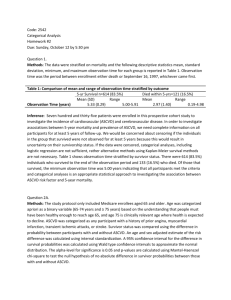
2193 BIOST 536 – HW#2 Excellent work! 124/140 Methods: We are
advertisement

2193 BIOST 536 – HW#2 Excellent work! 124/140 1. Methods: We are given observation time till either time of death or September 16, 1997, the end of the study. I created a binary outcome of having been observed alive till 5 years post-MRI or not. Subjects who died with an observation time of less than 5 years were considered to have experienced the outcome of interest, whereas those still alive at the end of the study and those who died after 5 years or more of observation were not considered to have experienced the outcome. There were no missing values for either observation time or death, so a 5-year mortality outcome could be calculated for all subjects. A single indicator for ASCVD was based on having had any diagnosis of CHD or stroke. There were also no missing values for either CHD or stroke, so all subjects had a value for ASCVD. With the 5-year mortality and ASCVD variables, I compared ASCVD status using the odds ratio comparing the odds of subjects with ASCVD dying within five years of their MRI to subjects without ASCVD. I calculated the probability of subjects with and without ASCVD dying within five years of their MRI using the sample proportions. A point estimate and 95% confidence interval for the ASCVD odds ratio were based on logistic regression of the binary 5-year mortality variable on a model including the variable indicating ASCVD status. The regression parameter for the ASCVD indicator provided the estimate of effect, and the confidence interval and p-value were computed assuming the regression parameter estimate was approximately normally distributed. Results: Of the 518 subjects without ASCVD, 53 (10.2%) died within five years of their MRI compared to 68 of 217 (31.3%) of subjects with ASCVD. Using the logistic regression model, subjects with ASCVD had a four-fold higher odds of dying within five years as compared to subjects without ASCVD (95% CI: 2.67-6.00). Based on a twosided p-value of <0.0001, I am led to reject the null hypothesis that 5-year mortality does not differ by ASCVD status. 2. Risk Difference a. Methods: I calculated the probability of subjects with and without ASCVD dying within five years of their MRI using the sample proportions and calculated a crude risk difference (RD). I stratified the association of ASCVD and 5-year mortality by sex and age. Age was categorized as 65-74-years-old or ≥75 yearsold. To obtain an overall measure of the association between ASCVD and 5-year mortality, the Mantel-Haenszel statistic weights were used for standardization to calculate an adjusted RD and 95% confidence interval (CI). Mantel-Haenszel weights were used, because selection had not occurred on either exposure or outcome, and the scientific question was one of etiology not public health intervention. Results: Of the 518 subjects without ASCVD, 53 (10.2%) died within five years of their MRI compared to 68 of 217 (31.3%) of subjects with ASCVD, yielding a crude RD of 21.1%. After adjusting for age and sex, subjects with ASCVD experienced an absolute increase of 19.1% in the probability of dying within five years. Based on a 95% CI, this result is consistent with the possibility that the true absolute increase lies between 8.09% and 30.1%. 2193 BIOST 536 – HW#2 b. Methods: I calculated the probability of subjects with and without ASCVD dying within five years of their MRI using the sample proportions and calculated a crude risk difference (RD). A point estimate and 95% CI for the difference in risk of death within five years were obtained from a linear regression of the binary 5year mortality indicator on a model including the ASCVD indicator, the binary sex indicator, and age as a continuous variable. The RD estimate came from the regression parameter for the ASCVD indicator. The CI was calculated using Wald inference of robust standard errors. Both the CI and p-value assumed the regression parameter estimates were approximately normally distributed. Results: Of the 518 subjects without ASCVD, 53 (10.2%) died within five years of their MRI compared to 68 of 217 (31.3%) of subjects with ASCVD, yielding a crude RD of 21.1%. After adjusting for age and sex using linear regression, subjects with ASCVD experienced an absolute increase of 18.9% in the probability of dying within five years. This result is consistent with a true absolute increase of 12.2% to 25.7%, and with a p-value of <0.0001, the null hypothesis of no difference in 5-year mortality by ASCVD status should be rejected. c. The stratified analysis inherently handles an interaction between ASCVD, sex, and/or age, whereas I would have needed to handle any presupposed effect modification explicitly in the linear regression. Stratum-specific RD estimates were approximately 10% lower for women than for men, by age group (15% and 11% for younger and older women, respectively, versus 26% and 22% for younger and older men, respectively), so there was some effect modification to be adjusted for. However, the regression allowed age to be modeled continuously, which entailed a smaller assumption than categorizing it. The overall results were very similar (18.9% vs. 19.1%), suggesting that influence of neither the effect modification nor the assumptions about modeling age was very great. 