Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL
advertisement

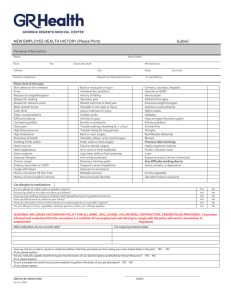
Version 1.2, 1st April, 2014 TO BE PRINTED ON LOCAL TRUST HEADED PAPER The BASIL-2 Trial: Bypass vs. Angioplasty in Severe Ischaemia of the Leg Chief Investigator: Professor Andrew Bradbury PARTICIPANT INFORMATION SHEET We would like to invite you to take part in a research study called BASIL-2. Before you decide, we would like you to understand why the research is being done and what it would involve for you. Please take time to read the following information carefully. A member of our research team will go through this information sheet with you and answer any questions you have. Please do ask us if there is anything that is not clear or if you would like more information. Talk to others about the study if you wish; and take your time to decide whether or not you wish to take part. Part 1 tells you the purpose of this study and what will happen to you if you take part Part 2 gives you more detailed information about the conduct of the study Part 1 What is the problem with your leg? The problems you are having with your leg are due to a severe lack of blood supply, a condition known as ‘severe limb ischaemia’. Your consultants believe that unless they can get more blood into your leg it is likely that your condition will deteriorate to a point where your leg, even your life, is in danger. What treatments are available to try to improve your leg? There are two ways of getting more blood into your leg; these are: Bypass surgery: this involves an operation to bypass the blocked / narrowed arteries Angioplasty / stenting: this involves inflating a balloon inside the blocked / narrowed arteries so forcing it open (angioplasty). Sometimes it is necessary to put a small metal tube into the artery to hold it open (stenting) How do we know which is the best treatment for your leg? We don’t, which is why we are doing this study. Although bypass surgery and angioplasty / stenting are both well-established methods for treating your condition, and have been used previously in many thousands of patients around the world for many years, nobody knows which of the two treatments works best for patients like you. The potential advantages of angioplasty/stenting over bypass are that it may be safer in the short term and that you may be able to go home sooner afterwards. Page 1 of 13 Version 1.2, 1st April, 2014 The potential disadvantages of angioplasty/stenting compared with bypass are that it may not work as well as surgery. This may mean that the angioplasty/stenting has to be repeated or that you may have to go on to have a bypass operation in any case. So, there are pros and cons of both treatments in terms of success and safety and which is best for patients like you is unknown. More information about these procedures is provided below. What is the purpose of the study you are being invited to take part in? Your doctors believe that they could treat your leg either by bypass surgery or angioplasty / stenting - but they don’t know which treatment is likely to be most successful and so which one to try first. You are being invited to take part in this study so that we can answer that question and so have a better idea of how to treat patients like you in the future. Can I pick which treatment I receive (i.e. whether I have bypass surgery or angioplasty/stenting)? No. To make sure that we get a true answer from the study we have to ensure that the results will not be biased in any way. In order to achieve this we have to be sure that there is a 50:50 chance of you being treated by either surgery or angioplasty/stenting in the first instance. In order to do this, a computer will randomly allocate you to one or other treatment first. You can think of it a bit like tossing a coin: Heads - your consultant will try surgery first Tails - your consultant will try angioplasty / stenting first This is essential so that a fair comparison can be made between the two groups. Dividing people into treatment groups in this way is what is called a ‘randomised clinical trial’ and is the standard and most reliable way of comparing different treatment options. If, for whatever reason, the treatment you are allocated to first doesn’t work then your consultants will still be able to go on and try the other treatment if they think that is in your best interests. How many patients will be taking part in this study? In order to get a meaningful result from the study approximately 600 patients recruited from many hospitals across the UK will be taking part. What are the pros and cons of taking part? Page 2 of 13 Version 1.2, 1st April, 2014 Any treatment of the arteries, either by surgery or angioplasty/stenting, carries some risk and these are described in detail below. However, what your consultants are quite certain about is that the risks of not improving the blood supply to your leg in terms of you losing your leg, even your life, are far higher than the risks of intervention whether that is by means of bypass surgery or angioplasty/stenting. Whether you take part in this study or not, in order to help make your leg better, you will require: blood tests, probably on repeated occasions to take medicines to thin your blood and reduce your cholesterol and blood pressure scans and X-rays of your blood vessels a procedure, either bypass surgery or angioplasty/stenting, to improve the circulation to your leg to attend hospital afterwards for regular check-ups, probably for the rest