Format for Clinical Trial Protocol
advertisement

CLINICAL TRIAL PROTOCOL FORMAT,
INSTITUTIONAL ETHICAL REVIEW COMMITTEE,
FACULTY OF MEDICINE,
UNIVERSITY OF PERADENIYA, SRI LANKA
<Title>
Protocol Number: <number>
Grant Number:
Principal Investigator:
Sponsor: <sponsor name, if applicable; do not include IND/IDE
number>
Draft or Version Number: <x.x>
<Day Month Year>
1
STATEMENT OF COMPLIANCE
The study (Title of the study) will be conducted in accordance with the International
Conference on Harmonisation guidelines for Good Clinical Practice (ICH E6).
The signature below constitutes the approval of this protocol and the attachments,
and provides the necessary assurances that this trial will be conducted according to
all stipulations of the protocol, including all statements regarding confidentiality, and
according to local legal and regulatory requirements and ICH guidelines, and the
conditions imposed by the IERC, Faculty of Medicine, University of Peradeniya, Sri
Lanka.
Principal Investigator or Clinical Site Investigator:
Signed:
Date:
Name:
Title:
{For multi-site studies, the protocol should be signed by the clinical site investigator
who is responsible for the day to day study implementation at his/her specific clinical
site.
LIST OF ABBREVIATIONS
{Please add all disease or study-specific abbreviations/acronyms in this section.
Modify this list as needed for your particular study and remove abbreviations that are
not used in the document.}
2
PROTOCOL SUMMARY
{Limit to 1-2 pages; put key words in boldface in Protocol Summary.}
Title:
Study design:
<A brief overview of the study design, including study groups,
schedule of interventions, schedule for specimen or data
collection, and analyses to be performed.>
{The précis should be only a few sentences in length. A
detailed schematic describing all visits and assessments
(schedule of events) should be included as Appendix A.}
Objectives:
<Insert objectives copied from the body of the protocol.
Include the primary objective and secondary objectives and
specify outcome measures.>
Primary (General):
Secondary (Specific):
Population:
<Population information, including sample size, gender, age,
demographic group, general health status, geographic
location.>
Phase:
<I, II, III, or IV (if applicable)>
Number of Sites:
<Insert a list of sites if 3 or fewer sites; for more than 3 sites,
insert the number of sites only, and list the sites in Section 1.>
Description of
Intervention:
<Describe the intervention. If intervention is a drug, include
dose and route of administration. For a non-pharmaceutical
study (device, procedure or behavioral intervention), provide
brief description.>
Study Duration:
<Estimated time (in months) from when the study opens to
enrollment until completion of data analyses.>
Subject
Participation
Duration:
<Time it will take to conduct the study for each individual
subject.>
Estimated Time to
Complete
Enrollment:
<Estimated time from enrollment into study of the first subject
to enrollment into study of the last subject.>
3
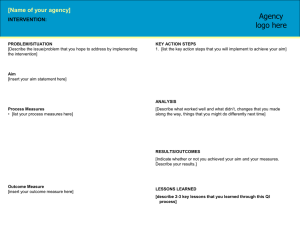
FLOWCHART OF THE STUDY DESIGN:
{The diagram below shows the preferred format and the level of detail needed to
convey an overview of study design. Complete each text box with study-specific
information and adapt the diagram to illustrate your study design (e.g., changing
method of assignment to study group, adding study arms, visits, etc.). The time
point(s) indicated in the schematic should correspond to the time point(s) in Section
7 of the protocol, Study Schedule, e.g., Visit 1, Day 0; Visit 2, Day 30 ± 7; etc.}
Prior to
Enrollment
Total N: Obtain informed consent. Screen potential subjects by inclusion and
exclusion criteria; obtain history, document.
Randomize
Arm 1
N subjects
Arm 2
N subjects
Visit 1
Time Point
Perform baseline assessments.
(list specimens to be collected, examinations or imaging or laboratory assays to
be performed, questionnaires to be completed)
Administer initial study intervention.
Visit 2
Time Point
Repeat study intervention (if applicable).
Visit 3
Time Point
Follow-up assessments of outcome measures and safety
(list specimens to be collected, examinations or imaging or laboratory assays to
be performed, questionnaires to be completed)
Visit 4
Time Point
Follow-up assessments of outcome measures and safety
(list specimens to be collected, examinations or imaging or laboratory assays to
be performed, questionnaires to be completed)
Visit X
Time Point
Final Assessments
List analyses to be performed
4
1 CONTACT INFORMATION, RESPONSIBILITIES OF THE CLINICAL TRIAL
COMMITTEE
{Provide the following information for each individual:
Name, degree, title, Institution Name, Address, Phone Number, Fax Number, Email}
Principal
Investigator:
Co-investigators:
Clinical Site
Investigators:
<if applicable, investigator name, institution>
Institutions:
{List study sites, clinical laboratory (ies), data coordinating
centers, and other medical or technical departments and/or
institutions, as applicable.
Provide the following information for each organization or
institution:
Institution Name, Address, Contact Person/Local Investigator
Phone Number, Fax Number, Email}
Other Key
Personnel:
{Consider listing, for example:
Collaborating Officials
Major international collaborators, if not included as site
investigators
Protocol data manager
1.1 Internal Trial Committees
Describe the role and responsibilities of each investigator in the committee. If no
committee is established, provide a valid justification.
1.2 Independent Safety and Data Monitoring Committee
Describe the role and composition of the Independent Safety and Data Monitoring
Committee (SDMC) (Define membership, function, frequency of review, stopping
rules). It is advisable to establish terms of reference for an SDMC and to include
them as appendices to the protocol. If no SDMC will be established, include a valid
justification for not having a SDMC in this section.
1.3 Sponsor
Provide the details of the person, collaboration or institution accepting the
responsibilities of the Sponsor for the study. A sponsor of a clinical research project
takes responsibility for the initiation, management, and/or financing of research.
5
1.4 Funding and resources
This section should describe how the study will be financed, but should not contain
specific amounts. Also state the source of other resources significant to the study,
such as study drug, if these were provided separately.
Example text: “This study is financed through a grant from the University of
Peradeniya, Grant No. ……………”
6
2 INTRODUCTION: BACKGROUND INFORMATION AND SCIENTIFIC
RATIONALE
2.1
Background Information
<Insert text>
{This section should include brief background information for this trial. It should not
be a copy of the background information from a grant application.
Include:
A brief description of the health problem that the study will address
The name and description of the study intervention/study product(s)
Discussion of important research relevant to the study that provides
background and scientific justification for the study (include findings from in
vitro studies, preclinical in vivo studies, and relevant clinical trials)
A brief description of the study’s overall goal
Applicable clinical, epidemiological, or public health background or context of
the study
Importance of the study and any relevant treatment issues or controversies}
2.2
Rationale
<Insert text>
{Include a description of, and justification for, the route of administration, dosage,
dosing regimen, intervention periods, or behavioral intervention methods and
selection of study population. Include a statement of the hypothesis.}
2.3
Potential Risks and Benefits
2.3.1
Potential Risks
<Insert text>
{Describe in detail any physical, psychological, social, legal, economic, or any other
anticipated risks to study subjects. Include risks of study intervention and other study
procedures.
