Neuroinflammation in Alzheimer`s disease
advertisement

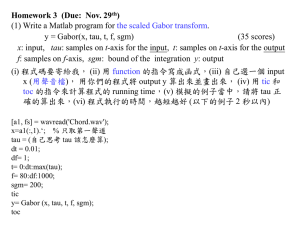
Astrocytes and neuroinflammation in Alzheimer’s disease Emma C Phillips1, Cara Croft1, Ksenia Kurbatskaya1, Michael J O’Neill2, Michael L Hutton2, Diane P Hanger1, Claire J Garwood3*, Wendy Noble1*a King’s College London, Institute of Psychiatry, Department of Neuroscience, De Crespigny Park, London, UK. 1 2 Eli Lilly and Company, Erl Wood Manor, Windlesham, Surrey, UK. Department of Neuroscience, Sheffield Institute for Translational Neuroscience, University of Sheffield, Sheffield, UK. 3 *These authors contributed equally to this work. a Corresponding author: Dr Wendy Noble, Department of Neuroscience, King’s College London, Institute of Psychiatry, De Crespigny Park, London, UK. Tel: 020 7848 0578. Email: wendy.noble@kcl.ac.uk. Keywords: Alzheimer’s disease, tauopathy, astrocyte, glia, inflammation Abstract Increased production of β-amyloid (Aβ) and altered processing of tau in Alzheimer’s disease are associated with synaptic dysfunction, neuronal death, cognitive and behavioural deficits. Neuroinflammation is also a prominent feature of Alzheimer brain and considerable evidence indicates that inflammatory events play a significant role in modulating the progression of AD. The role of microglia in AD inflammation has long been acknowledged. Substantial evidence now demonstrates that astrocyte-mediated inflammatory responses also influence pathology development, synapse health and neurodegeneration in AD. Several antiinflammatory therapies targeting astrocytes show significant benefit in models of disease, particularly with respect to tau-associated neurodegeneration. However, the effectiveness of these approaches is complex since modulating inflammatory pathways often has opposing effects on the development of tau and amyloid pathology, and is dependent on the precise phenotype and activities of astrocytes in different cellular environments. Increased understanding of interactions between astrocytes and neurons under different conditions is required for the development of safe and effective astrocyte-based therapies for AD and related neurodegenerative diseases. Introduction Alzheimer’s disease (AD) is a progressive neurodegenerative disease and the most common form of dementia. Clinical symptoms of AD include memory loss, confusion and behavioural changes. AD is characterised neuropathologically by the development of ß-amyloid (Aß) containing extracellular plaques, intracellular neurofibrillary tangles, comprised mainly of abnormally phosphorylated and aggregated tau protein, and widespread synaptic degeneration and neuronal loss [1]. It seems likely that several interconnected events lead to synaptic dysfunction and neuronal death in AD. A complex relationship between Aβ and tau is believed to play a key role in these processes [1], with tau deficiency protecting from Aβ-induced neurodegeneration and cognitive decline [2]. Neuroinflammation is another prominent feature of AD brain that plays a significant role in modulating disease progression [3]. Neuroinflammation in Alzheimer’s disease Rather than being simply a “bystander” pathology, experimental evidence demonstrates that neuroinflammation plays an active role in the development and progression of AD [3, 4]. In support of this view, recent genome-wide association studies have shown that variants of several immune genes, including complement receptor 1 (CR1) and triggering receptor expressed on myeloid cells 2 (TREM2), increase the risk of developing AD [5]. Aß-containing plaques in AD brain are surrounded by a halo of activated glial cells [6], and Aß is known to lead to the activation of astrocytes and microglia, along with induction of inflammatory signalling cascades [7, 8]. Both microglia and astrocytes release a myriad of pro- and anti- inflammatory cytokines under different conditions. Changes in the cellular environment elicit a range of responses that are not well defined or predictable, and that likely account for reports of both protective and neurotoxic effects of glial stimulation in models of disease [8-10]. Cytokines can be classified into several sub-families, including the interferons (IFNs), interleukins (IL)-1, -2, -10, and -17, tumour necrosis factors (TNFs), and chemokines, including monocyte chemoattractant proteins (MCPs) and macrophage inflammatory proteins (MIPs). There is usually some redundancy in these secreted factors, with several different cytokines having similar actions. Cytokines signal via a number of pathways that have been implicated in AD. For example, binding of MCP-1, IL-1, IL-6, TNFα and interferons to their neuronal receptors leads to activation of protein kinase C, caspase-1 and