of your life Your consultants believe that they could treat you either by surgery or angioplasty / stenting but they don’t know which is best for you. If you go in to the trial, whether you have surgery or angioplasty/stenting will be decided by a ‘toss of the coin’ as described above. If you choose not to go in to the trial, your consultants will either suggest bypass surgery or angioplasty / stenting based on their medical judgement as which will be best for you. Although entering the trial may not necessarily help you, the information gathered from this study will help doctors with their medical judgement and so better treatments for patients in the future. Your doctors and nurses will be able to discuss with you in detail the pros and cons of entering the study in relation to your particular condition and answer all of your questions. However, you should be reassured that both of the treatments (bypass surgery or angioplasty / stenting) that you might receive, whether you are in the study or not, are currently used to treat patients with your condition in the UK and in many other countries around the world and are not experimental. What are the risks of angioplasty / stenting? Angioplasty / stenting is usually performed under local anaesthetic with you awake in an Xray room or an operating theatre. The potential risks of angioplasty / stenting can be divided into the following categories: Related to arterial puncture site (usually in the groin): Bruising, this is inevitable but usually goes away in a few weeks Pain, this is inevitable but it is not usually severe and can be well controlled with pain killers Page 3 of 13 Version 1.2, 1st April, 2014 Bleeding, again this is inevitable but it is usually fairly minimal and stops of its own accord Rarely (1%) significant bleeding at the puncture site can require an emergency operation to repair the damaged artery Related to the contrast (the dye put into your arteries so that they can be seen by X-rays): Some patients experience an allergic reaction to the X-ray contrast. In most cases this is minor but rarely the reaction may be severe and require urgent treatment with medicines. Very rarely it can be fatal. The x-ray contrast can, in some patients, affect kidney function. If you are likely to be at risk of this, special precautions will be taken to reduce the chances of this problem occurring. Rarely, damage from the contrast can lead to the patient being put on a kidney machine (for dialysis). This is usually temporary but very rarely can be permanent. In patients with diabetes, the contrast can also upset their diabetic control. This can usually be prevented or managed by altering their diabetic tablets. Sometimes (for patients not on insulin already) it means going on to insulin; this is usually temporary but rarely can be permanent. Related to the treatment: The procedure may not work because the diseased arteries cannot be opened up with balloons and stents. In previous similar studies, this has occurred in up to 1020% of patients. We do not know how often this will happen in this study but the risks may be similar. If the procedure fails, your consultants may suggest having another go at angioplasty / stenting on a different day, or they may suggest going on to have bypass surgery instead. In previous similar studies, patients who have had to have bypass surgery after failed angioplasty / stenting have tended to do less well than those who have been treated with bypass surgery in the first instance. We do not know if that will be the case in this study. Rarely, the angioplasty/ stenting procedure can lead to a worsening of the blood supply to the leg so that emergency surgery is required to prevent amputation. Rarely, the angioplasty/ stenting procedure can lead to the blocked / narrowed artery bursting. This can sometimes be treated in the x-ray department by putting in a special stent with a covering around it (a stent-graft). If this is not possible, an emergency operation may be required to repair the artery. Rarely, small fragments from the lining of the blocked / narrowed artery can break off and lodge in an artery further down the leg (distal embolisation). This may also require an operation to ‘fish out’ the fragments if they are causing a problem with the blood flow. Page 4 of 13 Version 1.2, 1st April, 2014 What are the risks of bypass surgery? The potential risks of bypass surgery can be divided into the following categories. Related to anaesthetic: Bypass surgery is usually performed with you asleep under general anaesthesia although sometimes it is performed with you awake with the lower half of your body numbed by an injection in your back (epidural or spinal anaesthesia). These days such anaesthetics are very safe but the following problems can occur: Nausea and vomiting, this is quite common but is usually well controlled by tablets or injections Rarely, there can be damage to teeth / dentures from the tube put down your throat to help you breathe Rarely, lung problems can occur such as pneumonia or a collapsed lung Muscle aches and pain can occur but usually get better in a few days of their own accord Confusion, this is uncommon and usually clears in a few days of its own accord Related to the surgery itself: Rarely, the procedure may not work or fail soon after the operation. Wounds problems can occur such as poor healing, bruising, bleeding and infection; in most cases these respond to good nursing care and antibiotics; rarely further surgery is required. As with any surgical