9. KCHFT CUP Pathway FINAL 2015
advertisement
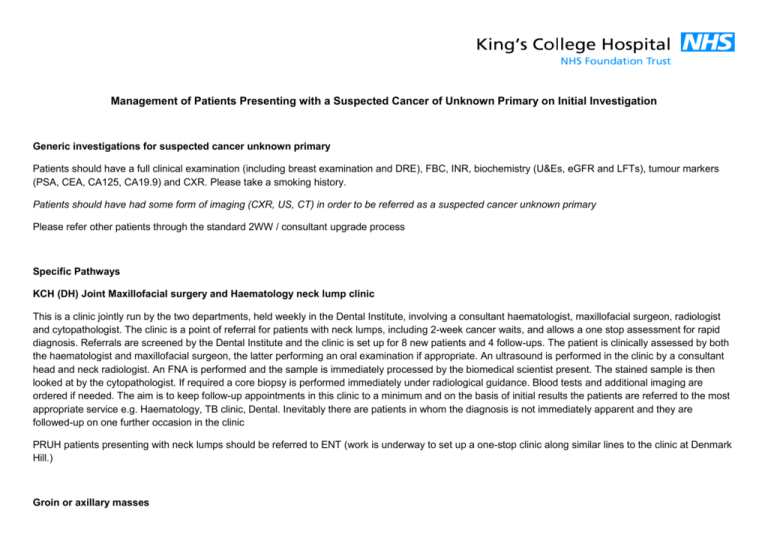
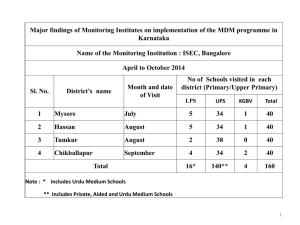
Management of Patients Presenting with a Suspected Cancer of Unknown Primary on Initial Investigation Generic investigations for suspected cancer unknown primary Patients should have a full clinical examination (including breast examination and DRE), FBC, INR, biochemistry (U&Es, eGFR and LFTs), tumour markers (PSA, CEA, CA125, CA19.9) and CXR. Please take a smoking history. Patients should have had some form of imaging (CXR, US, CT) in order to be referred as a suspected cancer unknown primary Please refer other patients through the standard 2WW / consultant upgrade process Specific Pathways KCH (DH) Joint Maxillofacial surgery and Haematology neck lump clinic This is a clinic jointly run by the two departments, held weekly in the Dental Institute, involving a consultant haematologist, maxillofacial surgeon, radiologist and cytopathologist. The clinic is a point of referral for patients with neck lumps, including 2-week cancer waits, and allows a one stop assessment for rapid diagnosis. Referrals are screened by the Dental Institute and the clinic is set up for 8 new patients and 4 follow-ups. The patient is clinically assessed by both the haematologist and maxillofacial surgeon, the latter performing an oral examination if appropriate. An ultrasound is performed in the clinic by a consultant head and neck radiologist. An FNA is performed and the sample is immediately processed by the biomedical scientist present. The stained sample is then looked at by the cytopathologist. If required a core biopsy is performed immediately under radiological guidance. Blood tests and additional imaging are ordered if needed. The aim is to keep follow-up appointments in this clinic to a minimum and on the basis of initial results the patients are referred to the most appropriate service e.g. Haematology, TB clinic, Dental. Inevitably there are patients in whom the diagnosis is not immediately apparent and they are followed-up on one further occasion in the clinic PRUH patients presenting with neck lumps should be referred to ENT (work is underway to set up a one-stop clinic along similar lines to the clinic at Denmark Hill.) Groin or axillary masses Patients presenting with masses in the axilla or groin should be referred to the DH or PRUH breast units for assessment and FNA / biopsy Intra-abdominal masses Patients presenting with an intra-abdominal mass are usually referred to GI services. Patients with an abdominal mass will be discussed at the weekly colorectal cancer MDM (attended by GI surgeons, gastroenterology and radiology). The aim of the discussion will be to agree the optimal way of obtaining a tissue diagnosis. Patients will be managed by the referring clinical team whilst on this patient pathway. GPs that identify a patient with an unexplained intraabdominal mass should refer the patient to the GI surgeons using the existing referral pathways to facilitate timely diagnosis Adrenal/ Paracaval / retroperitoneal masses Patients presenting with adrenal or paracaval / retroperitoneal masses which do not appear to be pancreatic or renal in origin should be referred to the adrenal / Endocrine MDM, based at DH. The endocrine team will work-up undifferentiated retroperitoneal masses and, following confirmation of the diagnosis, refer on as appropriate. Direct referral to this MDT is most appropriate because: 1. Biopsy for tissue diagnosis is contraindicated in any adrenal mass or possible paraganglioma without initial work up 2. Diagnosis is almost always achieved based on biochemistry, subspecialty radiology and nuclear medicine all of which are available. 3. In the unusual instance where histological diagnosis is needed before resection this can would be organised by the MDT Brain metastases KCH is the regional centre for neuro-oncology and patients with a new space occupying lesion in the brain will be referred to the MDT for a specialist opinion. On imaging it can be difficult to differentiate a primary brain tumour from metastatic disease: any space occupying lesion in the brain may look like a metastasis on imaging and multiple lesions could be multi-focal glioma. Following review at the neuro-oncology MDT and where clinically appropriate, most patients with brain-only metastatic disease will require a brain biopsy to obtain a tissue diagnosis. Where the decision is taken that a brain biopsy is either not technically feasible or that the patient is too unwell to undergo the procedure, referral to the local AOS / CUP team should be included in the neuro-oncology MDT recommendations. Suspected Cancer Unknown Primary Referral Pathway for GP / Internal Clinical Teams Head and Neck Lumps Axilla / Inguinal / Femoral Lumps Detected mass on Chest X-ray/chest CT Abdominal mass identified clinically and confirmed on US / CT Retroperitoneal mass Ascites (nonmalignant cause excluded) Liver metastase s Bone metastases (e.g. bone scan, CT or MRI) M Joint clinic Max Fax & Haematology (DH) ENT referral (PRUH) Breast clinic referral for assessment Lung cancer referral MDM for discussion & agreement of further investigations FNA Diagnostic FNA Non diagnostic FNA Lower GI cancer referral MDM for discussion re method of obtaining tissue: CT/LAP/Open biopsy Adrenal MDM & work up HPB MDM F Female: refer to gynae rapid access clinic Refer to lung cancer team Diagnostic biopsy where indicated – ordered by investigating MDM Results review at relevant MDM Any further investigations ordered by MDM Lymphoma confirmed Haematology MDM referral Not cancer Solid tumour malignancy confirmed OPA follow up if significant other pathology identified OR Discharge to GP Screening tests unhelpful Appropriate cancer MDM (including CUP MDM at GSTT for true unknown primary) Screening suggests specific pathway, e.g. abnormal CXR, raised PSA abnormal breast examination