3. Odds Ratio a. Methods: I calculated the probability of subjects with and without ASCVD dying within five years of their MRI using the sample proportions and calculated a crude odds ratio (OR). I stratified the association of ASCVD and 5-year mortality by sex and age. Age was categorized as 65-74-years-old or ≥75 years-old. To obtain an overall measure of the association between ASCVD and 5-year mortality, the Mantel-Haenszel statistic weights were used for standardization to calculate an adjusted OR and 95% confidence interval (CI). Mantel-Haenszel weights were used, because selection had not occurred on either exposure or outcome, and the scientific question was one of etiology not public health intervention. A p-value for the null hypothesis that the OR equaled 1 was obtained using the Mantel-Haenszel Chi-square statistic. Results: Of the 518 subjects without ASCVD, 53 (10.2%) died within five years of their MRI compared to 68 of 217 (31.3%) of subjects with ASCVD, yielding a crude OR of 4.00. After adjusting for age and sex, subjects with ASCVD experienced a 3.44-fold higher odds of dying within five years (95% CI 2.285.18). The p-value for the Mantel-Haenszel statistic was <0.0001, supporting a 2193 BIOST 536 – HW#2 rejection of the null hypothesis that subjects have the same odds of dying within five years regardless of ASCVD, after adjusting for age and sex. b. Methods: I calculated the probability of subjects with and without ASCVD dying within five years of their MRI using the sample proportions and calculated a crude odds ratio (OR). A point estimate and 95% CI for the OR of death within five years were obtained from a logistic regression of the binary 5-year mortality indicator on a model including the ASCVD indicator, the binary sex indicator, and age as a continuous variable. The OR estimate came from the regression parameter for the ASCVD indicator. The CI was calculated using robust standard errors. Both the CI and p-value assumed the regression parameter estimates were approximately normally distributed. Results: Of the 518 subjects without ASCVD, 53 (10.2%) died within five years of their MRI compared to 68 of 217 (31.3%) of subjects with ASCVD, yielding a crude OR of 4.00. After adjusting for age and sex using logistic regression, subjects with ASCVD experienced a 3.57-fold higher odds of dying within five years (95% CI 2.36-5.40). With p<0.0001, the null hypothesis of no difference in 5-year mortality odds by ASCVD status should be rejected. c. The regression allowed age to be modeled continuously, which entailed a smaller assumption than categorizing it. The stratified analysis inherently handles an interaction between ASCVD, sex, and/or age, whereas I would have needed to handle any presupposed effect modification explicitly in the logistic regression. Although the confidence intervals for the stratum-specific estimates were large, older women had a much smaller point estimate OR than younger women (1.9 vs. 5.7). The OR for men 75 and over was slightly lower than for those 65-74, but the estimates were more similar than those for women (3.5 vs. 4.4). These point estimates suggest that there may have been important effect modification of the OR by age and sex. However, the overall results were very similar (3.44 vs. 3.57), suggesting that influence of neither the effect modification nor the assumptions about modeling age was very great. 4. Relative Risk a. Methods: I calculated the probability of subjects with and without ASCVD dying within five years of their MRI using the sample proportions and calculated a crude relative ratio (RR). I stratified the association of ASCVD and 5-year mortality by sex and age. Age was categorized as 65-74-years-old or ≥75 yearsold. To obtain an overall measure of the association between ASCVD and 5-year mortality, the Mantel-Haenszel statistic weights were used for standardization to calculate an adjusted RR and 95% confidence interval (CI). Mantel-Haenszel weights were used, because selection had not occurred on either exposure or outcome, and the scientific question was one of etiology not public health intervention. A p-value for the null hypothesis that the RR equaled 1 was obtained using the Mantel-Haenszel Chi-square statistic. Results: Of the 518 subjects without ASCVD, 53 (10.2%) died within five years of their MRI compared to 68 of 217 (31.3%) of subjects with ASCVD, yielding a crude RR of 3.06. After adjusting for age and sex, subjects with ASCVD had a 2193 BIOST 536 – HW#2 2.65-fold higher risk of dying within five years. This result is consistent with an increased risk of death within five years of 1.92- to 3.65-fold among those with ASCVD. The p-value for the Mantel-Haenszel statistic was <0.0001, supporting a rejection of the null hypothesis that subjects have the same risk of dying within five years regardless of ASCVD, after adjusting for age and sex. b. Methods: I calculated the probability of subjects with and without ASCVD dying within five years of their MRI using the sample proportions and calculated a crude relative ratio (RR). A point estimate and 95% CI for the RR of death within five years were obtained from a Poisson regression of the binary 5-year mortality indicator on a model including the ASCVD indicator, the binary sex indicator, and age as a continuous variable. The RR estimate came from the regression parameter for the ASCVD indicator. The CI was calculated using robust standard errors. Both the CI and p-value assumed the regression parameter estimates were approximately normally distributed. Results: Of the 518 subjects without ASCVD, 53 (10.2%) died within five years of their MRI compared to 68 of 217 (31.3%) of subjects with ASCVD, yielding a crude RR of 3.06. After adjusting for age and sex using Poisson regression, subjects with ASCVD had a 2.72-fold higher risk of dying within five years. This result is consistent with an increased risk of death within five years of 1.96- to 3.77-fold among those with ASCVD. With p<0.0001, the null hypothesis of no difference in 5-year mortality risk by ASCVD status should be rejected. c. The regression allowed age to be modeled continuously, which entailed a smaller assumption than categorizing it. The stratified analysis inherently handles an interaction between ASCVD, sex, and/or age, whereas I would have needed to handle any presupposed effect modification explicitly in the Poisson regression. As with the OR, older women had a much smaller point estimate RR than younger women (1.7 vs. 4.8). The RR for men 75 and over was slightly lower than for those 65-74, but the estimates were more similar than those for women (2.6 vs. 3.2). These point estimates suggest that there may have been important effect modification of the RR by age and sex. However, the overall results were very similar (2.65 vs. 2.72), suggesting that influence of neither the effect modification nor the assumptions about modeling age was very great. 