procedure, you will feel somewhat tired afterwards and have some pain along the incisions; however, the pain is usually well controlled with tablets or injections. What are the risks shared by angioplasty / stenting and bypass surgery? Many patients with severe limb ischaemia also have other significant health problems such as diabetes, heart and lung disease. For this reason, even if the procedures go well, there are some complications that can occur both after bypass surgery and angioplasty / stenting. Each of these individual complications is quite uncommon but taken together the overall risk is probably in the region of 5-10%. These complications include: Stroke Heart attack Pneumonia Kidney failure, possibly requiring dialysis which, rarely, can be permanent Page 5 of 13 Version 1.2, 1st April, 2014 Bowel problems such as constipation and diarrhoea; these usually settle of their own accord, or with tablets or injections Blood clots in the leg (deep vein thrombosis, DVT) and lung (pulmonary embolus, PE); these would require treatment with blood-thinning injections and then tablets Participating in this study will involve either angioplasty and stenting, or angiography after surgery. You would receive one or other of these procedures as normal clinical care anyway, but in this study this choice is randomised, rather than your clinician making the decision. There is a risk from any exposure to ionising radiation, however small, that it may cause a cancer many years later. The x-ray dose from an angiogram is equivalent to approximately 13 months of average natural background radiation. You would receive this as a minimum x-ray exposure, even if you do not participate in this study. If you are randomised to receive Angioplasty +/- stenting, you will receive about an additional 14 months of average natural background radiation, bringing the total to 27 months. The Health Protection Agency (now Public Health England) Radiation Protection Division describe a radiation exposure equivalent to a few years average natural background radiation as ‘Low Risk’. Your doctors will be able to discuss the nature and level of these risks to you in more detail in relation to your particular health problems. However, your doctors feel that one or other of these treatments is necessary for you (whether you are in the trial or not) in order to prevent your leg getting worse to a point where you might require an amputation, or the condition may even become life-threatening. If I enter the trial will I need extra visits to hospital or treatment? No. Whether you enter the trial or not, your doctors will either advise surgery or angioplasty / stenting for your leg, and because of that they will want to see you back in hospital on a regular basis, probably for the rest of your life. At these visits your doctors will ask you how you are getting on; they will examine you, and may advise additional tests or procedures. If you enter the trial you will also receive this same high level of aftercare and will be seen by a research nurse 1, 3, and 6, 9, 12, 18, 24, and 36 months after your treatment; and inbetween and thereafter as your consultant feels is necessary. Do you have to enter this study? No, you do not have to enter this study. Taking part in research is always voluntary. The purpose of this document is to invite you to take part in the study and to provide some information to help you make up your mind. Your participation in this study is entirely voluntary and you may decline to take part, or withdraw from the study, at any time, without giving a reason and without your further care being affected in any way. Page 6 of 13 Version 1.2, 1st April, 2014 What will happen to me if I take part? If you agree to take part in BASIL-2 we will go through the study information with you again, giving you the chance to ask any questions. You will need to sign a Consent Form if you agree to take part. You should only sign the Consent Form if you understand the study and you are sure that you want to take part. Your details will then be passed to the BASIL-2 trial office at the University of Birmingham. You will be asked about your health (which will include a review of your previous medical history) and the medications that you are taking. We will record any history of previous vascular (blood vessel) interventions, your mobility status and perform an examination of your legs. You will also be asked to complete a short questionnaire about your quality of life before you have your treatment, as well as further questionnaires at 1, 3, and 6, 9, 12, 18, 24, 30 and 36 months after your treatment. As explained, above, most of the treatment you will receive will be the same whether you were in the study or not. There are no extra blood tests required beyond your normal care and there are no additional clinic visits. The BASIL-2 study was set-up to reflect the normal visit timetable of patients completing either of the study treatments. Whether you enter the study or not, your doctors will advise either bypass surgery or angioplasty/stenting for your leg, and because of this they will want to see you again every few months in their clinic, probably for the rest of your life. At these visits your doctors will ask you how you are getting on; they will examine you, and may advise additional tests or procedures. If you enter the study you will also receive this same high level of aftercare and will be seen by a research nurse 1, 3 and 6, 9, 12, 18, 24, 30 and 36 months after your treatment and