One or more of the following may serve as the source of risk information:
Package insert for a licensed product
Investigator’s Brochure (IB) for an investigational product
Preclinical data reports
Literature search and review (include references)}
7
2.3.2
Potential Benefits
<Insert text>
{If the research is beneficial, describe any physical, psychological, social, legal, or
any other anticipated benefits to subjects. While it may not provide direct benefit to
subjects, the importance of the knowledge that may result from the study may be
mentioned.
Note: Compensation to subjects is not considered a “benefit.”
8
3 .OBJECTIVES
3.1
Study Objectives (General/Primary and Specific/Secondary)
<Insert text>
{Provide a detailed description of the one primary objective and any secondary
objectives of the study. An objective is the reason for performing the study in terms
of the scientific question to be answered. The primary objective is the main question.
This objective generally drives statistical planning for the trial (e.g., calculation of the
sample size to provide the appropriate power for statistical testing). Secondary
objectives are goals that will provide further information on the use of the
intervention.
Express each objective as a statement of purpose (e.g., to assess, to determine, to
compare, to evaluate) and include:
3.2
General purpose (e.g., feasibility, acceptability, efficacy, safety, tolerability,
pharmacokinetics) and/or specific purpose (e.g., dose-response, superiority to
placebo, mechanisms of action, effect of an intervention on disease incidence,
disease severity, or health behavior)
Name(s) of intervention (e.g., procedure, drug, biologic, behavioral
intervention) being evaluated, specification of doses or dose ranges to be
studied, dose regimens, intervention frequency}
Study Outcome Measures
<Insert text>
{This section should include the methods for assessing how the objectives are met,
i.e., the study outcome measures.
An outcome measure is a specific measurement or observation used to assess the
effect of the study intervention. Outcome measures should be prioritized and should
correspond to the study objectives and hypotheses being tested. Give succinct but
precise definitions of the outcome measures used to address the study’s primary
objective and key secondary objectives (e.g., specific laboratory tests that define
safety or efficacy, clinical assessments of disease status, assessments of
psychological characteristics, assessments of individual or group oral health
behaviors, assessments of healthcare visit attendance, etc.). Include the study visits
or time points at which data will be recorded or samples will be obtained.}
3.2.1
Primary
<Insert text>
{Generally, there should be just one primary outcome measure that will provide a
clinically relevant, valid, and reliable measure of the primary objective. Additional
measures may require an adjustment to the sample size calculations and p-value
threshold.
9
3.2.2
Secondary
<Insert text>
{Describe secondary outcome measures, whether they add information about the
primary objective or address secondary objectives. Discuss their importance and
role in the analysis and interpretation of study results.}
10
4 STUDY DESIGN
<Insert text>
{The scientific integrity of the trial and the credibility of the data from the trial depend
substantially on the trial design. Include a brief paragraph or bulleted text describing
the trial design. This section should include:
A brief description of the type/design of trial to be conducted (e.g.,
randomized, placebo-controlled, double-mask, parallel group, cross-over,
open-label, dose-escalation, dose-ranging)
A description of the study population (e.g., healthy/sick, inpatient/outpatient,
demographic groups). Do not list inclusion/exclusion criteria here, as these
will be listed in Sections 5.1 and 5.2.
A brief discussion of the rationale for design features
Phase of trial, if applicable
Single or multicenter
The number of study groups/arms
Description of study groups/arms including sample size (including a table, if
appropriate); stratifications that will affect enrollment
Approximate time to complete study enrollment
The expected duration of subject participation
Identification and specifics of administration of the study intervention and its
control or comparison (e.g., placebo, current standard of care treatment, etc.)
A brief description of the sequence and duration of all trial periods, including
follow-up (specify individual subjects vs. entire trial). Details of study visit
schedules will be included in Section 7, Study Schedule.
Planned variation in intervention dose or schedule (e.g., dose escalation)
A brief summary of methods for collecting data for assessment of study
objectives (detailed methods will be included in Section 8)
Other protocol-specific details, such as centralization of evaluations (e.g.,
central laboratory or central reading center for clinical scans)}
11
5 STUDY ENROLLMENT AND WITHDRAWAL
{In subsections 5.1 to 5.6, define the study population, describe subject recruitment,
and discuss issues related to subject withdrawal. The study population should be
appropriate for the stage of the study and the development stage of the study
product or other intervention. Address the following in these subsections as
applicable:
Provide the target sample size; identify anticipated number to be screened in
order to reach the target enrollment.
Specify approach(es) for conforming with GCP policy on inclusion of women
and minorities. Include numbers of women and minorities expected to be
recruited, or provide justification if women and/or minorities will not be
recruited.
Indicate from where the study population will be drawn (e.g., inpatient hospital
setting, outpatient clinics, student health service, or general public). Where
appropriate (single center studies), include names of hospitals, clinics, etc.
If the study intends to enroll children, pregnant women, prisoners, or other
vulnerable populations, what additional protective measures used.
Use the following guidelines when developing subject eligibility criteria to be
listed in subsections 5.1 and 5.2:
The eligibility criteria should provide a definition of subject characteristics
required for study entry.
The risks of the intervention should be considered in the development of the
inclusion/exclusion criteria so that risk is minimized.
The same criterion should not be listed as both an inclusion and exclusion
criterion (e.g., do not state age >32 years old as an inclusion criterion and age
≤32 years old as an exclusion criterion).
Identify specific laboratory tests or clinical characteristics that will be used as
criteria for enrollment.
If reproductive status (i.e., pregnancy, lactation, reproductive potential) is an
eligibility criterion, provide specific contraception requirements (e.g., licensed
hormonal methods).}
5.1
Subject Inclusion Criteria
<Insert text>
{Provide a statement that individuals must meet all of the inclusion criteria in order to
be eligible to participate in the study and then list each criterion.}
Example :In order to be eligible to participate in this study, an individual must meet all of the
following criteria:
Provide signed and dated informed consent form
12
Willing to comply with all study procedures and be available for the duration of
the study
Male or female, aged XX to XX
In good general health as evidenced by medical history or Diagnosed with
specific condition/disease or Exhibits specific clinical signs or symptoms or
physical/oral examination findings
Laboratory results within a specific range
Women of reproductive potential must use highly effective contraception
{specify methods of contraception acceptable for the study, e.g., licensed
hormonal methods.}
Men of reproductive potential must use condoms {if appropriate for study}.
{End example text}
5.2
Subject Exclusion Criteria
<Insert text>
{Provide a statement that all individuals meeting any of the exclusion criteria at
baseline will be excluded from study participation and then list each criterion.}
Example :An individual who meets any of the following criteria will be excluded from
participation in this study:
Medical condition, laboratory finding, or physical exam finding {specify, e.g.,
vital signs outside of specific range} that precludes participation
Use of disallowed concomitant medications {specify}
Presence of <specific devices (e.g., orthodontic appliances, dentures)>
Recent febrile illness that precludes or delays participation {specify time
frame}
Pregnancy or lactation
Known allergic reactions to components of the study product(s)
Treatment with another investigational drug or other intervention {within a
specified time frame}
History of or current tobacco, drug or alcohol use {define parameters for
exclusion}
Characteristics of household or close contacts {e.g., household contacts who
are immunocompromised, residence in same household as a subject already
participating in study, if blinding or compliance could potentially be
compromised}
13
5.3
Anything that would place the individual at increased risk or preclude the
individual’s full compliance with or completion of the study.
