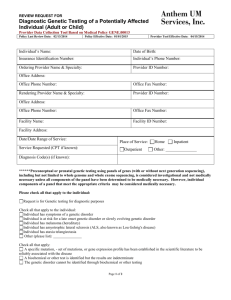
Highmark Requirements
advertisement

SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 1 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: POLICY: Genetic Testing is required to be scheduled prior to patients presenting to the laboratory for collection. This process will allow the scheduler to obtain the prior pre-authorization if needed from the ordering provider. Genetic testing is typically an expensive test and many insurance companies require pre-authorization prior to performing. The physician ordering the test is required to obtain the authorization number from the insurance company or meet the requirements for medical necessity if no authorization is needed. The patient cannot have the testing performed without the information provided above. If the patient presents without the information the ordering physician will be contacted to provide the authorization or asked to complete an Advanced Beneficiary Notice (ABN) form. The signed ABN holds the patient responsible for charges if the insurance does not cover the testing. The following insurances and requirements are included in this policy: Highmark UPMC Cigna Aetna Gateway Medicare FirstCare PPO HealthAmerica Coventry Types of Genetic Testing: Newborn Screening Newborn screening is used just after birth to identify genetic disorders that can be treated early in life. Diagnostic Testing Diagnostic testing is used to identify or rule out a specific genetic or chromosomal condition. In many cases, genetic testing is used to confirm a diagnosis when a particular condition is suspected based on physical signs and symptoms. Diagnostic testing can be performed before birth or at any time during a person’s life. SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 2 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Carrier Testing Carrier testing is used to identify people who carry one copy of a gene mutation that, when present in two copies, causes a genetic disorder. This type of testing is offered to individuals who have a family history of a genetic disorder and to people of certain ethnic groups with an increased risk of specific genetic conditions. Prenatal testing Prenatal testing is used to detect changes in the fetus’s genes or chromosomes before birth. This type of testing is offered during pregnancy if there is an increased risk that the baby will have a genetic or chromosomal disorder. In some cases, prenatal testing can lessen a couple’s uncertainty or help them make decisions about a pregnancy. Currently Available DNA-Based Gene Tests: Alpha-1-antitrypsin deficiency (AAT; emphysema and liver disease) Amyotrophic lateral sclerosis (ALS; Lou Gehrig’s Disease; progressive motor function loss leading to paralysis and death) Alzheimer’s disease (APOE; late-onset variety of senile dementia) Ataxia telangiectasia (AT; progressive brain disorder resulting in loss of muscle control and cancers) Gaucher disease (GD; enlarged liver and spleen, bone degeneration) Inherited breast or ovarian cancer (BRCA1/BRCA2; early onset tumors of breasts and ovaries) Hereditary nonpolyposis colon cancer (CA; early-onset tumors of colon and sometimes other organs) Central core disease (CCD; mild to severe muscle weakness) Charcot-Marie-Tooth (CMT; loss of feeling in ends of limbs) Congenital adrenal hyperplasia (CAH; hormone deficiency; ambiguous genitalia and male pseudohermaphroditism) Cystic fibrosis (CF; disease of lung and pancreas resulting in thick mucous accumulations and chronic infections) Duchenne muscular dystrophy/Becker muscular dystrophy (DMD, sever to mild muscle wasting, deterioration, weakness) Dystonia (DYT; muscle rigidity; repetitive twisting movements) Emanuel syndrome (severe mental retardation, abnormal development of the head, heart and kidney problem) Fanconi anemia, group C (FA; anemia, leukemia, skeletal deformities) Factor V Leiden (FVL; blood-clotting disorder) Fragile X Syndrome (FRAX; leading cause of inherited mental retardation) SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 3 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Galactosemia (GALT; metabolic disorder affects ability to metabolize galactose) Hemophilia A and B (HEMA and HEMB; bleeding disorders) Hereditary hemochromatosis (HFE; excess iron storage disorder) Huntington’s disease (HD, usually midlife onset; progressive, lethal, degenerative neurological disease) Marfan syndrome (FBNI; connective tissue disorder, tissues of ligaments, blood vessel walls, cartilage, heart valves and other structures abnormally weak) Mucoplysaccharidosis (MPS; deficiency of enzymes needed to break down long chain sugars called glycosaminoglycans; corneal clouding, joint stiffness, heart disease, mental retardation) Myotonic dystrophy (MD; progressive muscle weakness, most common form of adult muscular dystrophy) Neurofibromatosis type 1(NF1; multiple benign nervous system tumors that can be disfiguring; cancers) Phenylketonuria (PKU; progressive mental retardation due to missing enzyme; correctable by diet) Polycystic kidney disease (PKD1, PKD2; cysts in the kidneys and other organs) Adult polycystic kidney disease (APKD; kidney failure and liver disease) Prader Willi/Angleman syndromes (PW/A; decreased motor skills, cognitive impairment early death) Sickle cell disease (SS; blood cell disorder; chronic pain and infections) Spinocerebellar ataxia, type 1(SCA1; involuntary muscle movements, reflex disorders, explosive speech) Spinal muscular atrophy (SMA; severe, usually lethal progressive musclewasting disorder in children) Tay-Sachs disease (TS; fatal neurological disease of early childhood, seizures, paralysis) Thalassemias (THAL; anemias-reduced red blood cell levels) Timothy syndrome (CACNA1C; characterized by sever cardiac arrhythmia, webbing of the fingers and toes called syndactyly, autism) SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 4 