caspase-3, p38 and JNK mitogen-activated protein kinases (MAPKs), and phosphoinositide 3-kinase pathways [11]. In affected regions of AD brain, increased amounts of several classes of cytokines, including IL-1β, IL-6, IL-8, IL-18, MIP-1β, S100β, MCP-1, TNF-α and transforming growth factor beta (TGFβ), have been detected in association with plaques and tangles [12-15]. In accordance with this, the amounts of several pro-inflammatory mediators in peripheral fluids have been suggested as sensitive and specific biomarkers of AD [16]. The majority of transgenic rodent models of AD also exhibit prominent neuroinflammatory responses, with the severity of inflammatory cell infiltration correlating strongly with pathology development [17-18], cognitive decline [19], synaptic degeneration and neuronal death [17,20]. In addition, lipopolysaccharide-induced glial activation results in inflammatory responses that accelerate disease progression in transgenic models of AD [21]. These results suggest that, rather than simply occurring as a response to neurotoxic stimuli, inflammation directly affects pathways that lead to neurodegeneration. Much research has focussed on elucidating the role of microglia in the development of AD. There appears to be a spectrum of microglial changes that can have either a protective influence or be detrimental to neuron health [9]. For example, phagocytosis of Aβ by microglia is believed to be a protective mechanism [22], at least in younger animals [23]. However, increased pro-inflammatory cytokine production by microglia also results in neuronal loss in models of AD [23]. There is also evidence that microglial responses can have opposing influences on the development of amyloid and tau pathology. The NOD-like receptor family, pyrin domain containing 3 (NLRP3) inflammasome plays an important role in microglial inflammatory reactions. When NLRP3-deficient mice are crossed with a mouse model of AD that over-expresses mutant human amyloid precursor protein together with mutant presenilin (APP/PS1), the offspring show rescue of spatial memory, reduced caspase-1 activation and increased Aß clearance [24], suggesting that microglial activation exacerbates AD-like pathology. Conversely, fractalkine receptor (CX3CR1) is microglial specific, and its chemokine ligand (CX3CL1) is highly expressed in neurons. Crossing fractalkine receptor-deficient mice with mice that overexpress the entire wild-type human tau gene in the absence of mouse tau (htau mice), results in offspring with enhanced microglial activation and increased tau phosphorylation and aggregation [25]. Thus, microglial fractalkine may play a neuroprotective and anti-inflammatory role in animals that model tauassociated neurodegeneration. Astrocytes in healthy and Alzheimer’s disease brain It is estimated that astrocytes represent between 30%-50% of human neural cells [26], and they have long been acknowledged to provide crucial trophic and metabolic support for neurons. They have multiple roles, including secretion of important neurotrophic factors, such as TGFβ, brain-derived neurotrophic factor (BDNF) and nerve growth factor, they transport the vast majority of extracellular glutamate, and they convert glucose to lactic acid, which is taken up by neurons and converted to pyruvate for energy metabolism [27]. Astrocytes are also essential components of tripartite synapses [28], which are responsible for bidirectional communication between pre- and post-synaptic neurons and integrated glial cells. As such, astrocytes are critical for basal synaptic transmission, long-term potentiation (LTP), and cortical circuit function [29]. In AD brain, there are alterations in astrocyte morphology, gene expression, protein composition and activity, that are linked to changes in astrocyte function [30]. Altered astrocyte morphology in aging and diseased brain is complex and region-specific [31], however, the accumulation of activated astrocytes, often in clusters around amyloid plaques [6], correlates strongly with Braak staging in AD [32]. Importantly, astrocyte activation, together with the presence of phosphorylated tau in synapses, is one of the best biological correlates of cognitive decline in AD [33]. Accumulations of activated astrocytes in affected brain regions are also observed in many transgenic mouse models of AD, often prior to the appearance of plaque and/or tangle pathology [34], suggesting that astrocyte activation is involved in disease pathogenesis. Astrogliosis is associated with a series of cellular events including the release of nitric oxide (NO), reactive oxygen species, pro-inflammatory cytokines (such as TNFα, IL-1β and IL-6), and prostaglandin, all of which can have deleterious effects on neuronal