Strategies for Recruitment and Retention
<Insert text>
{Identify strategies for subject recruitment and retention. If subjects will be
compensated for study participation, describe amount and schedule of payments. If
the study requires long-term subject participation, describe procedures that will be
used to enhance subject retention (e.g., multiple methods for contacting subjects,
visit reminders, incentives for visit attendance, etc.)}
5.4
Treatment Assignment Procedures
<Insert text>
{This section should describe the methods of assigning subjects to study group
including randomization procedures (if applicable to the study design). It should
include a description or a table that describes how study subjects will be assigned to
study groups, without being so specific that masking or randomization might be
compromised (e.g., the ratio between intervention and placebo groups may be stated
but the randomization block sizes should not.)}
5.4.1
Randomization Procedures (if applicable)
<Insert text>
{Include plans for the maintenance of trial randomization codes. The timing and
procedures for planned and unplanned breaking of randomization codes should be
included.}
5.4.2
Masking (blinding) Procedures (if applicable)
<Insert text>
{State whether the intervention arms will be masked if the study includes more than
one intervention. Plans for maintaining appropriate masking for the study should be
discussed. }
5.5
Subject Withdrawal
<Insert text>
{Subjects may withdraw voluntarily from the study or the investigator may terminate
a subject's participation.}
5.5.1
Reasons for Withdrawal
<Insert text>
{Provide a list of reasons subjects may be withdrawn from the study. It may be
appropriate to provide distinct discontinuation criteria for subjects and cohorts. If so,
both sets of criteria should be listed separately and the distinction between the two
14
must be stated clearly. Also note that subjects may withdraw voluntarily from
participation in the study at any time.}
Example:-}
Subjects are free to withdraw from participation in the study at any time upon
request.
An investigator may terminate a study subject’s participation in the study if:
Any clinical adverse event (AE), laboratory abnormality, or other medical
condition or situation occurs such that continued participation in the study
would not be in the best interest of the subject.
The subject meets an exclusion criterion (either newly developed or not
previously recognized) that precludes further study participation.
{End sample text}
5.5.2
Handling of Subject Withdrawals or Subject Discontinuation of
Study Intervention
<Insert text>
{Describe efforts that will be made to continue follow-up of withdrawn subjects or
subjects who discontinue study intervention, especially for safety and efficacy
outcome measures (if applicable). Every effort must be made to undertake protocolspecified safety follow-up procedures to capture adverse events (AEs), serious
adverse events (SAEs), and unanticipated problems (UPs).
This section should include a discussion of replacement of subjects who withdraw or
discontinue early, if replacement is allowed.}
5.6
Premature Termination or Suspension of Study
<Insert text>
{List possible reasons for termination or suspension of the study, e.g., study closure
based on principal investigator (PI) decision, or IERCdecision. For any study that is
prematurely terminated or suspended, the PI will promptly inform the IERC and
Sponsor and provide the reason(s) for the termination or suspension.}
Example:This study may be suspended or prematurely terminated if there is sufficient
reasonable cause. Written notification, documenting the reason for study
suspension or termination, will be provided by the suspending or terminating party to
<investigator, funding agency, the Investigational New Drug (IND) /Investigational
Device Exemption (IDE) sponsor and regulatory authorities>. If the study is
prematurely terminated or suspended, the principal investigator will promptly inform
the IERC, FM, Peradeniya and will provide the reason(s) for the termination or
suspension.
Circumstances that may warrant termination include, but are not limited to:
15
Determination of unexpected, significant, or unacceptable risk to subjects.
Insufficient adherence to protocol requirements.
Data that is not sufficiently complete and/or evaluable.
Determination of futility.
{End sample text}
16
6 STUDY INTERVENTION
{An interventional study may involve an investigational drug or device or an
approved drug or device (Section 6.1), and/or a surgical or other intervention
(Section 6.7). Depending on the type of intervention(s) in your study, some of the
sections below may not apply. Complete applicable sections and delete sections
and subsections that do not apply (including headings). For example, if your study
involves only a behavioral intervention, delete Sections 6.1 to 6.6 and 6.7 to 6.10;
numbering of behavioral section headers will then automatically update, so that the
first behavioral section becomes Section 6.1, etc. Include additional subsections, if
necessary.}
6.1
Study Product Description
<Insert text>
{If the study does not use a study product, delete this section, including the
heading and associated subheadings.
Product information can usually be obtained from:
Investigator’s Brochure, if available, for investigational drug or biologic
package insert, for licensed drug or biologic
proposed labeling and material safety data sheet for investigational device
final labeling for a marketed device.
Provide this study product information to all investigators and IERC. .
If multiple products are to be evaluated, this section and the following sections
should be repeated for each product and the sections should be renumbered
accordingly. Include sections to describe placebo or control product.}
6.1.1
Acquisition
<Insert text>
{Describe how the study product will be acquired (e.g., an investigational product
may be supplied by the manufacturer or sponsor, an approved product may be
acquired from the hospital pharmacy, etc.)}
6.1.2
Formulation, Packaging, and Labeling
<Insert text>
{Describe the formulation, packaging, and labeling of the study product as supplied.}
6.1.3
Product Storage and Stability
<Insert text>
{Describe product’s storage needs. Include storage requirements and stability
(temperature, humidity, security, and container).
17
Provide additional information regarding stability and expiration time for studies in
which multidose vials are entered (i.e., the seal is broken).}
6.2
Dosage, Preparation and Administration of Study Product
<Insert text>
{List study product(s), route, doses, and frequency of administration. Include
thawing, diluting, mixing, and reconstitution or other preparation instructions, as
appropriate. Include any specific instructions or safety precautions for administration
of study products or masking of the product or the study staff administering it.
Include maximum hold time and conditions of product once thawed, mixed, diluted,
reconstituted, etc.}
6.3
Modification of Study Product Administration for a Subject
<Insert text>
{Clearly explain instructions for modification of dose due to toxicity or any other
reason. Address dose modifications for specific abnormal laboratory values of
concern or other AEs that are known to be associated with the planned intervention
regimen. Do not restate reasons for withdrawal of subjects. Cross-reference
relevant sections, as appropriate.}
6.4
Accountability Procedures for the Study Product
<Insert text>
{Provide plans for how the study product will be distributed, including participation of
a drug repository, frequency of product distribution, amount of product shipped,
device tracking procedures, and plans for return of unused product.}
6.5
Assessment of Subject Compliance with Study Product Administration
<Insert text>
{If applicable, include in this section plans for compliance assessment (e.g.,
questionnaires, direct observation, pill counts).}
6.6
Concomitant Medications/Treatments
<Insert text>
{This section should be consistent with the medications restrictions in the
inclusion/exclusion criteria.
