University of Huddersfield - The Association for Perioperative Practice
advertisement
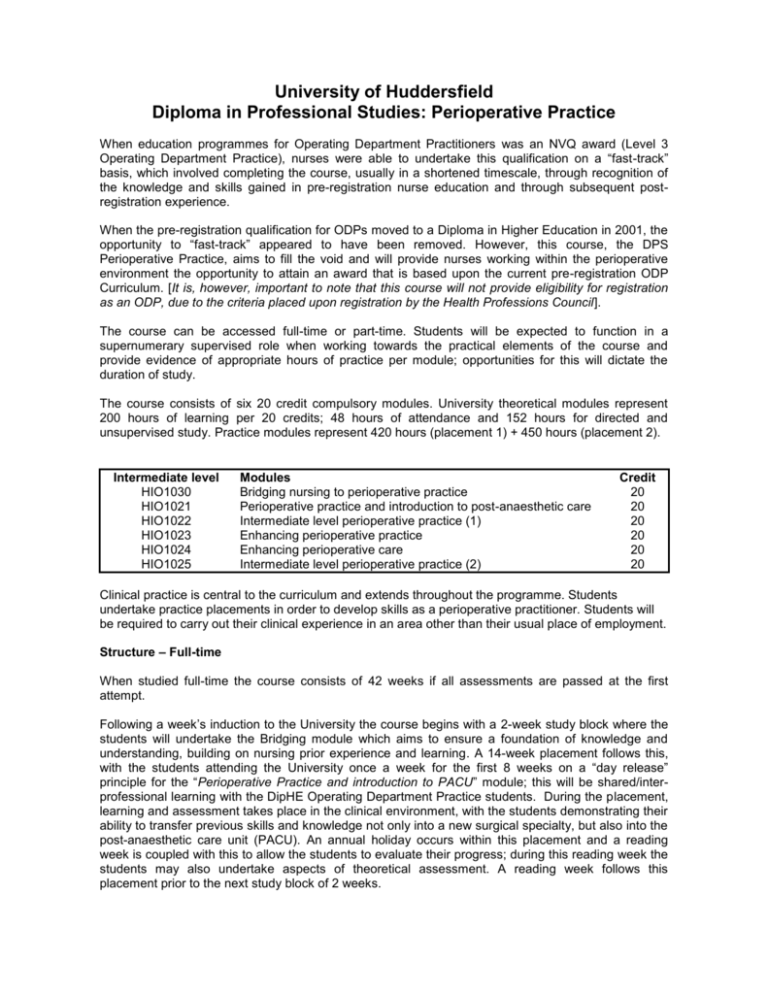
University of Huddersfield Diploma in Professional Studies: Perioperative Practice When education programmes for Operating Department Practitioners was an NVQ award (Level 3 Operating Department Practice), nurses were able to undertake this qualification on a “fast-track” basis, which involved completing the course, usually in a shortened timescale, through recognition of the knowledge and skills gained in pre-registration nurse education and through subsequent postregistration experience. When the pre-registration qualification for ODPs moved to a Diploma in Higher Education in 2001, the opportunity to “fast-track” appeared to have been removed. However, this course, the DPS Perioperative Practice, aims to fill the void and will provide nurses working within the perioperative environment the opportunity to attain an award that is based upon the current pre-registration ODP Curriculum. [It is, however, important to note that this course will not provide eligibility for registration as an ODP, due to the criteria placed upon registration by the Health Professions Council]. The course can be accessed full-time or part-time. Students will be expected to function in a supernumerary supervised role when working towards the practical elements of the course and provide evidence of appropriate hours of practice per module; opportunities for this will dictate the duration of study. The course consists of six 20 credit compulsory modules. University theoretical modules represent 200 hours of learning per 20 credits; 48 hours of attendance and 152 hours for directed and unsupervised study. Practice modules represent 420 hours (placement 1) + 450 hours (placement 2). Intermediate level HIO1030 HIO1021 HIO1022 HIO1023 HIO1024 HIO1025 Modules Bridging nursing to perioperative practice Perioperative practice and introduction to post-anaesthetic care Intermediate level perioperative practice (1) Enhancing perioperative practice Enhancing perioperative care Intermediate level perioperative practice (2) Credit 20 20 20 20 20 20 Clinical practice is central to the curriculum and extends throughout the programme. Students undertake practice placements in order to develop skills as a perioperative practitioner. Students will be required to carry out their clinical experience in an area other than their usual place of employment. Structure – Full-time When studied full-time the course consists of 42 weeks if all assessments are passed at the first attempt. Following a week’s induction to the University the course begins with a 2-week study block where the students will undertake the Bridging module which aims to ensure a foundation of knowledge and understanding, building on nursing prior experience and learning. A 14-week placement follows this, with the students attending the University once a week for the first 8 weeks on a “day release” principle for the “Perioperative Practice and introduction to PACU” module; this will be shared/interprofessional learning with the DipHE Operating Department Practice students. During the placement, learning and assessment takes place in the clinical environment, with the students demonstrating their ability to transfer previous skills and knowledge not only into a new surgical specialty, but also into the post-anaesthetic care unit (PACU). An annual holiday occurs within this placement and a reading week is coupled with this to allow the students to evaluate their progress; during this reading week the students may also undertake aspects of theoretical assessment. A