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: PROCEDURE: Prior to genetic testing being performed the Physician’s office must contact the scheduling department at 724-357-7075. The scheduling staff will require the office to obtain the proper authorization if needed prior to calling. The authorization and ordering script must be faxed at the time of scheduling. The ordering script and authorization form will be scanned into Meditech for other departments to prepare for the patient arrival by the scheduling staff. Appointments will have a two-day lead time and will only be scheduled Monday – Thursday 0630 to 1600 at the IRMC OP Lab at 835 Hospital Road location. Laboratory staff will have ample time to determine specimen requirements based on the test ordered and provide specimen integrity for shipping to the appropriate reference lab. Meditech Scheduling Software is programmed to flag the scheduling staff with the following message: THIS PROCEDURE WILL MORE THAN LIKELY REQUIRE A PRE-AUTHORIZATION. OFFICES MUST CALL INSURANCE TO VERIFY PATIENT PLAN REQUIREMENTS PER CPT. Physician’s office will be required to provide one of the following upon scheduling: Authorization number No authorization needed as per insurance o Name of the representative giving information from insurance provider o Info provided by representative o Who called (from Physician’s office) o Date and time called No authorization and meeting medical necessity as per policy/procedure The scheduler will place either the AUTHORIZATION # or NONE in the authorization field. SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 5 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Patient presents with authorization or verification: Testing can be ordered, collected and referred to the proper reference laboratory. Verify if multiple testing is ordered that all requiring authorizations are denoted on the authorization form. If not an additional authorization may need to be obtained. Patient presents without authorization: The genetic test listing below denotes requirements for pre-authorizations prior to collection. Contact the physician office and inform pre-authorization form must first be obtained prior to collection of specimen. The physician office can fax the form to the collection site Patient may need to return to have testing completed until authorization is received If patient is unwilling to return, they can complete an ABN form with the understanding they are responsible financially for any charges to IRMC The authorization or ABN must be scanned into the system along with the physician order SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 6 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Highmark Requirements Genetic testing performed on patients with no current evidence or manifestation of genetic disease (i.e., asymptomatic) is considered genetic screening and is noncovered except for those groups/programs that specifically identify coverage in benefits. This includes genetic testing performed to determine susceptibility or predisposition to diseases such as cancer and heart disease and genetic testing for carrier identification to determine if a person is a “carrier” of an abnormal gene. Highmark requires a pre-authorization form for the following tests: CYP2C19 (Drug Metabolism) CYP2D6 (Drug Metabolism) CYP2C9 (Drug Metabolism) CPT 81275 KRAS Gene Mutation CPT 81280 Long QT Syndrome Full Gene Sequence CPT 81281 Long QT Syndrome Known Familial Sequence Variant CPT 81282 Long QT Syndrome Deletion/Duplication Variants CPT 81401 TPMT Genotyping CPT 81403 Pancreatitis Mutation CPT (Dependent on Agent) Infectious Agent Genotype CPT 81479 Unlisted Pathology Test CPT 83520x5, 88347, 88347x2, 81401 Chrons Prognostic CPT 81257, 81401, 81403, 81404 Hgb Molecular Exam And Selection Of Retrieved Archival The following testing is covered for symptomatic patients. The testing is only covered for asymptomatic patients when the patient’s contract covers genetic testing. This is not an all-inclusive list. CPT: 81292, 81293, 81294, 81295, 81296, 81298, 81299, 81300, 81301, 81317, 81318, 81319) Inherited susceptibility to colon cancer CPT: 81220, 81221, 81222, 81223, 81224 Cystic Fibrosis Testing CPT: 81256 Hemochromatosis CPT: 81257 Alpha-Thalessemia CPT: 81255 Tay-Sachs Disease CPT: 81251 Gaucher Disease CPT: 81330 Niemann-Pic Disease CPT: 81241 Factor V Leiden Thrombophilia CPT: 81243, 81244 Fragile X Syndrome SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 7 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Genetic testing for prenatal and preconceptual carrier screening is considered medically necessary for individuals of Ashkenazi Jewish ancestry in accordance with the American College of Medical Genetics guidelines as follows: Bloom Syndrome Canavan Disease Cystic Fibrosis Dihydrolipoamide Dehydrogenase Deficiency (DLD) Familial Dysautonomia (FD) Familial Hyperinsulinism (FHI) Fanconi Anemia Type C Gaucher Disease Type 1 Glycogen Storage Disease type 1A Joubert Syndrome Maple Syrup Urine Disease Mucolipidosis IV Nemaline Myopathy (NM) Niemann-Pic Disease Type A Spinal Muscular Atrophy Usher Syndrome Type III and Type 1F Walker-Warburg Syndrome SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 8 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: UPMC Health Plan Requirements UPMC Health Plan requires prior authorization for the following genetic testing. Authorization should be approved based on the following indications. However, if testing is being performed based on the limitations medical necessity may not be proven. CPT Code: 81280 Long QT Syndrome Full Gene Sequence 81281 Long QT Syndrome Known Familial Sequence Variant 81282 Long QT Syndrome Deletion/Duplication Variants CPT Codes: Breast and Ovarian Cancer Testing 81211 BRCA1/BRCA2 Gene Analysis Common Variant 81212 BRCA1/BRCA2 185/5385/6174 Variants 81213 BRCA1/BRCA2 Uncommon Variant 81214 