Describe the data that will be recorded related to permitted concomitant medications
and/or treatments. Include details about when the information will be collected (at
screening, at all study visits, etc.). Discuss any rescue treatments or medications
that are included in the study design.}
6.7
Study Procedural Intervention(s) Description
<Insert text>
18
{If the study does not use a procedural intervention, delete this section,
including the heading and associated subheadings.
Describe the surgical or other medical procedural intervention(s) that will be tested in
the study. If one or more intervention(s) will be compared to a control intervention or
to treatment as usual, include a general description of these. Detailed descriptions of
the intervention(s), including any intervention manuals, detailed procedures, subject
handouts, etc., can be provided in a separate Manual of Procedures.}
6.8
Administration of Procedural Intervention
<Insert text>
{Include information about who will administer the intervention and how the
intervention will be administered. In addition, describe the schedule of the
intervention procedure(s), including the number of interventions, frequency of the
intervention delivery, and the approximate duration of each intervention.}
6.9
Procedures for Training of Clinicians on Procedural Intervention
<Insert text>
{Describe any means used to standardize the surgical or procedural intervention
(e.g., single operator, calibration, images, minimal time of therapy required,
specialized required instruments and/or materials, required measurements).
Describe any re-standardization or re-evaluation procedures and time intervals
between reassessments.}
6.10
Assessment of Clinician and/or Subject Compliance with Study
Procedural Intervention
<Insert text>
{If applicable, include in this section plans for compliance assessment (e.g.,
questionnaires, research record review, medical record review, laboratory result
review, telephone follow-up contacts, direct observation).}
19
7 STUDY SCHEDULE
{Information outlined in this section should refer to and be consistent with the
information in the Schedule of Events in Appendix A and in Section 8.
Provide a schedule of initial, intermediate, and final study visits, and include all
contacts with subjects, e.g., telephone contacts. State permissible time windows for
study visits, e.g., Day 7 ± 1 day (weekly visits will have a small window, whereas a 6month follow-up visit might have a window of several weeks). When establishing
visit intervals and windows, consider feasibility and relevance to study outcome
measures, and take into account how weekends and holidays will affect the
windows.
For each visit, identify the purpose and describe what will occur at the visit. If any of
the procedures occurring at a visit are completed as part of standard clinical care
rather than as study procedures, identify them as such.}
7.1
Screening
<Insert text>
{Include any evaluations necessary to assess whether an individual meets eligibility
criteria. Discuss the sequence of events that should occur during screening and the
decision points regarding eligibility. List the time frame prior to enrollment within
which screening tests and evaluations must be done (e.g., within 28 days prior to
enrollment).
This section must include instructions for obtaining signed informed consent.
If screening procedures are required for eligibility (e.g., review of medical
records, clinical examination, or laboratory tests), they may be performed
under a separate screening consent form. State if a separate screening
consent will be used. If a separate screening consent form will not be used,
the study consent form must be signed prior to screening.
Example:Screening Visit (Day -28 to -1) {include a window that is appropriate for the study}
Obtain and document consent from potential subject on screening consent
form.
Review medical/dental history to determine eligibility based on
inclusion/exclusion criteria.
Review medications history to determine eligibility based on
inclusion/exclusion criteria.
Perform medical/dental examinations needed to determine eligibility.
Collect blood/urine/saliva.
Schedule study visits for individuals who are eligible and available for the
duration of the study.
20
Provide potential subjects with instructions needed to prepare for first study
visit {specify instructions to be provided}.
{End sample text}
7.2
Enrollment/Baseline
<Insert text>
{Discuss evaluations/procedures necessary to assess or confirm whether an
individual still meets the eligibility criteria and may be enrolled, and specify what will
be recorded at baseline for later outcome measure comparison after study
intervention (e.g., baseline signs and symptoms prior to treatment). Discuss the
sequence of events that should occur during enrollment and/or initial administration
of study product or intervention. List any special conditions (e.g., results of the
pregnancy test must be negative and available prior to administration of study
product or intervention). List the procedures for administering the study product or
intervention and follow-up procedures after administration.
Example:Enrollment/Baseline Visit (Visit 1, Day 0)
Obtain and document consent from subject on study consent form.
Verify inclusion/exclusion criteria.
Obtain demographic information, medical/dental history, medication history,
alcohol, and tobacco use history.
Record results of physical and dental examinations.
Collect blood/urine/saliva/other specimen.
Administer the intervention. Following administration of <intervention>
o Assess pain on visual analog scale
o Administer Symptoms Questionnaire
{End sample text}
7.3
Intermediate Visits
<Insert text>
{List each intervention or evaluation visit, including visit number and visit window.
For each visit, list the procedures to be completed (in chronological order, if
applicable).
Confirm that the procedures listed are consistent with those included in the Schedule
of Events (Appendix A).}
Example:Visit 2, Day X ± Y
{Repeat for each visit, providing a study-appropriate window for the visit.}
21
Record adverse events as reported by subject or observed by investigator.
Record results of physical and dental examinations.
Collect blood/urine/saliva.
Administer the <intervention>.
Record subject’s compliance with <intervention>.
Following administration of <intervention>
o Assess vital signs
o Administer Symptoms Questionnaire
{End sample text}
7.4
Final Study Visit
<Insert text>
{Define when the final study visit should occur and any special
procedures/evaluations or instructions to the subject. Describe provisions for followup of ongoing AEs/SAEs. If study results will be shared with subjects, discuss when
and how subjects will receive this information.
Example:Final Study Visit (Final Visit, Day X ± Y)
Record adverse events as reported by subject or observed by investigator.
Record results of physical and dental examinations.
Collect blood/urine/saliva.
Record subject’s compliance with <intervention>.
Provide final instructions to subject {e.g., follow-up of ongoing adverse events,
oral hygiene instructions}.
{End sample text}
7.5
Withdrawal Visit
<Insert text>
{If subject withdraws early or investigator terminates subject participation, specify
which of the evaluations required for the final study visit should be offered to the
subject.}
7.6
Unscheduled Visit
<Insert text>
{Specify how unscheduled visits will be handled and documented.}
22
8 STUDY PROCEDURES /EVALUATIONS
{Information outlined in the Procedures/Evaluations section should refer to and be
consistent with the information in the Schedule of Events in Appendix A.
In the following subsections, describe procedures for collection of all study data
including clinical observations, laboratory results, biospecimens, images,
questionnaire responses.
All procedures listed here should be specific to the study and not part of standard
clinical care. Procedures completed during the study as part of normal standard of
clinical care should be identified as such and summarized in a separate section.}
8.1
Study Procedures/Evaluations
<Insert text>
{List and describe all study procedures and evaluations to be done as part of the
study. Possible content includes:
8.2
Medical history (describe what is included for history, e.g., time-frame
considerations, whether history will be obtained by interview or from medical
records).
Medications history (e.g., describe if a complete medications history is
needed, or if only currently taken medications should be included; prescription
medications only or also over-the-counter). Assessment of eligibility should
include a review of permitted and prohibited medications.
Physical examination (list the vital signs [including height and weight] and
organ systems to be assessed.); if appropriate, discuss what constitutes a
targeted physical examination and at what visits it may occur.
Oral exams, including caries assessments or periodontal measurements.
