Self 5 items EuroQol Group, 1990. Satisfaction and quality of life Spinal cord injury Self or Examiner 37 items May & Warren, 2001; May & Warren 2002. General quality of life; satisfaction with physical and mental health Psychologica l resilience Spinal cord injury Self 3 Charlifue et al., 2012. To register study and submit licensing fees (if applicable): www.euroqol.org For direct access: www.uic.edu/orgs/ql i/questionaires/questi onnairehome.htm Items can be found in the Charlifue et al. article. General Self 25 items; 10item, 2-item versions available Connor & Davidson, 2003. EuroQoL-5 Dimension Questionnaire (EQ-5D) Quality of Life Index (QLI) SCI version International SCI Basic Data Set QoL items Resilience Connor Davidson Resilience Scale (CD-RISC) To obtain any version of the scale, a request form can be found at: www.cdrisc.com/ Mood Positive and Negative Affect Schedule (PANAS)7 positive and negative affect General Self 20 items Watson et al., 1998. Can be accessed in the appendix of the original article by Watson et al. Participation Craig Handicap Assessment and Reporting Technique (CHART) – SF Community integration and independence Variety of physical rehabilitation populations Self or Examiner 19 items for CHART-SF Whiteneck et al., 1992. Available via Craig Hospital website: www.craighospital.o rg/repository/docume nts/Research%20Inst ruments/CHART%2 0Manual.pdf Appendix 1. PAIN SYMPTOM ASSESSMENT A. Overall pain Number of days with pain in the last 7 days including today: none; 1; 2; 3; 4; 5; 6; 7; unknown Average pain intensity of the worst pain last week: 0 = no pain; 10 = the most intense pain imaginable: 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10 Average pain unpleasantness in the last week 0 = not at all unpleasant; 10 = the most unpleasant pain imaginable 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10 Number of days with manageable/tolerable pain in the last 7 days including today none; 1; 2; 3; 4; 5; 6; 7; unknown B. Each pain problem Pain intensity in present moment 0 = no pain; 10 = the most intense pain imaginable: 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10 How long does your pain usually last? ≤ 1 min; > 1 min but < 1 hr; ≥ 1 hr but < 24 hrs; ≥ 24 hrs; constant or continuous; unknown When during the day is the pain most intense? -12.00); - - 06.00) (pain is not consistently more intense at any one time of day) - 2. SENSORY ASSESSMENT A. Dynamic light touch At level of injury Normal Absent Hypoesthesia Hyperesthesia Allodynia Other _________ If allodynia, rate the intensity: 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10 Below level of injury Normal Absent Hypoesthesia Hyperesthesia Allodynia Other _________ If allodynia, rate the intensity: 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10 Notes: Left or right side can be noted here B. Pinprick At level of injury Normal Absent Hypoalgesia Hyperalgesia Other _________ If hyperalgesia, rate the intensity: 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10 Below level of injury Normal Absent Hypoalgesia Hyperalgesia Other _________ If hyperalgesia, rate the intensity: 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10 Notes: Left or right side can be noted here C. Cold (Thermoroller, Acetone, Termotester) At level of injury Normal Absent Hypoesthesia Hyperesthesia Allodynia Other _________ If allodynia, rate the intensity: 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10 Below level of injury Normal Absent Hypoesthesia Hyperesthesia Allodynia Other _________ If allodynia, rate the intensity: 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10 Notes: Left or right side can be noted here 3. TREATMENTS A. Past treatments This section can either be filled out for overall pain or for each separate pain component. Please indicate previous treatments (over the last 12 months) and whether the treatment was helpful. Please indicate all treatments you have had (over the last 12 months) Was the treatment helpful? Check Yes Physiotherapy Aerobic exercise (low to moderate intensity) Passive exercise (non-weight bearing or against resistance, e.g., stretching) Resistance exercise (strength building, e.g., weight training) Position adjustment (in wheelchair, bed, etc.) Joint mobilisation/manipulation (incl. chiropractic, osteopathic) Other, specify Passive and stimulation therapy Massage Acupressure Transcutaneous electrical nerve stimulation (TES, TNS, TENS) Ultrasound Laser Heat therapy (incl. heat-packs, shortwave) Other, specify Relaxation and Psychotherapy Bio-feedback/relaxation training Relaxation (relaxation techniques, e.g., muscle relaxation or deep breathing) Meditation (meditation techniques, e.g., concentrative, religious) Mindfulness meditation (meditation using mindfulness technique) Hypnosis Cognitive/Behavioural therapy Other psychotherapy Other, specify Oral and topical medication Antidepressants (e.g., amitriptyline, nortriptyline, duloxetine) Antiepileptics (e.g., pregabalin, gabapentin, carbamazepine) Tramadol Opioids (e.g., morphine, oxycodone, buprenorphine, fentanyl) Cannabinoids (e.g., marijuana) Acetaminophen/paracetamol NSAIDs/aspirin e.g., ibuprofen, naproxen, celecoxib, meloxicam Benzodiazepines e.g., diazepam No Uncertain/ Unknown Antispasticity drugs e.g., baclofen, tizantidine Topical anaesthetics e.g., lidocaine/lignocaine Topical capsaicin Other, specify Procedural interventions Trigger point injection/Dry needling Acupuncture Peripheral nerve/motor point block (incl. alcohol, phenol, steroid, anaesthetic blocks, botulinum toxin injection) Joint injections (incl. shoulder, knee, facet joint, ilio-sacral) Intravenous lidocaine Intravenous ketamine Epidural block Intrathecal pumps (incl. morphine, ziconotide, clonidine, baclofen) Spinal cord stimulator Transcranial brain stimulation (tDCS or rTMS) Other, specify Surgical interventions Dorsal root entry zone lesion Spinal surgery (incl. stabilization, rod removal, untethering the cord, shunt) Deep brain stimulation (implanted brain electrodes) Other, specify Other treatments Specify B. Current treatments For examples of treatments please see previous scetion (A. Past treatments) Treatment Dose How often PGIC* Side effects/adverse events *PGIC - Patient Global Impression of Change Indicate the effect of the treatment on your global wellbeing using one of the following descriptors: Very much improved (1) – Much improved (2) – Minimally improved (3) – No change (4) – Minimally worse (5) – Much worse (6) – Very much worse (7)