BRCA1 Gene Analysis Common Variants 81215 BRCA1 Known Familial Variant 81216 BRCA2 Gene Analysis Common Variants 81217 BRCA2 Known Familial Variant BRACAnalysis® Rearrangement Test (BART) (Myriad Genetic Laboratories, Inc., Salt Lake City, UT) Inherited Colorectal Cancers: (HPNCC, FAP and MAP testing) CPT Codes: Cystic Fibrosis Testing 81220 CFTR Gene Analysis Common Variants 81221 CFTR Known Familial Variants 81222 CFTR Dup/Del Variants 81223 CFTR Full Gene Sequence Genetic Testing for Long QT Syndrome: In order for medical necessity to be established, adequate information must be furnished by the treating physician. Necessary information includes, but is not limited to: Physician’s letter of medical necessity which includes supporting documentation such as patient symptoms, QT interval per EKG and family history with clinical documentation validating diagnosis. The Medical Management staff assigned to review obtains the clinical information according to determine if there is adequate clinical information. If the case does not meet established criteria, it is referred to a Medical Director. The Medical Director will SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 9 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: then determine if the request service is medically necessary and appropriate. The Medical Management staff completes the review process and communicates the review decision according to the Timeliness of UM Decisions policy for the member’s benefit plan. Indications: QTc interval >470 msec in males and >480 msec in females Documented history of Torsades de pointes Presence of T-wave alternans AND notched T Waves in 3 leads A first degree relative with a confirmed clinical diagnosis of LQTS Members with a QTc>440 msec AND an episode of aborted sudden death without another cause (such as cardiomyopathy or MI) Unexplained syncope and either A QTc >450 msec for males or >460 msec for females OR A known family member (1st or 2nd degree relative) with genetically identified LQTS Limitations: Members with a known cause of acquired LQTS such as drug induced, intracranial bleed or acute MI Genetic screening for LQTS in the general population Genetic screening to determine prognosis and/or direct therapy in patients with known LQTS Family testing of members with genetically-proven LQTS Molecular Susceptibility Testing for Breast Cancer and/or Ovarian (BRCA and BART Testing): In order to assess medical necessity for BRCA testing, adequate information must be furnished by the treating physician. Necessary information includes, but is not limited to: Physician’s letter of medical necessity to include o The physician’s evaluation of the member’s condition and o Detailed personal and family history of Breast/Ovarian and other pertinent cancers among first and second degree relatives (when applicable) o Additional information will be requested if necessary o BART test- BRCA test results in addition to the above information The Medical Management staff assigned to review obtains the clinical information according to determine if there is adequate clinical information. If the case does not meet established criteria, it is referred to a Medical Director. The Medical Director will SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 10 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: then determine if the request service is medically necessary and appropriate. The Medical Management staff completes the review process and communicates the review decision according to the Timeliness of UM Decisions policy for the member’s benefit plan. Indications for BRCA1/BRAC2 Test BRCA testing is indicated in any ONE (1) of the following situations (1-8) 1. Family history with known BRCA1/BRCA2 mutation (male or female) 2. Personal history of breast cancer (including invasive and ductal carcinoma insitu breast cancers) and at least ONE (1) of the following: Diagnosed age ≤ 45 years old Diagnosed age ≤ 50 years old AND o 1 close blood relative with breast cancer ≤ 50 years old OR o 1 close blood relative with epithelial ovarian cancer, fallopian cancer, or primary peritoneal cancer OR o Limited family history 2 breast primaries when first breast cancer diagnosis occurred prior to age 50(2 breast primaries include bilateral diseases or cases where there are 2 or more separate ipsilateral primary tumors) Diagnosed age < 60 yrs with triple negative breast cancer (ER neg, PR neg, HER neg) Diagnosed at any age AND o 2 close blood relatives with breast cancer or epithelial ovarian cancer, fallopian tube cancer, or primary peritoneal cancer at any age Close male blood relative with breast cancer Personal history of epithelial ovarian cancer, fallopian tube cancer, or primary peritoneal cancer Personal background of ethnicity that is associated with higher mutational frequency (e.g. founder populations of Ashkenazi Jewish, Swedish, Icelandic, Hungarian and Dutch) Note: Testing for founder mutation(s), if available, should be performed first. Full sequencing may be considered if other HBOC criteria are met. OR 3. Personal history of epithelial ovarian cancer, fallopian tube cancer, or primary peritoneal cancer OR 4. Personal history of male breast cancer SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 11 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: OR 5. Personal history of breast and/or ovarian cancer at any age AND 2 close blood relatives with pancreatic cancer at any age OR 6. Personal history of pancreatic adenocarcinoma at any age AND 2 close blood relatives with breast and/or ovarian and/or pancreatic cancer at any age OR 7. Family history only AND 1st or 2nd degree relative who meets any of the above criteria (1-6) OR 3rd degree blood relative with breast cancer and/or ovarian/fallopian tube/primary peritoneal cancer AND 2 close blood relatives with breast cancer (at least one with breast cancer ≤ 50yr and/or ovarian cancer (at