Radiographic or other imaging assessments.
Biological specimen collection.
Administration of questionnaires or other instruments for subject-reported
outcomes, daily diary.
Observation and coding of subject behaviors.}
Laboratory Procedures/Evaluations
8.2.1
Clinical Laboratory Evaluations
<Insert text>
{List all laboratory evaluations to be done as part of the study (e.g., hematology,
clinical chemistry, urinalysis, pregnancy testing). Differentiate screening laboratories
from those taken after treatment. Include specific test components and estimated
volume and type of specimens needed for each test. Specify laboratory methods to
provide for appropriate longitudinal and cross-sectional comparison (e.g., use of
consistent laboratory method throughout study, use of single laboratory for multi-site
23
studies). If more than one laboratory will be used, specify which evaluations will be
done by each laboratory.}
8.2.2
Special Assays or Procedures
<Insert text>
{List special assays or procedures required to assess the effect of the intervention
(e.g., immunology assays, pharmacokinetic studies, images, flow cytometry assays,
microarray, DNA sequencing). For research laboratory assays, include specific
assays, estimated volume and type of specimen needed for each test. For
procedures, provide special instructions or precautions. If more than one laboratory
will be used, specify which assays will be done by each laboratory.}
8.2.3
Specimen Preparation, Handling, and Storage
<Insert text>
{Special instructions for the preparation, handling, and storage of specimens should
be explained clearly in this section, including specific time requirements for
processing, required temperatures, aliquots of specimens, where they will be stored,
and how they will be labeled.}
8.2.4
Specimen Shipment
<Insert text>
{State the frequency with which specimens are to be shipped and to what address.
Include contact information for laboratory personnel. Include days and times
shipments are allowed, and any labeling requirements for specimen shipping. Also,
include any special instructions such as dry ice or wet ice or the completion of a
specimen-tracking log.}
24
9 ASSESSMENT OF SAFETY
To establish a meaningful safety system for the study, consider the risks of the study
intervention and other study procedures as well as the characteristics of the study
population (healthy individuals, individuals with disease, and vulnerable populations
such as children). This section should be tailored for specific study characteristics,
including but not limited to the following:
the study involves an investigational new drug or investigational device;
the study requires selection of an appropriate toxicity grading scale;
the study involves risks to individuals other than research subjects (e.g., study
interventionists, other study staff, family members or associates of study
subjects, communities, etc.);
reporting of certain events (e.g., suspected child abuse or substance abuse)
is mandatory because of the study population or study design characteristics;
the study is conducted at multiple sites, and will require centralized safety
oversight.}
9.1
Specification of Safety Parameters
<Insert text>
{Describe safety parameters that will be recorded in the safety reporting system.
“Recording” refers to documenting data in the study database. Define what data will
require reporting for protection of human subjects.}
9.1.1
Unanticipated Problems
<Insert text>
Example:Unanticipated problems involving risks to subjects or others to include, in general,
any incident, experience, or outcome that meets all of the following criteria:
unexpected in terms of nature, severity, or frequency given (a) the research
procedures that are described in the protocol-related documents, such as the
IRB-approved research protocol and informed consent document; and (b) the
characteristics of the subject population being studied;
related or possibly related to participation in the research (“possibly related”
means there is a reasonable possibility that the incident, experience, or
outcome may have been caused by the procedures involved in the research);
and
suggests that the research places subjects or others at a greater risk of harm
(including physical, psychological, economic, or social harm) than was
previously known or recognized.
{End sample text}
25
{Per the definition, only a subset of adverse events would be characterized as
unanticipated problems. There are other types of incidents, experiences, and
outcomes that are not considered adverse events, but are characterized as
unanticipated problems (e.g., breach of confidentiality or other incidents involving
social or economic harm).}
9.1.2
Adverse Events
<Insert text>
{The definition of adverse event here is drawn from the WHO guidance; for some
studies, the ICH E6 definition may be more appropriate.}
Example:An adverse event is any untoward or unfavorable medical occurrence in a human
subject, including any abnormal sign (for example, abnormal physical finding or
laboratory finding), symptom, or disease, temporally associated with the subject’s
participation in the research, whether or not considered related to the subject’s
participation in the research.
{End sample text}
9.1.3
Serious Adverse Events
<Insert text>
{SAEs are a subset of all AEs.}
Example:A serious adverse event (SAE) is one that meets one or more of the following
criteria:
Results in death
Is life-threatening (places the subject at immediate risk of death from the
event as it occurred)
Results in inpatient hospitalization or prolongation of existing hospitalization
Results in a persistent or significant disability or incapacity
Results in a congenital anomaly or birth defect
An important medical event that may not result in death, be life threatening, or
require hospitalization may be considered an SAE when, based upon
appropriate medical judgment, the event may jeopardize the subject and may
require medical or surgical intervention to prevent one of the outcomes listed
in this definition.
{End sample text}
{Some protocols may list events specific to the protocol that should be reported as
serious. Examples might be post-extraction bleeding in anticoagulated subjects and
anaphylactic reaction after lidocaine or analgesic administration.}
26
9.2
Time Period and Frequency for Event Assessment and Follow-Up
<Insert text>
{Describe how AEs will be recorded and how AEs and SAEs will be followed until
resolved or considered stable. Specify procedures for recording and follow-up of,
SAEs, and AEs that are consistent with the Schedule of Events. Include duration of
follow-up after appearance of events (e.g., 1 week, 2 months).}
Example:Unanticipated problems will be recorded in the data collection system throughout the
study.
The PI will record all reportable events with start dates occurring any time after
informed consent is obtained until 7 (for non-serious AEs) or 30 days (for SAEs) after
the last day of study participation. At each study visit, the investigator will inquire
about the occurrence of AE/SAEs since the last visit. Events will be followed for
outcome information until resolution or stabilization.
{End sample text}
9.3
Characteristics of an Adverse Event
9.3.1
Relationship to Study Intervention
<Insert text>
{All adverse events must have their relationship to study intervention or study
participation assessed as either related or not related. Evaluation of relatedness
must consider etiologies such as natural history of the underlying disease,
concurrent illness, concomitant therapy, study-related procedures, accidents, and
other external factors.
In a clinical trial, the study intervention must always be suspect.}
{Begin sample text}
To assess relationship of an event to study intervention, the following guidelines are
used:
1. Related (Possible, Probable, Definite)
a. The event is known to occur with the study intervention.
b. There is a temporal relationship between the intervention and event
onset.
c. The event abates when the intervention is discontinued.
d. The event reappears upon a re-challenge with the intervention.
2. Not Related (Unlikely, Not Related)
a. There is no temporal relationship between the intervention and event
onset.
27
b. An alternate etiology has been established.
{End sample text}
9.3.2
Expectedness of SAEs
<Insert text>
{The risk information to assess expectedness can be obtained from preclinical
studies, the investigator’s brochure, published medical literature, the protocol, or the
informed consent document.}
Example:The Study PI will be responsible for determining whether an SAE is expected or
unexpected. An adverse event will be considered unexpected if the nature, severity,
or frequency of the event is not consistent with the risk information previously
described for the intervention.
