Cystosarcoma Phyllodes - Dis Lair
advertisement
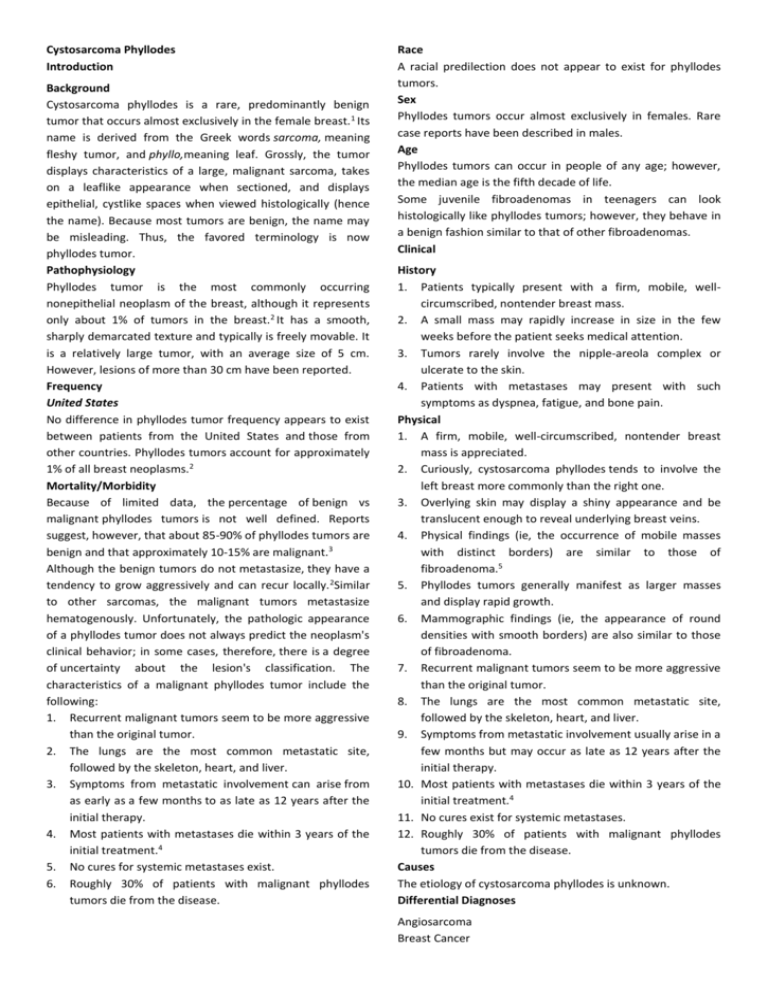
Cystosarcoma Phyllodes Introduction Background Cystosarcoma phyllodes is a rare, predominantly benign tumor that occurs almost exclusively in the female breast. 1 Its name is derived from the Greek words sarcoma, meaning fleshy tumor, and phyllo,meaning leaf. Grossly, the tumor displays characteristics of a large, malignant sarcoma, takes on a leaflike appearance when sectioned, and displays epithelial, cystlike spaces when viewed histologically (hence the name). Because most tumors are benign, the name may be misleading. Thus, the favored terminology is now phyllodes tumor. Pathophysiology Phyllodes tumor is the most commonly occurring nonepithelial neoplasm of the breast, although it represents only about 1% of tumors in the breast.2 It has a smooth, sharply demarcated texture and typically is freely movable. It is a relatively large tumor, with an average size of 5 cm. However, lesions of more than 30 cm have been reported. Frequency United States No difference in phyllodes tumor frequency appears to exist between patients from the United States and those from other countries. Phyllodes tumors account for approximately 1% of all breast neoplasms.2 Mortality/Morbidity Because of limited data, the percentage of benign vs malignant phyllodes tumors is not well defined. Reports suggest, however, that about 85-90% of phyllodes tumors are benign and that approximately 10-15% are malignant.3 Although the benign tumors do not metastasize, they have a tendency to grow aggressively and can recur locally. 2Similar to other sarcomas, the malignant tumors metastasize hematogenously. Unfortunately, the pathologic appearance of a phyllodes tumor does not always predict the neoplasm's clinical behavior; in some cases, therefore, there is a degree of uncertainty about the lesion's classification. The characteristics of a malignant phyllodes tumor include the following: 1. Recurrent malignant tumors seem to be more aggressive than the original tumor. 2. The lungs are the most common metastatic site, followed by the skeleton, heart, and liver. 3. Symptoms from metastatic involvement can arise from as early as a few months to as late as 12 years after the initial therapy. 4. Most patients with metastases die within 3 years of the initial treatment.4 5. No cures for systemic metastases exist. 6. Roughly 30% of patients with malignant phyllodes tumors die from the disease. Race A racial predilection does not appear to exist for phyllodes tumors. Sex Phyllodes tumors occur almost exclusively in females. Rare case reports have been described in males. Age Phyllodes tumors can occur in people of any age; however, the median age is the fifth decade of life. Some juvenile fibroadenomas in teenagers can look histologically like phyllodes tumors; however, they behave in a benign fashion similar to that of other fibroadenomas. Clinical History 1. Patients typically present with a firm, mobile, wellcircumscribed, nontender breast mass. 2. A small mass may rapidly increase in size in the few weeks before the patient seeks medical attention. 3. Tumors rarely involve the nipple-areola complex or ulcerate to the skin. 4. Patients with metastases may present with such symptoms as dyspnea, fatigue, and bone pain. Physical 1. A firm, mobile, well-circumscribed, nontender breast mass is appreciated. 2. Curiously, cystosarcoma phyllodes tends to involve the left breast more commonly than the right one. 3. Overlying skin may display a shiny appearance and be translucent enough to reveal underlying breast veins. 4. Physical findings (ie, the occurrence of mobile masses with distinct borders) are similar to those of fibroadenoma.5 5. Phyllodes tumors generally manifest as larger masses and display rapid growth. 6. Mammographic findings (ie, the appearance of round densities with smooth borders) are also similar to those of fibroadenoma. 7. Recurrent malignant tumors seem to be more aggressive than the original tumor. 8. The lungs are the most common metastatic site, followed by the skeleton, heart, and liver. 9. Symptoms from metastatic involvement usually arise in a few months but may occur as late as 12 years after the initial therapy. 10. Most patients with metastases die within 3 years of the initial treatment.4 11. No cures exist for systemic metastases. 