function and health. In addition, many activated astrocytes in AD brain and in transgenic models of AD, express high levels of calcineurin, a protein phosphatase that mediates inflammatory responses. Recent studies have shown that astrocytes are activated by A, resulting in the release of inflammatory factors that reduce synaptic and neuronal health in cell models of AD [7, 8, 35]. Importantly, astrocytes are required to mediate the effects of Aβ on tau phosphorylation and cleavage, and this is linked with increased release of inflammatory mediators including IL-1, TNF and IL-6 [8]. Astrocyte activation and increased amounts of these inflammatory factors are also associated with the development of tauopathy in htau mice [18]. Taken together, this suggests that astrocytes play a part in disease progression in AD, likely due to their activation resulting in increased secretion of inflammatory mediators. The therapeutic potential of targeting astrocytes and disrupting astrocytic inflammatory signalling In many AD patients there is a relatively late onset of symptomatic impairment which creates an opportunity for effective therapeutic intervention. However, currently prescribed drugs only reduce the symptoms of disease, and have little or no effect on disease progression. A variety of therapies, primarily designed to prevent excess Aβ production, tangle formation, and/or the spread of disease pathologies, are currently under investigation. Another active area of interest is reduction of inflammatory signalling, since this may result in reduced neuronal vulnerability to degenerative mechanisms. Some of the best evidence that targeting inflammatory responses in astrocytes could be an effective therapeutic strategy in AD was provided by Furman et al. [35]. In response to Aβ and inflammatory mediators, astrocytic calcineurin is activated, leading to dephosphorylation of nuclear factor of activated T-cells (NFAT) transcription factors, and induction of astrocyte activation and inflammatory cytokine production. Furman et al. [35] showed that modulating astrocytic inflammatory signalling in APP/PS1 mice by targeted expression of VIVIT, a peptide that interferes with calcineurin/NFAT signalling, prevents astrocyte activation, lowers Aβ levels and improves synaptic function and measures of learning and memory. Pharmacological approaches also demonstrate the benefits of reducing astrocyte activation in transgenic mouse models of AD. Treatment of htau transgenic mice with minocycline, a tetracycline antibiotic derivative with potent anti-inflammatory effects, significantly reduced numbers of activated astrocytes and inflammatory mediators [18], and decreased pathological phosphorylated, cleaved and aggregated tau species [36]. Follow up studies in primary neural cell cultures demonstrated that minocycline diminishes the release of inflammatory factors from astrocytes, thereby preventing Aß-induced increases in tau phosphorylation, tau cleavage, and neurotoxicity. Comparison of the effects of minocycline in pure neuronal cultures with mixed neuronal and astrocytic cultures, showed that the protective effects of minocycline were mediated by astrocytes, and that neurons were relatively resistant to Aß in the absence of astrocytes [8]. Neutral sphingomyelinase (N-SMase) inhibitors have also shown benefit in models of AD by reducing astrocytic inflammatory pathways. N-SMase degrades sphingomyelin to produce ceramide, a lipid second messenger molecule that can trigger cell death in neurons and astrocytes [37]. Aß and IL-1 activate N-SMase and induce production of ceramide in human primary neurons [7]. Inhibiting N-SMase, either by knock down or by pharmacological inhibition, reduces astrocyte activation and amounts of pro-inflammatory cytokines, thereby protecting neurons from Aß-induced cell death [7]. Taken together, this evidence suggests that targeting astrocytic inflammatory pathways may be a means to slow the development of tau and amyloid pathologies, synaptic dysfunction and neuron death in AD. There is also evidence that astrocytes may be protective in animal models of AD. For example, genetic ablation of glial fibrillary acidic protein and vimentin in APP/PS1 mice, prevents astrocyte activation and results in accelerated plaque deposition and increased dystrophic neurites [38]. The apparent discrepancies in the influence of astrocytes in these disease models may reflect differences in the mechanisms by which astrocytes are associated with tau- and Aβ- mediated degeneration, as discussed above for microglia. However, protective effects of astrocytes in tau models of dementia have also been reported. Transgenic mice over-expressing mutant (P301S) tau display age-dependent development