thereafter as your consultant feels is necessary. You should also keep all of your other doctor appointments. We will ask you at each visit how many other doctor appointments you have had since the previous visit. During the study visits you will be asked questions about your health and questions about the cost of expenses related to your severe limb ischaemia. Will you be given the opportunity to say how successful you think the treatment has been? Yes, definitely. As part of the study we will ask you to fill in simple questionnaires before and after your treatment to find out how you feel about your general state of health and about your leg. In this way we can judge the relative success of the two treatments not only from the doctors’ point of view but also, more importantly, from the point of view of the patients undergoing the treatment now and in the future. What happens if you are unhappy with your treatment? Page 7 of 13 Version 1.2, 1st April, 2014 Entering this study does not affect your normal rights in any way. If you have a grievance against one of your doctors, or against the hospital, as a result of your treatment then you will be able to pursue your complaint in exactly the same way as you would normally do. Will I get paid if I take part? No. We are unable to pay you for participating; we do not expect your travel expenses to differ from those that would normally be incurred by you for your standard routine hospital visits outside of this study. What are the alternatives for taking part in the study? As explained above, if you choose not to go in to the trial, your consultants will either suggest bypass surgery or angioplasty / stenting based on their medical judgement as which will be best for you. There are no other effective treatments for your leg condition. Who will know you are in this study? Your hospital doctors and your General Practitioner will know that you are in this study. As is normal practice, all your medical and hospital records will be kept confidential although the doctors conducting the study will have access to the information contained within them. We would like to follow your progress after treatment for up to five years and would, therefore, ask your permission for the doctors conducting the study to have continued access to your health records even after your final visit to the clinic. All the results of the study will be treated confidentially and will be published for the benefit of other doctors and patients in such a way as to make it impossible for anyone to identify the individual patients taking part. Which organisation is running the study? This study is being conducted in hospitals across the UK and is being co-ordinated by the Birmingham Clinical Trials Unit (BCTU) at the University of Birmingham. The trial is being funded by a government body called the National Institute of Health Research (NIHR) Health Technology Assessment (HTA) programme. If I have any questions, who can I ask? Your own hospital doctors, your research nurse or your General Practitioner should be able to answer any questions you may have. How long do I have to decide? Page 8 of 13 Version 1.2, 1st April, 2014 There is no pressure on you to decide quickly or before you are ready. However, because of the problems you are having with your leg, your doctors will want to get on and treat your leg fairly quickly whether or not you are in the trial. If the information in Part 1 has interested you and you are considering participation, please read the additional information in Part 2 before making any decision. Page 9 of 13 Version 1.2, 1st April, 2014 Part 2 What if relevant new information becomes available? Sometimes we get new information about the treatment being studied. If this happens your research doctor will tell you and discuss whether you should continue in the study. If this new information means that we should stop the study, or change how we are running it, we will do this and make sure that you are offered the best treatment. What will happen if I don’t want to carry on with the study? You are free to withdraw from the study at any time and this will not affect your care. You can either withdraw completely or choose to keep in contact with us to let us know your progress. Information collected earlier in the study will still be used for study purposes. What if something goes wrong? If you have a concern about any aspect of this study, you should ask to speak to the researcher who will do their best to answer your questions <insert Local PI contact details here>. We do not anticipate that anything will go wrong and we will of course take great care that nothing goes wrong but if you are harmed by taking part in this research you should understand that there are no special compensation arrangements. If you are harmed due to someone’s negligence, then you may have grounds for a legal action but you may have to pay for it. Regardless of this, if you wish to complain, or have any concerns about any aspect of the way you have been approached or treated during the course of this study, the normal National Health Service complaints mechanisms are available to you: ask to speak to the complaints manager of the hospital. If you remain unhappy and wish to complain formally you can contact your local Patient Advice and Liaison Services (PALS) group or local equivalent group <insert name and contact details>. Taking part in the study would not affect your legal rights. Will my taking part in the study be kept confidential? Yes. If