least 1 with breast cancer 50 yr) OR 8. Limited family history, such as fewer than 2- 1st or 2nd degree female relatives or female relatives surviving beyond 45 year in either linage. Note: When investigating limited family history, the maternal and paternal sides should be considered separately. Testing Family Members Occasional, blood or tissue samples from other non-covered family members are required to provide the medical information necessary for the proper medical care of a member. Such molecular-based testing for BRCA and other specific heritable disorders in non-members will be reviewed for medical necessity when ALL of the flowing conditions are met: 1. The information is needed to adequately assess risk in the member AND 2. The information will be used in the immediate care plan of the member AND 3. The non-covered family member’s benefit plan (if any) will not cover the test and the denial is based on specific plan exclusion. SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 12 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Indications for BRACAnalysis® Rearrangement Test (BART): BART testing is indicated when the member is BRCA1/BRCA2 negative AND In any ONE (1) of the following situations (1-5) 1. Breast cancer before age 50 AND Family history of 2 or more close blood relatives with a diagnoses of breast cancer before age 50 and/or ovarian cancer at any age 2. Ovarian cancer at any age AND Family history of 2 or more close blood relatives with a diagnoses of breast cancer before age 50 and/or ovarian cancer at any age 3. Male breast cancer at an age AND Family history of 2 or more close blood relatives with a diagnoses of breast cancer before age 50 and/or ovarian cancer at any age 4. Breast cancer at or after age 50 and ovarian cancer at any age AND Family history of 1 or more close blood relatives with breast cancer before age 50 and/or ovarian cancer at any age 5. Breast cancer before age 50 and ovarian cancer at any age AND No additional relatives are required Limitations of BRCA1/BRCA2 and BART testing 1. Experimental and Investigational and therefore not covered: BRCA testing for assessment of risk of cancers other than breast or ovarian cancers 2. Not medically necessary and therefore not covered: Genetic testing in members less than 18 years old for BRCA1 and BRCA2 mutations When BRCA testing is performed primarily for medical management of other family members that are not covered by UPMC Insurance Services Division 3. Members post bone marrow transplant (allogenic or autologous) should not have testing via blood or buccal samples (due to contamination of donor DNA). In these cases, DNA should be extracted from a fibroblast culture. SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 13 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Genetic Testing for Inherited Colorectal Cancers: (HPNCC, FAP and MAP testing) HPNCC indications: UPMC Insurance utilizes modified Bethesda criteria to determine Medical necessity. Individuals must meet one of the following for medical necessity of HPNCC testing. Diagnosed with colorectal cancer before the age of 50 years Presence of synchronous or metachronous colorectal or other HNPCC related tumors regardless of age. Colorectal cancer with the MSI-H histology diagnosed in individual before the age of 60 years. Individuals with colorectal cancer with one or more first-degree relatives with an HNPCC related tumor, with one of the cancers diagnosed before age 50 years. Colorectal cancer diagnosed in two or more first or second degree relatives with an HNPCC related tumor, regardless of age. An alternative indication for who should have genetic testing is to perform the MSI-H testing on colon cancer tissue of patients meeting any of the Bethesda modified criteria. It the MSI-H is positive, the one could proceed with genetic testing for HNPCC. Note: Genetic testing to determine the carrier status of the HNPCC gene may be considered medically necessary in patients without a history of colorectal cancer but who have a first- or second-degree relative with a known HNPCC mutation. FAP indications: Members with greater than 100 colonic polyps identified by colonoscopy: OR History of FAP in first degree relatives Individuals with 10-100 adenomas may be considered for APC testing. MYH Associated Polyposis (MAP) indications: Individuals with personal history of adenomatous polyposis and a negative APC test and a negative family history for adenomatous polyposis. Individual with a personal history of AP and family history for recessive inheritance where only siblings are affected; OR Asymptomatic siblings of individuals with know MYH polyposis SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 14 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Cystic Fibrosis Genetic Testing: Indications: Diagnostic purpose o A clinical presentation of CF and a negative/equivocal sweat test o Infants with meconium ileus or other symptoms indicative of CF who are too young to produce adequate amounts of sweat for a sweat chloride test Carrier Screening for any of the following o Individuals with positive family history of CF o Adults with partners with known CF mutation or family history of and planning a pregnancy o Woman’s reproductive partner had CF or apparently isolated congenital bilateral absence of vas deferens Prenatal testing of fetus may be indicated for any of the following o Embryo at risk when either a parent has a diagnosis of CF, is a known carrier of a CFTR mutation of has a family history of CF o Fetus with fetal echogenic bowel per ultrasound during 2 nd trimester Limitations: Carrier screening in the general population If a patient has been previously testing, results should be documented and the test not repeated Complete gene sequencing (beyond the ACMG-23 standard mutation panel) is not appropriate for carrier screening because it may yield results that are difficult