reading week follows this placement prior to the next study block of 2 weeks. During this 2-week block the students are introduced to complicated and major interventions, how practice should be modified in response to individual patient needs, in response to changes in the clinical environment, and what is required in the effective co-ordination of the perioperative team and resources. It is expected that during the delivery of this content the students will have the opportunity to interact with healthcare users/patients in order to further develop the students’ understanding of the patient experience and the need to promote individualised care. A reading week follows this block. The modules are then further explored during the day release that the students attend at the University for the first 8 weeks of the next placement. The block and day release for these modules also involves shared/inter-professional learning with the DipHE Operating Department Practice students. Within this 15-week placement the students are required to demonstrate they are able to function as an autonomous practitioner (under supervision), and in doing so ensure the safe and efficient running of operating lists. Annual holidays and reading weeks are identified within the placement to provide the students with the opportunity and time to evaluate and reflect on their progress. If all assessments have been successfully achieved, the course ends at this point. Structure - Part-time When studied part-time the student negotiates their programme of learning with their personal tutor at the start of each year, ensuring they are not registering for tuition in more than 80 credits per year. The modules will be delivered for two intakes, September and March (excluding March 2008), which will enable part-time students to be flexible in their attendance over an extended period of study. For example, a student could undertake one theory module per intake over a 2-year period, whilst providing evidence of supervised practice in achieving each practice module. The maximum period of time over which credits can be accumulated towards this award is five years, in accordance with University regulations. Distance Learning Due to University constraints which require a minimum number of students to be enrolled for a traditional module to run, the course was designed to include the modules from the second year of the DipHE ODP course; this will ensure adequate student numbers as both DPS and DipHE students can study alongside each other, also promoting multidisciplinary and inter-professional learning. However, the Bridging module is a stand-alone requirement of the DPS and the module may not be able to run if there is insufficient uptake. For this reason, it is intended to review the module delivery method and provide it using a blended strategy incorporating both traditional and electronic resources that will promote distance learning. This mode of delivery will not, however, be available until mid2008, which may mean that the DPS will not be available until then if there are insufficient numbers of applicants for September 2007. Criteria for Admission Applicants for this course will be expected to: hold current registration with the NMC in the appropriate section of the register. be employed in a NHS or Independent sector hospital that has an appropriate range of available clinical experiences and the support networks necessary for teaching and assessment in practice. have management support for undertaking the course Further Details Steven Brown –Admissions Tutor 01484 473284 – odpadmissions@hud.ac.uk ODP Secretary - 01484 473530 - odpsec@hud.ac.uk