Instructions for Planning Using Clinical Reasoning Tool Clinical
advertisement
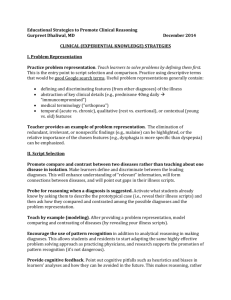
Instructions for Planning Using Clinical Reasoning Tool Clinical reasoning is the process by which clinicians solve the health problems of their patients. Clinical reasoning often leads to a diagnosis. For first and second year medical students, arriving at a diagnosis, while satisfying, is not the important objective in a PBL Case. Skilled clinicians use recognition of illness ‘scripts for quickly arriving at a diagnosis in many instances. This is referred to as intuitive inference. These scripts result from reasoning through patient problems repeatedly. Assisting with the development of illness scripts may occur as part of the PBL process, but is secondary to the development of clinical reasoning skills referred to as analytic inference. Cases which best foster clinical reasoning skills will lead students to a process that is: Deliberate, mindful Not instantaneous Less likely to be error-prone Based on science, causal relations, logic, probabilistic associations Such a process: Serves as a check and, if necessary, an override on intuitive responses Requires considerable cognitive work Creates models in working memory, maintains a coherent story This is achieved by drawing diagrams, forming hypotheses, testing hypotheses against new information, and seeking new knowledge and information. Cases need not include misleading information, but all cases should include a breadth of information such that students must consider whether and how it relates to the problem at hand. This tool will assist the case developer in considering the process for students and facilitators and in specifying the level of detail required for an optimal learning experience. For assistance or consultation contact Office of Educational Development (409) 772-2791 2/7/16 1 PBL Clinical Reasoning Scaffolding The following information should be specified as part of the case development process and should be part of the facilitator notes Active? Problem Potential Underlying Mechanisms In case development and in the PBL sessions, all problems should be listed and active problems discussed. A problem is any abnormal presentation (symptom), finding, or historical event (surgery etc). Problems should include a listing of established diagnoses (e.g. history of hypertension), but should not include possible diagnoses based on the current presenting problems. Students should be directed to consider basic science as the underlying mechanism for problems, thus the facilitator guide must outline the relevant points of such discussion. Active problems are those that might be related to the presenting complaint. These may be specified by putting a check mark in the Active column. Mechanism of the problem may be the anatomical, physiological, cellular process level explanation(s) for the problem. This should be a discussion of the basic science that underlies findings. Each problem may have multiple underlying mechanisms. This should be addressed for active problems. The level of mechanism to be included will relate to expectations expressed in the case learning objectives. Facilitators may need suggested probing questions to guide the discussion to the molecular level where appropriate. The construction of the problem list and discussion of underlying mechanisms should be a means of activating prior knowledge. Potential questions to be asked of students when putting the problem list on the board and discussing the mechanisms: Specific to this case: Which of the following might contribute to the presenting problem: Environmental factors Genetic background / family history Exposure to infectious agents Risk factors associated with lifestyle, previous illness, or previous treatment Medications or allergies Psychosocial issues For assistance or consultation contact Office of Educational Development (409) 772-2791 2/7/16 2 General: What physical structures might be involved in this problem? (bone, muscle, nerves, skin, organs) What mechanism would explain the patient’s complaint? (e.g., how does pain, swelling, cough, etc occur? ) Can you diagram the mechanism? Are there relationships among the problems? Describe / diagram the relationship. From relationships, generate hypotheses about patient problems (Differential Diagnoses).These may be broader than actual diagnoses at first. Students should first consider categories – infection, trauma, neoplasm, etc. And narrow those as their knowledge grows. Identify what information points to each hypothesis (confirming), information that is inconsistent with each hypothesis (disconfirming) and what the students want more information about (Evidence to seek). The following information should be specified as part of the case development process and should be part of the facilitator notes Hypothesis Confirming evidence Disconfirming evidence Evidence needed After discussing hypotheses and the evidence available, students should consider how they could obtain the evidence needed (question patient, physical exam, labs, diagnostic tests) For assistance or consultation contact Office of Educational Development (409) 772-2791 2/7/16 3 Differential Diagnoses Not all cases will include development of differential diagnoses. During the first and second years in our curriculum, the clinical knowledge base of students may be insufficient for this process. Learning the process of developing a diagnosis is more important that correctly identifying a single correct diagnosis. Three top Diagnoses and pertinent positives and negatives for each Pertinent positives – findings whose presence supports the diagnosis Pertinent negatives – findings whose absence supports the diagnosis (being afebrile could be a pertinent negative). Diagnosis 1. Pertinent positives Pertinent Negatives Family member Relevant to present illness 2. 3. Family History Diagnosis Social History Information Relationship to present case For assistance or consultation contact Office of Educational Development (409) 772-2791 2/7/16 4 Review of Systems Negative: Positive: Physical exam General: HEENT: Neck: Breasts: Heart: Lungs: Abdomen: Extremities: Pelvic exam: Other clinical Information: Lab vaules: Consider presentation format – lab reports of actual values? When possible lab reports should be in the format used in EPIC. Exhibits: Images: For assistance or consultation contact Office of Educational Development (409) 772-2791 2/7/16 5