{End sample text}
9.3.3
Severity of Event
<Insert text>
{Describe the method of grading an adverse event for severity. Many toxicity tables
are available for use and are adaptable to various study designs. One of the
commonly used toxicity table is as follows}
Example:The following scale will be used to grade adverse events:
1. Mild: no intervention required; no impact on activities of daily living (ADL)
2. Moderate: minimal, local, or non-invasive intervention indicated; moderate
impact on ADL
3. Severe: significant symptoms requiring invasive intervention; subject seeks
medical attention, needs major assistance with ADL
{End sample text}
9.4
Reporting Procedures
<Insert text>
{Institutions engaged in human subjects research conducted or supported by the
Department of Health Service must have written procedures for ensuring prompt
reporting to the IERC, appropriate institutional officials, and any supporting
department or agency head of any unanticipated problem involving risks to subjects
or others
Describe the protocol-specific reporting procedures, including the individual
responsible for each step (e.g., the investigator, the Data Coordinating Center, the
28
Medical Monitor), which forms should be completed, timeframes for reporting, how
reports will be distributed, and what follow-up is required.
Include specific details of reporting procedures for:
Deaths and life-threatening events
Other SAEs
Other adverse events
The sample text in the following sections may be customized by including IERCspecified reporting time frames or protocol-specific parameters (safety issues) that
need to be reported in an expedited fashion, either to the IERC, sponsor, or other
regulatory body. For multi-site studies, be cognizant of different IERC reporting
requirements.}
9.4.1
Unanticipated Problem Reporting to IERC
<Insert text>
Example:Incidents or events that are of unanticipated problems require the creation and
completion of an unanticipated problem report form. IERC recommends that
investigators include the following information when reporting an adverse event, or
any other incident, experience, or outcome as an unanticipated problem to the IERC:
appropriate identifying information for the research protocol, such as the title,
investigator’s name, and the IERC project number;
a detailed description of the adverse event, incident, experience, or outcome;
an explanation of the basis for determining that the adverse event, incident,
experience, or outcome represents an unanticipated problem;
a description of any changes to the protocol or other corrective actions that
have been taken or are proposed in response to the unanticipated problem.
To satisfy the requirement for prompt reporting, unanticipated problems will be
reported using the following timeline:
Unanticipated problems that are serious adverse events will be reported to the
IERC within 3 days of the investigator becoming aware of the event.
Any other unanticipated problem will be reported to the IERC within 1 weeks
of the investigator becoming aware of the problem.
All unanticipated problems should be reported to appropriate institutional
officials (as required by an institution’s written reporting procedures).
All unanticipated problems will be reported to IERC.
{End sample text}
29
9.4.2
Serious Adverse Event Reporting to IERC
<Insert text>
{Describe the SAE reporting procedures. Include description of when events are
reported to various oversight and regulatory groups.}
Example:Any AE meeting the specified Serious Adverse Event criteria will be submitted on an
SAE form to IERC. This report may be sent by fax or email.
This process applies to both initial and follow-up SAE reports.
The study clinician will complete a Serious Adverse Event Form and submit via fax
or email within the following timelines:
All deaths and immediately life-threatening events, whether related or
unrelated, will be recorded on the Serious Adverse Event Form and submitted
to IERC within 24 hours of site awareness.
Serious adverse events other than death and immediately life-threatening
events, regardless of relationship, will be reported to the IERC within 42 hours
of site awareness.
All SAEs will be followed until resolution or stabilization.
{End sample text}
{Other supporting documentation of the event may be requested and should be
provided as soon as possible.}
9.4.3
Reporting of Pregnancy
<Insert text>
{State the study’s pregnancy-related policy and procedure. Include appropriate
mechanisms for reporting to IERC, sponsor, study leadership and regulatory
agencies. Provide appropriate modifications to study procedures (e.g.,
discontinuation of treatment while continuing safety follow-up, requesting permission
to follow pregnant women to pregnancy outcome).}
9.5
Halting Rules
<Insert text>
{Describe safety findings that would prompt temporary suspension of enrollment
and/or study interventions until a safety review is convened (either routine or ad
hoc). The objective of the safety review is to decide whether the study (or
intervention for an individual or study cohort) should continue per protocol, proceed
with caution, be further investigated, be discontinued, or be modified and then
proceed. Suspension of enrollment (for a particular group, a particular study site or
for the entire study) is a potential outcome of a safety review.
30
Subsequent review of serious, unexpected, and related AEs by the IERC the
sponsor(s), or relevant local regulatory authorities may also result in suspension of
further trial interventions/administration of study product at a site. The IERC and
study sponsor(s) retain the authority to suspend additional enrollment and study
interventions/administration of study product for the entire study, as applicable.
Examples of findings that might trigger a safety review are the number of SAEs
overall, the number of occurrences of a particular type of SAE, severe AEs/reactions,
or increased frequency of events.}
31
10 CLINICAL SITE MONITORING
<Insert text>
{Based on a determination of study oversight requirements, clinical site monitoring
may be required. Site monitoring is conducted to ensure that the rights of human
subjects are protected, that the study is implemented in accordance with the protocol
and/or other operating procedures, and that the study uses high quality data
collection processes. The monitor will evaluate study processes based on ICH E6,
sponsor and, when appropriate, regulatory guidelines.
Include in this section a general description of the site monitoring planned for the
study. State who will conduct the monitoring. Indicate the frequency of monitoring
visits.
Example:- (adapt as needed for a specific study.}
Clinical site monitoring is conducted to ensure that the rights of human subjects are
protected, that the study is implemented in accordance with the protocol and/or other
operating procedures, and that the quality and integrity of study data and data
collection methods are maintained. The monitor will evaluate study processes and
documentation based on International Conference on Harmonisation (ICH), E6:
Good Clinical Practice guidelines (GCP).
Details of clinical site monitoring will be documented by the PI in collaboration with
the IERC and sponsor. The IERC will specify the frequency of monitoring, monitoring
procedures, the level of clinical site monitoring activities (e.g., the percentage of
subject data to be reviewed), and the distribution of monitoring reports.
Documentation of monitoring activities and findings will be provided to the site study
team, the study PIs, IERC. The IERC, FM, UP reserves the right to conduct
independent audits as necessary.
{End sample text}
32
11 STATISTICAL CONSIDERATIONS
{The following subsections describing statistical considerations should be “selfcontained” for coherence and ready reference. The statistical plan should show how
the study will answer the most important questions with precision and a minimum of
bias, while remaining feasible. Many elements below can be found in ICH guidance
document E9 (Statistical Principles for Clinical Trials) and the CONSORT statement
(http://www.consort-statement.org/), which describes standards for improving the
quality of reporting randomized controlled trials.}
11.1
Study Hypotheses
<Insert text>
{State the formal, testable, null, and alternate hypotheses for the primary objective
and key secondary objectives.}
11.2
Sample Size Considerations
<Insert text>
{Provide all information needed to validate your calculations, and also to judge the
feasibility of enrolling and following the necessary numbers of subjects.