12. Roughly 30% of patients with malignant phyllodes tumors die from the disease. Causes The etiology of cystosarcoma phyllodes is unknown. Differential Diagnoses Angiosarcoma Breast Cancer Other Problems to Be Considered Juvenile fibroadenoma Giant fibroadenoma Inflammatory carcinoma Sclerosing adenosis Radial scar Fat necrosis Fibrocystic change Breast abscess Adenocarcinoma Mastitis Workup Laboratory Studies No specific hematologic tumor markers or other blood tests can be used to diagnose cystosarcoma phyllodes. Imaging Studies Although mammography and ultrasonography generally are important in the diagnosis of breast lesions, they are notoriously unreliable in differentiating benign cystosarcoma phyllodes (CSP) from the malignant form of the condition or from fibroadenomas. Thus, findings on imaging studies are not definitively diagnostic of CSP.6 Procedures 1. Fine-needle aspiration for cytologic examination usually is inadequate for the diagnosis of phyllodes tumors.Core biopsy is more reliable, but there still can be sampling errors and difficulty in distinguishing the lesion from a fibroadenoma. 2. Open excisional breast biopsy for smaller lesions or incisional biopsy for large lesions is the definitive method for diagnosing phyllodes tumors. Histologic Findings All phyllodes tumors contain a stromal component that can vary significantly in histologic appearance from one lesion to another. In general, benign phyllodes tumors demonstrate a markedly increased number of regular fusiform fibroblasts in the stroma. Occasionally, highly anaplastic cells with myxoid changes are observed. A high degree of cellular atypia, with increased stromal cellularity and an increased mitotic count, is almost always observed in the malignant form of cystosarcoma phyllodes. Ultrastructurally, in the benign and malignant forms of phyllodes tumors, nucleoli may reveal a coarsely meshed nucleolonema and abundant cisternae in the endoplasmic reticulum. Treatment Surgical Care In most cases of cystosarcoma phyllodes, perform wide local excision, with a rim of normal tissue. 7,8,9 No absolute rules on margin size exist. However, a 2 cm margin for small (<5 cm) tumors and a 5 cm margin for large (>5 cm) tumors have been advocated. The lesion should not be "shelled out," as might be done with a fibroadenoma, or the recurrence rate will be unacceptably high.4 1. If the tumor to breast ratio is sufficiently high to preclude a satisfactory cosmetic result by segmental excision, total mastectomy, with or without reconstruction, is an alternative. 2. More radical procedures are not generally warranted.8 3. Perform axillary lymph node dissection only for clinically suspicious nodes. However, virtually all of these nodes are reactive and do not contain malignant cells. 10 Consultations Consult a general surgery specialist. Medication There is no proven role for adjuvant chemotherapy or radiation therapy in the treatment of phyllodes tumors. Response to chemotherapy and radiotherapy for recurrences and metastases has been poor, and no success with hormonal manipulation has been documented. Follow-up Further Outpatient Care 1. Although specific guidelines regarding follow-up care for phyllodes tumors are limited because of the rarity of these lesions, regular, long-term follow-up care should be performed to detect possible local recurrences. 2. An initial visit 1-2 weeks after surgery to detect any initial complications should be followed by periodic visits as determined by the patient's surgeon. A reasonable schedule might be physical examinations every 6 months and mammograms yearly for at least 5 years (seeComplications). 3. Carefully observe patients for any possible recurrence. Complications As with most breast surgery, postoperative complications from the surgical treatment of phyllodes tumors include the following: o Infection o Seroma formation o Local and/or distant recurrence Prognosis 1. Although cystosarcoma phyllodes is considered to be a clinically benign tumor, the possibility for local recurrence following excision always exists, particularly with lesions that display malignant histology.9,11Tumors that, after initial treatment by wide local excision, recur locally should ideally be treated with total mastectomy. 2. Metastatic disease is typically observed in the lung, mediastinum, and skeleton. 3. The clinical course is variable. o If the tumor is benign, the long-term prognosis is excellent following adequate local excision. o If the tumor recurs locally after excision, further local excision or total mastectomy is typically curative.