of tau pathology, neuroinflammation, cognitive decline and loss of specific cortical neurons [39]. Hampton et al. [10] set out to determine if transplantation of neural precursor cells was able to prevent the disease phenotype in these animals. Unexpectedly, they found that the transplanted neural stem cells differentiated into astrocytes and that this conferred neuroprotection. A similar approach was taken in 3xTg-AD mice, which express mutant forms of human tau (P301L), APP (K670N-M671L), and PS1 (M146V). When neural stem cells were transplanted into the brains of these mice, the majority of the cells differentiated into astrocytes, and recovery of hippocampal synaptic degeneration, spatial learning and memory deficits were observed [40]. The beneficial effects observed in this mouse model were ascribed to production of BDNF from the transplanted cells [40]. These studies further indicate that the phenotype of astrocytes under different conditions can have widely divergent effects, depending on their environment. In the studies described here, these differences likely reflect the protective/neurotrophic influence of naïve new-born astrocytes, and the toxic influence of astrocytes that have changed their phenotype as a result of aging and/or their sustained presence in a diseased (and possibly pro-inflammatory) environment. Targetting specific inflammatory signalling pathways Targeting specific pro-inflammatory cytokines could represent an alternative approach for treating AD. IL-1ß is a pro-inflammatory cytokine synthesised and released by both activated microglia and astrocytes. Single nucleotide polymorphisms in IL-1ß increase the risk of developing AD, and IL-1ß expression is elevated in AD relative to age-matched control brain [41]. In primary mixed neuronal and glial cultures, IL-1ß elevates tau phosphorylation via p38 MAPK and decreases the amount of the pre-synaptic marker, synaptophysin [42], changes that are blocked by IL-1 receptor antagonists. Similarly, increased levels of phosphorylated tau closely correlate with IL-1β amounts in the cortex of htau mice, and treatment of these mice with minocycline reduces both IL-1β and phosphorylated tau [18]. Finally, transgenic over-expression of IL-1ß in 3xTg-AD mice causes substantial increases in tau phosphorylation that is associated with activation of p38 MAPK and GSK-3 [43]. However, marked reductions in the burden of Aβ in the brains of these animals were also observed, again highlighting a possible dissociation between the effects of inflammatory mediators on tau and Aβ pathologies. IL-18 is another pro-inflammatory cytokine released by activated astrocytes. IL-18 can regulate N-methyl-D-aspartate (NMDA) receptor function, and may impair LTP [44]. NMDA receptor activity can influence tau structure and function in multiple ways. For example, NMDA receptor-mediated signalling influences the cleavage of tau by calpains and also tau phosphorylation by kinases such as extracellular signal-related kinase [45]. Furthermore, stimulating NMDA receptor activity elevates neuronal tau release in vivo [46]. The transsynaptic spread of tau pathology in AD is thought to underlie the progression of disease through anatomically connected brain regions [47], and thus it is possible that inflammatory mediators such as IL-18 may influence tau transmission via an effect on NMDA receptor function. Conclusions Neuroinflammation is a prominent feature of AD brain that has a significant influence on disease progression [3]. Microglia, the primary immune cells in the brain, play a major role in mediating inflammatory responses in AD brain, however, recent evidence has suggested that astrocytes also play a key role in disease pathogenesis. Activation of astrocytes leads to increased release of inflammatory mediators, including IL-1ß and IL-18. These proinflammatory cytokines can signal to neurons and initiate signalling pathways that affect Aβ production, tau processing and function. Genetic and pharmacological modulation of astrocytic inflammatory signalling results can be beneficial in cell and animal models of AD, particularly with respect to tau-associated degeneration. Astrocytes are critical for many fundamental CNS functions that are known to be dysregulated in AD, including regulation of cellular calcium, basal synaptic transmission, LTP, cortical circuit maintenance, and synaptic pruning [29, 48]. Many of these processes are known to be influenced by inflammatory mediators, particularly IL-1 [49-50], and thus modulating the astrocytic inflammatory signalling could have substantial benefit in AD. However, the effectiveness of astrocytetargetted anti-inflammatory treatments is significantly confounded by the complex interplay between