to interpret, hence it is not covered and requests for exceptions will be reviewed on a case by case basis. SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 15 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Cigna Requirements Genetic Disease Screening Panels: Cigna covers genetic testing for specific diseases and disorders as medically necessary when established criteria for that specific genetically transmitted disease are met. For specific criteria, please refer to the following related disease specific indications and limitations. CPT Code: Cystic Fibrosis Testing 81220 CFTR Gene Analysis Common 81221 CFTR Known Familial Variant 81223 CFTR Full Gene Sequence (NOT COVERED) CPT Code: Hemochromatosis 82156 Hemochromatosis HFE Gene Analysis CPT Code: Hereditary Hypercoagulability 81241 Factor V Leiden Variant 81240 Prothrombin G20210A Gene Analysis 81479 Unlisted Molecular Pathology Procedure (NOT COVERED) CPT Code: Hemoglobin Molecular consisting of: 81257 HBA1/HBA2 Gene Analysis Common Variant 81401 Molecular Procedure Level 2 81403 Molecular Procedure Level 4 81404 Molecular Procedure Level 5 CPT Code: Long QT Syndrome 81280 Long QT Syndrome Gene Analysis, full sequence 81281 Long QT Syndrome Gene Analysis, known familial sequence variant 81282 Long QT Syndrome Gene Analysis, duplication/deletion variants CPT Code: Breast Cancer and Ovarian Cancer Testing 81211 BRCA1/BRCA2 Gene Analysis Common Variant 81212 BRCA1/BRCA2 185/5385/6174 Variants 81213 BRCA1/BRCA2 Uncommon Variant 81214 BRCA1 Gene Analysis Common Variant 81215 BRCA1 Known Familial Variant 81216 BRCA2 Gene Analysis Common Variant 81217 BRCA2 Known Familial Variant BRACAnalysis® Rearrangement Test (BART)(Myriad Genetic Laboratories, Inc., Salt Lake City, UT) SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 16 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: CPT Code: TPMT Genotyping 81401 Molecular Procedure Level 2 Cystic Fibrosis: Cigna covers genetic testing for cystic fibrosis (CF) using the American College of Medical Genetics (ACMG) mutation core panel (ACMG-23) as medically necessary of any of the following: o Confirmatory testing Exhibition of symptoms of CF but has a negative sweat test Infant with other symptoms of CF but is too young to produce adequate volumes for sweat test. Infant with an elevated immunoreactive tyrpsinogen(IRT) with no suspicion of CF o Preconception or prenatal carrier testing of an individual who is pregnant or a prospective biologic parent o Prenatal testing of fetus (amniocentesis or chorionic villus sampling) Parent has a diagnosis of CF or a known carrier of mutation Fetal echogenic bowl has been identified on ultrasound ICD-9-CM Diagnosis Codes: 277.00 CF without mention of meconium ileus 277.01 CF with mention of meconium ileus 277.02 CF with pulmonary manifestations 277.03 CF with gastrointestinal manifestations 277.09 CF with other manifestations V82.71 Screening for genetic disease carrier status Cigna Does Not Cover for: o Carrier Screening in general population o Routine genetic mutation screening in newborns o Extended mutation panels o CPT: 81223 CFTR Full Gene Sequence SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 17 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Genetic Testing for Hereditary Hemochromatosis: Cigna covers genetic testing to confirm a diagnosis of HFE-HHC as medically necessary without a requirement for preand post-test genetic counseling when an individual has findings consistent with hemochromatosis and a serum transferrin iron saturation greater than or equal to 45%, but the diagnosis remains uncertain after completion of conventional testing. ICD-9-CM Diagnosis Code: 275.01 Hereditary hemochromatosis Genetic Testing for Hereditary Hypercoagulability Disorders: Cigna covers genetic testing with targeted mutation analysis for coagulation Factor V Leiden and coagulation factor II (20210G) as medically necessary for either of the following indications: o Confirmatory testing in ANY Of the following situations Age <50 with history of unexplained venous thrombosis Age <50 with unexplained arterial thrombosis in the absence of other risk factors for atherosclerotic vascular disease Venous thrombosis in an unusual site Recurrent venous thrombosis Venous thrombosis and a strong family history of thrombotic disease Venous thrombosis in a pregnant woman or a woman taking oral contraceptives MI in female smoker age <50 Predictive testing in a woman of childbearing age with intent/ability to conceive who has first-degree relative with history of high-risk thrombophilia ICD-9-CM Diagnosis Codes: 2869 Other and unspecified coagulation defects 28981 Primary hypercoagulable state 410.00-410.92 Acute Myocardial Infarction 444.0-444.9 Arterial embolism and thrombosis 452 Portal vein thrombosis 453.0-453.9 Other venous embolism and thrombosis 557.0 Acute vascular insufficiency of intestine 634.00-634.92 Spontaneous abortion 646.30 Habitual aborter, unspecified as to episode of care or not applicable 646.33 Habitual aborter, antepartum condition or complication 671.50-671.54 Other phlebitis and thrombosis in pregnancy and the puerperium V12.51 Personal history of venous thrombosis and embolism SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 18 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Cigna DOES NOT COVER for the following indications because they are not considered medically necessary: o General population screening o Routine screening during pregnancy or prior to the use of oral contraceptives, HRT or SERMs o Newborn or routine testing on asymptomatic child o Routine initial testing in an individual with arterial thrombosis o Adverse pregnancy outcomes such as recurrent pregnancy loss, preeclampsia, intrauterine growth restriction or placental abruption o Testing of an asymptomatic first-degree relative of an individual with proven symptomatic thromboembolism and a proven