you decide to take part in BASIL-2, all information collected about you during the course of the study will be kept strictly confidential in the same way as all of your other medical records. Information about you, your disease and progress will be sent by your doctors to the BASIL-2 Study Office at the University of Birmingham Clinical Trials Unit (BCTU), on paper and electronically, where it will be securely stored under the provisions of the 1998 Data Protection Act. This will include a signed copy of your Consent Form. Your name and address will also be given to dedicated staff at the BCTU when you first enter the study, in Page 10 of 13 Version 1.2, 1st April, 2014 case we need to send Quality of Life questionnaires to your home address. As we may contact you by post or telephone to ask you to complete questionnaires asking about your progress, we will ask you to give us your permission to do so. Your GP, and the other doctors involved in your clinical care, will be notified of your participation in the study and kept informed of your progress. Also, if you consent; the research staff involved in BASIL-2 may access electronic data from your central NHS records. This will provide researchers with information that is routinely gathered and stored during your visits to primary care and hospital, and will allow researchers to find out about your health after the trial has ended and the long-term effects of the treatments. By using routinely collected data we will be able to do this without needing to contact you further. In order to do this, we would need to send your name, gender, date of birth and NHS number with any request for information. As with the main study data we would store this personal data on a secure, password-controlled database with access given to only a small number of delegated study staff. This information will be strictly confidential and all medical details will be anonymised to everyone except the core staff involved in this trial. All will have a duty of confidentiality to you as a research participant and will do their best to meet this duty. With your permission, your relevant medical records may be inspected by authorised individuals from the BCTU. The purpose of this is to check that the study is being carried out correctly. All those associated with the study will have a duty of confidentiality to you as a research participant. In line with Good Clinical Practice, at the end of the study, the data will need to be securely archived (stored) for at least 5 years (but ideally not less than 25 years). Arrangements for confidential destruction will then be made. Should you withdraw consent at any time for your data to be collected, no further data will be collected from that point onwards. Data already collected prior to withdrawal may still be used in the trial analysis. Will my GP be told that I am in a study? Yes, we will inform your GP of your involvement in the study. Will any genetic tests be done? No genetic tests will be performed. What will happen to the results of the study? Once BASIL-2 has finished we will publish the results in international, peer-reviewed scientific journals so that others can benefit. We will also publicise the results on the study’s website. No individual patients will be identified in any publications or reports. Page 11 of 13 Version 1.2, 1st April, 2014 Which organisation is running and funding the study? This study is being conducted in hospitals across England and Scotland. The study is sponsored by the University of Birmingham and is being coordinated by the Birmingham Clinical Trials Unit (BCTU) at the University of Birmingham. The study is being funded by a government body called the National Institute of Health Research (NIHR) Health Technology Assessment (HTA) programme. The research doctors will not receive a payment for including you in this study. Who has reviewed the study? All research in the NHS is reviewed by an independent group of people called a Research Ethics Committee to ensure your safety, rights, wellbeing and dignity. This study has been reviewed by the <insert name> Research Ethics Committee. Further information and contact details: We will be pleased to answer any questions you may have or clarify things you do not understand. You can contact the BASIL-2 team on <insert contact details>. If you wish to discuss the study with a doctor who is not directly involved with the study you may contact Dr <insert name and contact details>. Thank you for taking the time to read this Participant Information Sheet Can I keep a copy of this Information sheet? Yes. Please feel free to keep this document. If you decide to take part in the study then you will be asked to sign a consent form and you will also be given a copy of that to keep. YOUR SURGEONS NAME IS: THE CONTACT TELEPHONE NUMBER IS: Page 12 of 13 Version 1.2, 1st April, 2014 (BASIL 2) Trial Flow Diagram Patient with severe limb ischaemia due to lack of blood supply to the leg. A screening consent form for medical records is discussed and signed. Diagnostic imaging is performed and reviewed by a team of consultants to ensure that both vein bypass to, and angioplasty / stenting of, arteries below the knee are options for the patient. Informed consent for the trial is completed. Baseline assessments including medical history, completion of a physical examination, and assessment of the legs. Randomisation Vein bypass Follow-up visits completed at 1, 3, 6, 9, 12, 18, 24, 30 and 36 months. Page 13 of 13 Angioplasty / stenting