5. All three approaches—calculating the RD, OR, and RR—can be done with either stratification or regression, and all can be adjusted for confounders or effect modifiers. The RD and RR are more directly interpretable than the OR. Because this was a cohort study with selection on neither ASCVD status nor outcome, and because the question was one of etiologic association not public health impact, I would opt for the relative risk. There is no necessity in using the OR because of the sample design, and the RR is more easily communicated to the lay population. The RR is also more consistent than the RD against changes in the exposure frequency in the population, which is important when comparing across studies as you do when attempting to determine an etiologic association. Were causality between ASCVD and 5-year mortality post-MRI among the elderly already established, the RD would have more benefit in comparing the impact of the association on the population. 2193 BIOST 536 – HW#2 6. Using the incidence ratio as a measure of association, provide inference for an association between incidence of colorectal cancer and birthplace, after adjustment for age, sex, and SEER.. Methods: I calculated the probability of subjects with and without ASCVD dying within five years of their MRI using the sample proportions and calculated a crude relative ratio (RR). A point estimate and 95% CI for the OR of death within five years were obtained from a Poisson regression of the binary 5-year mortality indicator on a model including the ASCVD indicator, the binary sex indicator, and age as a continuous variable. a. Methods: To assess the association between foreign or U.S. birthplace and colorectal cancer incidence using standardization, person-years were calculated for each birthplace-age-sex-SEER combination based on the 1980 census for each demographic group and the number of years each SEER center had been collecting data. The person-years for the U.S.-born subjects served as the standard population for the standardization. Incidence rates were then calculated for the U.S.- and foreign-born groups, a ratio taken, and confidence intervals computed. Results: U.S.-born subjects experienced 32.6 colorectal cases per 100,000 (95% CI 32.3-32.8) population, compared to 33.1 cases for foreign-born subjects (95% CI 32.1-34.3), after adjusting for age, sex, and SEER center. Foreign-born subjects had a 2% increased risk of colorectal cancer compared to those born in the U.S. (RR 1.02, 95% CI 1.00-1.03). This result is not statistically significant, so we cannot reject the null hypothesis that birthplace is not associated with colorectal cancer incidence. b. Methods: To assess the association between foreign or U.S. birthplace and colorectal cancer incidence using standardization, person-years were calculated for each birthplace-age-sex-SEER combination based on the 1980 census for each demographic group and the number of years each SEER center had been collecting data. A point estimate and 95% CI for the RR of colorectal cancer for foreign-born subjects were obtained from a Poisson regression of the binary cancer indicator on a model including an indicator for foreign-born, a binary sex indicator, age as an ordered categorical variable, SEER as a nominal categorical variable, and an offset for the person-years per 100,000 population. The RR estimate came from the regression parameter for the foreign-born indicator. Both the CI and p-value assumed the regression parameter estimates were approximately normally distributed. Results: U.S.-born subjects experienced 32.6 colorectal cases per 100,000 (95% CI 32.3-32.8) population, compared to 89.3 cases for foreign-born subjects (95% CI 32.1-34.3), not accounting for age, sex, and SEER center. After adjusting for age, sex, and SEER center using Poisson regression, foreign-born subjects experienced 0.95 times the colorectal cancer than did those born in the U.S. This was consistent with a true relative difference of 0.93- to 0.97-fold risk. A p-value <0.0001 leads me to reject the null hypothesis that birthplace and colorectal cancer are unassociated. However, given the minor reduction in risk for being foreign-born, it is questionable as to whether this difference is clinically meaningful. 2193 BIOST 536 – HW#2 c. Directly standardizing the rates inherently adjusted for any interactions between birthplace and/or the various covariates. There were certainly differences by category, but there were 324 combinations of the covariates and were difficult to assess without regression. If we were interested in how the effect of birthplace on colorectal cancer might be modified by age, sex, or center, we would need to use regression. The regression also took advantage of the ordered nature of the age categories, whereas the standardization did not draw any information from that. The estimates were both very close to 1, although in different directions. This may be accounted for by the regression’s modeling of age.