Consider applicable items from the following list when describing sample size
determination:
Statistical method used to calculate the sample size
Outcome measure used for calculations (almost always the primary variable)
Test statistic
Type I error rate
Type II error rate
Method for adjusting calculations for planned interim analyses, if any
Assumptions used in calculations:
o Assumed event rate for dichotomous outcome (or mean or variance of
continuous outcome) for each study arm, justified and referenced by
historical data as much as possible
o Assumed dropout rates, withdrawal, cross-over to other study arms,
missing data, etc., also justified
o Approach to handling withdrawals and protocol violations, i.e., to what
extent data from withdrawn subjects will be evaluable (e.g., whether
subjects will be included in the “intent-to-treat” population), whether
withdrawn subjects will be replaced
Present calculations from a suitable range of assumptions to gauge the robustness
of the proposed sample size. Most assumptions are not accurate as point estimates.
Discuss whether the sample size also provides sufficient power for addressing
secondary objectives or for secondary analyses in key subgroup populations.}
33
11.3
Planned Interim Analyses (if applicable)
<Insert text>
{Describe the types of statistical interim analyses and stopping guidelines (if any)
that are proposed, including their timing.}
11.3.1 Safety Review
<Insert text>
{If statistical rules will be used to halt enrollment into all or a portion of the study (see
Section 9.5), describe the statistical techniques and their operating characteristics,
e.g., the probability of stopping under different safety event rates and the associated
number of subjects that would be enrolled.}
11.3.2 Efficacy Review
<Insert text>
{Provide the same information as in Section 11.3.1, but for efficacy outcome
measures. Also discuss the impact of the interim analysis (if being done) on the final
efficacy analyses, particularly on Type I error.
If formal interim analyses will be performed, provide unambiguous and complete
instructions so that an independent statistician could perform the analyses.}
11.4
Final Analysis Plan
<Insert text>
{Describe analyses for assessing the primary and secondary objectives.
Plans must clearly identify the analyses cohorts (e.g., “Per Protocol” or “Intent to
Treat,” as well as subsets of interest) and methods to account for missing, unused or
spurious data.
Discuss how outcome measures will be assessed and transformed, if relevant,
before analysis. (Examples: Is the primary variable binary, categorical, or
continuous? Will a series of measurements within a subject be summarized, such as
by calculating the area under the curve? For survival outcome measures, what are
the competing risks and censoring variables?)
For complex data analyses (e.g., multiple secondary objectives), an overview of the
statistical analyses may be provided here, with more details in a separate statistical
analysis plan written prior to performing any analyses.}
34
12 SOURCE DOCUMENTS AND ACCESS TO SOURCE DATA/DOCUMENTS
<Insert text>
{Source data are all information, original records of clinical findings, observations, or
other activities in a clinical trial necessary for the reconstruction and evaluation of the
trial. Examples of these original documents and data records include, but are not
limited to, hospital records, clinical and office charts, laboratory notes, memoranda,
subjects’ memory aid or evaluation checklists, pharmacy dispensing records,
recorded data from automated instruments, audio recordings of counseling sessions
or other data collection events, copies or transcriptions certified after verification as
being accurate and complete, photographs or digital photo files, x-rays, and subject
files and records kept at the pharmacy, at the laboratories, and medico-technical
departments involved in the clinical trial. It may be acceptable to use case report
forms (CRFs) as source documents.
Describe how source documents will be managed in the study. Specify what will be
considered source documents, how they will be maintained, and who will have
access to records.}
Example:- (adapt as needed to specify what will be source documents for your
study}
Study staff will maintain appropriate medical and research records for this study, in
compliance with ICH E6, Section 4.9 and regulatory and IERC requirements for the
protection of confidentiality of subjects. Study staff will permit authorized
representatives of IERC and regulatory agencies to examine (and when required by
applicable law, to copy) research records for the purposes of quality assurance
reviews, audits, and evaluation of the study safety, progress and data validity.
{End required text}
35
13 QUALITY CONTROL AND QUALITY ASSURANCE
<Insert text>
{This section will address the plans for local quality assurance and quality control.
Quality Management is the overall process of establishing and ensuring the quality of
processes, data, and documentation associated with clinical research activities. It
encompasses both quality control (QC), and quality assurance (QA) activities. All
sites conducting research are required to have a plan in place for assuring the
quality of the research being conducted.
Each site should have standard operating procedures (SOPs) and/or a quality
management plan that describe:
How data will be evaluated for compliance with the protocol and for accuracy
in relation to source documents.
The documents to be reviewed (e.g., CRFs, clinic notes, product
accountability records, specimen tracking logs, questionnaires, audio or video
recordings), who is responsible, and the frequency for reviews.
Who will be responsible for addressing quality assurance issues (correcting
procedures that are not in compliance with protocol) and quality control issues
(correcting errors in data entry).
Staff training methods and how such training will be tracked.
If applicable, calibration exercises conducted prior to and during the study to
train examiners and maintain acceptable intra- and inter-examiner agreement.
}
36
14 ETHICS/PROTECTION OF HUMAN SUBJECTS
14.1
Ethical Standard
<Insert text>
{Include in this section the guiding ethical principles being followed by the study.}
Example:The investigator will ensure that this study is conducted in full conformity with the
principles set forth in The Belmont Report: Ethical Principles and Guidelines for the
Protection of Human Subjects of Research, compliance with declaration of Helsinki,
CIOMS, and WHO.
{End required text}
{If the study is conducted at international sites, the statement could be as above
and/or could reference compliance with the Declaration of Helsinki, CIOMS,
International Ethical Guidelines for Biomedical Research Involving Human Subjects
(2002), or another country’s ethical policy statement, whichever provides the most
protection to human subjects.}
14.2
Institutional Ethical Review Committee
<Insert text>
{Each participating institution must provide for the review and approval of this
protocol and the associated informed consent documents and recruitment materials
by an appropriate IERC recognized by the Ministry of Health SL. Any amendments
to the protocol or consent materials must also be approved before they are placed
into use.
Example:- (modify as appropriate for a multi-site study)
The protocol, informed consent form(s), recruitment materials, and all subject
materials will be submitted to the IERC, FM, UP for review and approval. Approval
of both the protocol and the consent form must be obtained before any subject is
enrolled. Any amendment to the protocol will require review and approval by the
IERC before the changes are implemented in the study.
{End required text}
14.3
Informed Consent Process
<Insert text>
{Identify different consent forms that are needed for the study (e.g., screening, study
participation, future use of specimens, assent form for minors).
When a study includes subjects who may be enrolled in the trial only with the
consent of the subject’s legally authorized representative (e.g., minors or subjects
whose cognitive impairment is such that they are unable to give informed consent),
the subject should be informed about the trial to the extent compatible with the
37
subject’s understanding. If capable, the subject should assent and sign and
personally date the written consent form. A separate IERC-approved assent form,
describing (in simplified terms) the details of the study intervention, study
procedures, and risks may be used. Assent forms do not substitute for the consent
form signed by the subject’s legally authorized representative.
It is mandatory to translate all information and consent forms to Sinhala language
and where necessary to Tamil language.