factor V Leiden of factor II mutations for the purpose of considering primary prophylactic anticoagulation o Prenatal testing of fetus Cigna DOES NOT COVER genetic testing for ANY of the following indications because it is considered experimental, investigational or unproven: o F2 (coagulation factor II) 1199G<A Variant o F5 (coagulation factor V) HR2 Variant o F7 (coagulation factor VII) R353Q Variant o F13B (factor XIII, B polypeptide), V34L variant ICD-9-CM Diagnosis Codes: Not covered V78.8 Special Screening for other disorders of blood and blood-forming organs V78.9 Special screening for unspecified disorder of blood and blood forming organs V82.71 Screening for genetic disease carrier status V82.79 Other genetic screening 2869 Other and unspecified coagulation defects 28981 Primary hypercoagulable state 410.00-410.92 Acute Myocardial Infarction 444.0-444.9 Arterial embolism and thrombosis SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 19 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Genetic Testing for Hemoglobinopathies: Cigna covers genetic testing for hemoglobinopathies (i.e. thalassmemias and sickle cell disease) as medically necessary for ANY of the following indications: o Confirmatory testing with targeted mutation analysis for common deletions or variants in gene HBB, HBA1 or HBA2 in the following situation Symptomatic individual with clinical features suggestive of a hemoglobinopathy, results by conventional studies yield equivocal results and a definitive diagnosis remains uncertain Infant with a newborn screening test positive for hemoglobinopathy o Confirmatory testing with sequence analysis when targeted mutation analysis is negative and the clinical suspicion of hemoglobinopathy remains high o Preconception or prenatal genetic testing to determine carrier status of a prospective biological parent with the capacity and desire to reproduce when ANY of the following applies An affected family member (first- or second-degree relative) who has thalassemia or sickle cell disease The individual is the reproductive partner of a known carrier The individual is of African, Asian, Mediterranean, Middle Easter or Caribbean descent and result of testing by conventional studies yield equivocal results and a definitive diagnosis remains uncertain o Prenatal testing of a fetus in either of the following situations: Testing targeted mutational analysis of the known mutation when both parents are known carriers for the disorder One parent is a known carrier and the mutation status of the other parent is not known and can’t be determined ICD-9-CM: 282.41-282.49 Thalassemias 282.5 Sickle Cell Trait 282.60-282.69 Sickle Cell Disease 282.7 Other hemoglobinopathies V18.9 Family history of genetic disease carrier V82.71 Screening for genetic disease carrier status SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 20 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Genetic Testing for Long QT Syndrome (LQTS): Cigna covers genetic testing for the long QT syndrome as medically necessary for ANY of the following indications: o Confirmatory testing with full sequent analysis when there is confirmed prolonged QT interval on electrocardiogram or Holter monitor and an acquired cause has been ruled out o Predictive testing with full sequence analysis when there is evidence in a first-degree relative of a history of prolonged QT interval on ECG or Holter monitor , sudden death or near sudden death and a genetic syndrome is suspected o Predictive testing for the known familial sequence variant when there is a positive genetic test for LQTS in a first-degree relative. o Prenatal testing of a fetus for known familial sequence variant when the disease-causing mutation has been identified in an affected biologic parent o Cigna covers genetic testing for LQTS with deletion and duplication analysis as medically necessary when sequence analysis is negative and the clinical suspicion of LQTS remains high. Cigna DOES NOT COVER genetic screening for LQTS if the general population, because such screening is considered not medically necessary or of unproven benefit. ICD-9-CM: 426.82 Long QT Syndrome 427.0-427.69 Cardiac Dysrhythmias 780.2 Syncope and collapse 780.4 Dizziness and giddiness V12.53 Personal history of sudden cardiac arrest V17.41 Family history of sudden cardiac death (SCD) V17.49 Family history of other cardiovascular diseases V18.9 Family history of genetic disease carrier Not covered: V82.79 Other genetic screening SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 21 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Genetic Testing for Susceptibility to Breast and Ovarian Cancer (BRCA1 and BRCA2): Cigna covers BRCA1 and BRCA2 genetic testing for susceptibility to breast or ovarian cancer in adults as medically necessary for ANY of the following indications: o Biologically-related individual from a family with a known BRCA1 or BRCA2 mutation o Personal history of breast cancer and ANY of the following: Diagnosed at age 45 or younger Diagnosed at age 50 or younger with EITHER of the following: At least one close blood relative with breast cancer at age 50 o o o o o or less At least one close blood relative with epithelial ovarian, fallopian tube or primary peritoneal cancer Diagnosed with two breast primaries (includes bilateral disease or cases where there are two or more clearly separate ipsilateral primary tumors) when the first breast cancer diagnosis occurred prior to age 50 Diagnoses at age 60 or younger with a triple negative breast cancer Diagnosed at age 50 or younger with a limited family history Diagnosed at any age and there are at least two close blood relatives with breast cancer or epithelial ovarian, fallopian tube or primary peritoneal cancer at any age Close male blood relative with breast cancer Personal history of epithelial ovarian, fallopian tube or primary peritoneal cancer Personal history of epithelial