For a multi-site study, each participating institution will be provided with a model
informed consent form. Each institution may revise or add information to comply
with institution consent templates, but may not remove procedural or risk content
from the model consent form.}
Example:
Informed consent is a process that is initiated prior to the individual agreeing to
participate in the study and continues throughout study participation. Extensive
discussion of risks and possible benefits of study participation will be provided to
subjects and their families, if applicable. A consent form describing in detail the
study procedures and risks will be given to the subject. Consent forms will be IERC
approved, and the subject is required to read and review the document or have the
document read to him or her. The investigator or designee will explain the research
study to the subject and answer any questions that may arise. The subject will sign
the informed consent document prior to any study-related assessments or
procedures. Subjects will be given the opportunity to discuss the study with their
surrogates or think about it prior to agreeing to participate. They may withdraw
consent at any time throughout the course of the study. A copy of the signed
informed consent document will be given to subjects for their records. The rights
and welfare of the subjects will be protected by emphasizing to them that the quality
of their clinical care will not be adversely affected if they decline to participate in this
study.
The consent process will be documented in the clinical or research record.
{End required text}
14.4
Exclusion of Women, Minorities, and Children (Special Populations)
<Insert text>
{Explain why any of these populations are excluded from study participation, or state
that individuals of any age, gender or racial/ethnic group may participate.}
14.5
Subject Confidentiality
<Insert text>
{Include procedures for maintaining subject confidentiality and any special data
security requirements. Describe who would have access to records, including the
investigator and other study staff, the clinical monitor, representatives of IERC or
other funding institutions. For some studies, it may be necessary to obtain a
Certificate of Confidentiality. A Certificate of Confidentiality protects researchers and
38
research institutions from being forced to provide identifying information on study
subjects to any state, or local authority.
Example:- (include Certificate of Confidentiality and Data Sharing Policy text, only if
applicable)
Subject confidentiality is strictly held in trust by the investigators, study staff, and the
sponsor(s) and their agents. This confidentiality is extended to cover testing of
biological samples and genetic tests in addition to any study information relating to
subjects.
The study protocol, documentation, data, and all other information generated will be
held in strict confidence. No information concerning the study or the data will be
released to any unauthorized third party without prior written approval of the sponsor.
The study monitor or other authorized representatives of the sponsor may inspect all
study documents and records required to be maintained by the investigator,
including but not limited to, medical records (office, clinic, or hospital) for the study
subjects. The clinical study site will permit access to such records.
Certificate of Confidentiality (if applicable)
{End sample text}
14.6
Future Use of Stored Specimens and Other Identifiable Data
<Insert text>
{Refer to Human Subject Regulations Decision Charts 2 and 5:
If residual specimens or other identifiable data will be maintained after the study is
complete, include the provisions for consent and the options that are available for the
subject to agree to the future use of his/her specimens, images, audio or video
recordings. Specify the location(s), if other than the clinical site, where specimens or
other data will be maintained, how long specimens or other data will be stored, if the
site's IERC will review future studies, and protections of confidentiality for any future
studies with the stored specimens or data (e.g., specimens will be coded, bar-coded,
de-identified, identifying information will be redacted from audio recording transcripts,
etc.). Include a statement that genetic testing will or will not be performed. A
Certificate of Confidentiality may be obtained if genomic testing is planned.}
39
15 DATA HANDLING AND RECORD KEEPING
<Insert text>
{Include instructions for data handling or record-keeping procedures required for
maintaining subject confidentiality, any special data security or data transfer
requirements, and record retention.
Briefly describe steps to be taken to ensure that the data collected are accurate,
consistent, complete, reliable, and in accordance with ICH E6. The description
should include reference to source documentation, CRFs, instructions for completing
forms, data handling procedures, and procedures for data monitoring.
Example:The investigators are responsible for ensuring the accuracy, completeness, legibility,
and timeliness of the data reported. All source documents should be completed in a
neat, legible manner to ensure accurate interpretation of data. The investigators will
maintain adequate case histories of study subjects, including accurate case report
forms (CRFs), and source documentation.
{End sample text}
15.1
Data Management Responsibilities
<Insert text>
{Include a general description as in the sample text below and add study-specific
details and information about the role of a data coordinating center, if applicable.}
Example:Data collection and accurate documentation are the responsibility of the study staff
under the supervision of the investigator. All source documents and laboratory
reports must be reviewed by the study team and data entry staff, who will ensure that
they are accurate and complete. Unanticipated problems and adverse events must
be reviewed by the investigator or designee.
{End sample text}
15.2
Types of Data
<Insert text>
{Indicate the types of data that will be collected, such as safety, laboratory (clinical,
immunology, pharmacokinetic, other study specific), and outcome measure data
(e.g., periodontal measurements, caries assessments, physical measurements,
questionnaire responses). Specify if safety data are collected in a separate
database.}
15.3
Study Records Retention
<Insert text>
40
{Specify the length of time for the investigator to maintain all records pertaining to
this study. Consideration should be given to FERCSL,FERCAP and ICH guidance,
state and local regulations.}
Example:Study records will be maintained for at least three years.
Study documents should be retained for a minimum of 2 years after the last approval
of a marketing application in an ICH region and until there are no pending or
contemplated marketing applications in an ICH region or until at least 2 years have
elapsed since the formal discontinuation of clinical development of the investigational
product. These documents should be retained for a longer period, however, if
required by local regulations. No records will be destroyed without the written
consent of the sponsor, if applicable. It is the responsibility of the sponsor to inform
the investigator when these documents no longer need to be retained.
{End sample text}
15.4
Protocol Deviations
<Insert text>
{Begin sample text}
A protocol deviation is any noncompliance with the clinical study protocol and Good
Clinical Practice. The noncompliance may be on the part of the subject, the
investigator, or study staff. As a result of deviations, corrective actions are to be
developed by the study staff and implemented promptly.
These practices are consistent with investigator and sponsor obligations in ICH E6:
Compliance with Protocol, Sections 4.5.1, 4.5.2, 4.5.3, and 4.5.4.
Quality Assurance and Quality Control, Section 5.1.1
Noncompliance, Sections 5.20.1 and 5.20.2.
All deviations from the protocol must be addressed in study subject source
documents and promptly reported to the IERC, according to their requirements.
{End sample text}
41
16 PUBLICATION/DATA SHARING POLICY
<Insert text>
{The publication and authorship policies should be established and briefly outlined in
this section. For example, for a study with multiple investigators, this section might
state that an Executive Committee will be responsible for developing publication
procedures and resolving authorship issues.}
Example:The International Committee of Medical Journal Editors (ICMJE) member journals
have adopted a clinical trials registration policy as a condition for publication. The
clinical trials are defined as any research project that prospectively assigns human
subjects to intervention or concurrent comparison or control groups to study the
cause-and-effect relationship between a medical intervention and a health outcome.
Medical interventions include drugs, surgical procedures, devices, behavioral
treatments, process-of-care changes, and the like. Health outcomes include any
biomedical or health-related measures obtained in patients or participants, including
pharmacokinetic measures and adverse events.
{End sample text}
42
17 LITERATURE REFERENCES
<Insert text>
{Include a list of relevant literature references in this section. Use a consistent, standard,
modern format, which might be dependent upon the required format for the anticipated
journal for publication (Vancouver method is preferred)
43