ovarian fallopian tube or primary peritoneal cancer Personal history of male breast cancer Personal history of breast, ovarian or pancreatic cancer at any age with two or more close blood relatives with breast, ovarian or pancreatic cancer at any age No personal history of breast or ovarian cancer and a family history of first- or second-degree blood relative meeting any of the above criteria No personal history of breast or ovarian cancer and a family history of a third-degree blood relative with breast and/or epithelial ovarian/fallopian tube/primary peritoneal cancer with two or more close blood relatives with breast and/or ovarian cancer SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 22 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Cigna covers BRACAnalysis® Rearrangement Test (BART)(Myriad Genetic Laboratories, Inc., Salt Lake City, UT) as medically necessary when conventional BRCA1/BRAC2 testing is negative and for ANY of the following indication: o Breast Cancer diagnosed before age 50 and a family history of EITHER of the following or o Ovarian Cancer diagnosed at an age and a family history of EITHER of the following or o Male breast cancer diagnosed at any age and a family history of EITHER of the following or o Breast cancer diagnosed at or after age 50 and ovarian cancer at an age and a family history of EITHER of the following Two or more diagnoses of breast cancer before age 50 (male breast at any age) Ovarian cancer at any age o Diagnosed with both breast cancer before age 50 and ovarian cancer at any age Cigna DOES NOT COVER BRCA1/BRCA2 genetic testing for susceptibility to breast cancer for the following because it is not considered medically necessary: o Genetic screening for general population o Testing of individuals with no personal history of breast or ovarian cancer except as noted above o Testing of individuals under 18 years of age Cigna DOES NOT COVER other genetic tests for susceptibility to breast and ovarian cancer because they are considered experimental, investigational or unproven. (e.g.Candidate breast cancer susceptibility genes and single nucleotide polymorphisms (SNPs) SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 23 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: ICD-9-CM Diagnosis Codes: 158.8 Malignant neoplasm of specified parts of peritoneum 158.9 Malignant neoplasm of peritoneum, unspecified 174.0-174.9 Malignant neoplasm of female breast 175.0-175.9 Malignant neoplasm of male breast 183.0 Malignant neoplasm of ovary 198.6 Secondary malignant neoplasm of ovary 198.81 Secondary malignant neoplasm of breast 233.0 Carcinoma in situ of breast 238.3 Neoplasm of uncertain behavior of breast V10.3 Personal history of malignant neoplasm of breast V10.41 Personal history of malignant neoplasm of cervix uteri V10.43 Personal history of malignant neoplasm of ovary V10.44 Personal history of malignant neoplasm of other female genital organs V10.88 Personal history of malignant neoplasm of other endocrine glands and related structures V16.0 Family history of malignant neoplasm of gastrointestinal tract V16.3 Family history of malignant neoplasm, breast V16.41 Family history of malignant neoplasm, ovary V84.01 Genetic susceptibility to malignant neoplasm of breast V84.02 Genetic susceptibility to malignant neoplasm of ovary Not medically covered: V82.79 Other genetic screening Genotyping for Thiopurine Methyltranferase (TPMT) Deficiency in Individuals with Inflammatory Bowel Disease (IBD): Cigna covers genotyping for thiopurine methyltransferase (TPMT) deficiency as medically necessary for the management of inflammatory bowel disease (IBD) for either of the following: o Prior to the initiation of azathioprine (AZA) or 6-mercaptopurine (6-MP) therapy o When standard dosing of AZA/6-MP fails to produce a therapeutic response ICD-9-CM Diagnosis Codes: 555.0-555.9 Regional enteritis, Crohn’s disease 556.0-556.9 Ulcerative colitis SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 24 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Gateway Health Plan Requirements Gateway has contracted with many participating hospitals and laboratory facilities for outpatient laboratory services. Gateway members are required to have all of their outpatient laboratory work completed through the appropriate contracted lab. Currently IRMC Lab is not a contracted laboratory with Gateway Medicaid or Medicare Assured. If IRMC is designated as a lab for any reason please contact Provider Services at 1800-685-5205 for further explanation of what services require an authorization. Authorizations are the responsibility of the ordering provider. STAT laboratory services must only be utilized in urgent cases. If a lab other than the member’s designated lab is to be used, a referral form is required. Every effort should be made to direct the member to his/her designated lab. Unusual circumstances arise where it is impossible to follow the laboratory procedures outlined above, please contact Gateway’s Utilization Management Dept at 1-800-3921146 for assistance. AETNA Requirements Aetna requires precertification for the following genetic testing: BRCA Genetic Testing: 1-877-794-8720 CPT Codes: 81211 BRCA1/BRCA2 Gene Analysis Common Variant 81212 BRCA1/BRCA2 185/5385/6174 Variants 81213 BRCA1/BRCA2 Uncommon Variant 81214 BRCA1 Gene Analysis Common Variants 81215 BRCA1 Known Familial Variant 81216 BRCA2 Gene Analysis Common Variants 81217 BRCA2 Known Familial Variant SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 25 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: Maternity genetic testing through the Beginning Right® Maternity Program: 1-800272-3531 CPT Code: Hemoglobin Molecular consisting of: 81257 HBA1/HBA2 Gene Analysis Common Variant 81401 Molecular Procedure Level 2 81403 Molecular Procedure Level 4 81404 Molecular Procedure Level 5 CPT Codes: 81280 Long QT Syndrome Gene Analysis, full sequence 81281 Long QT Syndrome Gene Analysis, known familial sequence variant 81282 Long QT Syndrome Gene Analysis, duplication/deletion variants CPT Codes: 81220 CFTR Gene Analysis Common Variants 81221 CFTR Known Familial Variant Pre-implantation genetic testing: 1-800-575-5999 Medicare Requirements Medicare states genetic testing will be covered if medical necessity is met. FirstCare PPO The services requiring preauthorization include, but are not limited to, those services listed below. This listing is subject to change. Please contact customer service 1-800240-3270 (Commercial) or 1-800-249-7366 (Self-funded) for information on the most up-to-date listing. Payments will be reduced for covered services if a pre-authorization form is not completed. Genetic Testing of any type- Excludes prenatal genetic testing HealthAmerica Coventry Genetic studies are listed as possibly needing prior authorization, but no specific testing is listed. For specific authorization information, use the Authorization Procedure Code Lookup at www.DirectProvider.com or contact Customer Service at 1-800-735-4404 (Western PA) or 1-800-290-0190 (Advantra). Coverage is subject to all plan provisions, limitations and eligibility. SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 26 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: CPT Information: DESCRIPTION BCR/ABL1 Major BREAK QUAL/QUANT BCR/ABL1 Min Break Qual/Quant BCR/ABL1 Other BREAK QUAL/QUANT BRAF Gene Analysis V600e Variant BRCA1/BRCA2 GENE Analysis Common VARIANT BRCA1/BRCA2 185/5385/6174 Variants BRCA1/BRCA2 Uncommon Variant BRCA1 Gene Analysis Common Variants BRCA1 Known Familial Variant BRCA2 Gene Analysis Common Variants BRCA2 Known Familial Variant CFTR Gene Analysis Common Variants CFTR Known Familial Variant CFTR Dup/Del Variants CFTR Full Gene Sequence CFTR Intron 8 Poly-T Analy EGFR Gene Analysis Common Variant PROTHROMBIN G20210A Gene Analysis FACTOR V LEIDEN Variant Gene Analysis HEMOCHROMATOSIS HFE Gene Analysis HBA1/HBA2 Gene Analysis Common Variant JAK2 Gene Analysis V617F Variant KRAS Gene Analysis Codon 12/13 Variant MTHFR Gene Analysis Common Variant SERPIN PEPTIDASE INHIB Gene Analysis HLA ONE LOCUS DQA1/DQB1 Molecular Procedure Level 2 Molecular Procedure Level 3 Molecular Procedure Level 4 Molecular Procedure Level 5 Unlisted Molecular Path Procedure CMV Gene Analysis By Nucleic Acid HBV Gene Analysis By Nucleic Acid MCR ALT CODE/CPT 81206 81207 81208 81210 81211 81212 81213 81214 81215 81216 81217 81220 81221 81222 81223 81224 81235 81240 81241 81256 81257 81270 81275 81291 81332 81376 81401 81402 81403 81404 81479 87910 87912 IRMC LIS code BCRABLFISH BRAF CYSFIB EGFR PTGENE F5MUT HEMOCHROMA JAK2 KRAS MTHFR in A1APHENO SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 27 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: DESCRIPTION Pancreatitis Mutation Molecular Procedure Level 4 HGB Molecular HBA1/HBA2 Gene Analysis Common Variant Molecular Procedure Level 2 Molecular Procedure Level 4 Molecular Procedure Level 5 Chrons Prognostic Immunoassay Quant #1 Immunoassay Quant #2 Transglutaminase Antibody ASIALOGM1 IGG ASIALOGM1 IGM GD1A IGG Immunofluorescent Indirect Molecular Procedure Level 2 TPMT Genotyping Molecular Procedure Level 2 REVISED: MCR ALT CODE/CPT IRMC LIS code HERPANMUT 81403 81257 81401 81403 81404 CROHNPROG 83520 83520 88347 83520 83520 91 83520 91 88347 81401 TPMTGENO 81401 SUBJECT: GENETIC TESTING REQUIREMENTS REFERENCE # GL100-1 PAGE: Page 28 of 28 DEPARTMENT: DEPARTMENT OF LABORATORY MEDICINE EFFECTIVE: 4/1/2013 APPROVED BY: REVISED: REFERENCES: Aetna Participating Provider Precertification List; 23.03.858.1P,Effective 1/1/13 Aetna Medical Precertification List, www.aetna.com/healthcare-professionals/policiesguidelines/precertification _policy, Obtained 2/4/13 Cigna Medical Coverage Policy Number 0280: Genetic Disease Screening Panels Effective Date 2/15/12 Cigna Medical Coverage Policy Number 0022: Genetic Testing for Cystic Fibrosis, Effective Date 1/15/13 Cigna Medical Coverage Policy Number 0255: Genetic Testing for Hereditary Hypercoagulability Disorders, Effective Date 12/15/12 Cigna Medical Coverage Policy Number 0192: Genetic Testing for Hemoglobinopathies,Effective Date 9/15/12 Cigna Medical Coverage Policy Number 0193: Genetic Testing for Long QT Syndrome (LQTS), Effective Date 10/15/12 Cigna Medical Coverage Policy Number 0001: Genetic Testing for Susceptibility to Breast and Ovarian Cancer (e.g.BRCA1 & BRAC2), Effective Date 3/15/12 Cigna Medical Coverage Policy Number 0003: Genotyping for Thiopurine Methyltransferase (TPMT) Deficiency in Individuals with Inflammatory Bowel Disease (IBD), Effective Date 1/15/13 FirstCare PPO Services Requiring Pre-Authorization Gateway Health Plan®, Laboratory Services, 2012 Medicaid Provider Office Policy and Procedure Manual pp 51-52. Coventry HealthAmerica/Advantra; Prior Authorization List Highmark Medical Policy Bulleting, Section Laboratory, Number L-34, Genetic Testing, Effective date 1/1/2013 Highmark Special Bulletin for Network Providers,”Highmark to Update Its List of Outpatient Procedures/Services Requiring Authorization” Rev 10/12. Highmark’s List of Procedures/DME Requiring Authorization Rev. 10/12 Medicare National Coverage Determinations Manual, Chapter 1, Part 3 (Sections 170190.34) Coverage Determinations Rev. 131, 2-23-11 UPMC Healthplan Physician Partner Update Technology Assessment Committee 4/2012 UPMC Healthplan Quick Reference Guide Effective 2/1/2013 UPMC Healthplan Policy:PAY.080, 3/2012 Genetic Testing UPMC Healthplan Policy:PAY.116, 6/2012 Genetic Testing for Cystic Fibrosis UPMC Healthplan Policy:PAY.042, Rev 8/12 Genetic Testing for Inherited Colorectal Cancers UPMC Healthplan Policy:MP.055, Rev 7/2012 Molecular Susceptibility Testing for Breast Cancer and/or Ovarian Cancer (BRCA and BART Testing) UPMC Healthplan Policy: MP.027, Rev 5/2012 Genetic Testing for Long QT Syndrome