tau and amyloid pathologies, and the phenotype and function of activated astrocytes in different cellular environments. A greater understanding of these events is required for the development of safe and effective astrocyte-based therapies for AD. Acknowledgements Work in the authors’ laboratories is supported by the Biotechnology and Biological Sciences Research Council, National Council for the Replacement, Refinement and Reduction of Animals in Research, Alzheimer’s Research UK, and Eli Lilly and Co. Ltd. List of abbreviations Aß: ß-amyloid AD: Alzheimer’s disease APP: amyloid precursor protein GSK-3: Glycogen synthase kinase 3 IFN: interferon IL: Interleukin LTP : long-term potentiation MAPK : mitogen activated protein kinase MIP : macrophage inflammatory protein MCP : monocyte chemoattractant protein NFAT: nuclear factor of activated T-cells NMDA: N-methyl-ᴅ-aspartate N-SMase: Neutral sphingomyelinase PS: presenilin TNF: Tumour necrosis factor References [1] Crimins, J.L., Pooler, A., Polydoro, M., Luebke, J.I., Spires-Jones, T.L. (2013). The intersection of amyloid β and tau in glutamatergic synaptic dysfunction and collapse in Alzheimer's disease. Ageing Res Rev. 12(3), 757-63. [2] Ittner, L.M., Götz, J. (2011). Amyloid-β and tau--a toxic pas de deux in Alzheimer's disease. Nat Rev Neurosci. 12(2), 65-72. [3] McGeer, E.G., McGeer, P.L. (2010). Neuroinflammation in Alzheimer's disease and mild cognitive impairment: a field in its infancy. J Alzheimers Dis. 19(1), 355-61. [4] Zhang, B., Gaiteri, C., Bodea, L.G., Wang, Z., McElwee, J., Podtelezhnikov, A.A., Zhang, C., Xie, T., Tran, L., Dobrin, R., Fluder, E., Clurman, B., Melquist, S., Narayanan, M., Suver, C., Shah, H., Mahajan, M., Gillis, T., Mysore, J., MacDonald, M.E., Lamb, J.R., Bennett, D.A., Molony, C., Stone, D.J., Gudnason, V., Myers, A.J., Schadt, E.E., Neumann, H., Zhu, J., Emilsson, V. (2013). Integrated systems approach identifies genetic nodes and networks in late-onset Alzheimer's disease. Cell. 153(3), 707-20. [5] Morgan, K. (2011). The three new pathways leading to Alzheimer's disease. Neuropathol Appl Neurobiol. 37(4), 353-7. [6] Walsh, D.M., Selkoe, D.J. (2004). Deciphering the molecular basis of memory failure in Alzheimer's disease. Neuron. 44(1), 181-93. [7] Jana, A., Pahan, K. (2010) Fibrillar amyloid-beta-activated human astroglia kill primary human neurons via neutral sphingomyelinase: implications for Alzheimer's disease. J Neurosci. 30:12676-12689. [8] Garwood, C.J., Pooler, A.M., Atherton, J., Hanger, D.P., Noble, W. (2011). Astrocytes play a key role in Aβ-induced tau phosphorylation and neurotoxicity in primary culture. Cell Death Dis. 2:e167. [9] Perry, V.H. (2010). Contribution of systemic inflammation to chronic neurodegeneration. Acta Neuropathol. 120(3), 277-86. [10] Hampton, D.W., Webber, D.J., Bilican, B., Goedert, M., Spillantini, M.G., Chandran, S. (2010). Cell-mediated neuroprotection in a mouse model of human tauopathy. J Neurosci. 30(30):9973-83. [11] Anisman, H. (2009) Cascading effects of stressors and inflammatory immune system activation: implications for major depressive disorder. J Psychiatry Neurosci 34:4-20. [12] Fillit, H., Ding, W.H., Buee, L., Kalman, J., Altstiel, L., Lawlor, B., Wolf-Klein, G. (1991) Elevated circulating tumor necrosis factor levels in Alzheimer's disease. Neurosci Lett. 129(2), 318-20. [13] Dickson, D.W., Lee, S.C., Mattiace, L.A., Yen, S.H., Brosnan, C. (1993). Microglia and cytokines in neurological disease, with special reference to AIDS and Alzheimer's disease. Glia. 7(1), 75-83. [14] Huell, M., Strauss, S., Volk, B., Berger, M., Bauer, J. (1995). Interleukin-6 is present in early stages of plaque formation and is restricted to the brains of Alzheimer's disease patients. Acta Neuropathol. 89(6), 544-51. [15] Ojala, J., Alafuzoff, I., Herukka, S.K., van Groen, T., Tanila, H., Pirttilä, T. (2009). Expression of interleukin-18 is increased in the brains of Alzheimer's disease patients. Neurobiol Aging. 30(2), 198-209. [16] Lee, K.S., Chung, J.H., Choi, T.K., Suh, S.Y., Oh, B.H., Hong, C.H. (2009). Peripheral cytokines and chemokines in Alzheimer's disease. Dement Geriatr Cogn Disord. 28(4), 2817. [17] Janelsins, M.C., Mastrangelo, M.A., Park, K.M., Sudol, K.L., Narrow, W.C., Oddo, S., LaFerla, F.M., Callahan, L.M., Federoff, H.J., Bowers, W.J. (2008) Chronic neuron-specific tumor necrosis factor-alpha expression enhances the local inflammatory environment ultimately leading to neuronal death in 3xTg-AD mice. Am J Pathol 173:1768-1782. [18] Garwood, C.J., Cooper, J.D., Hanger, D.P., Noble, W. (2010) Anti-inflammatory impact of minocycline in a mouse model of tauopathy. Front Psych – Neurodeg Dis 1(138):1-8. [19] Beauquis, J., Vinuesa, A., Pomilio, C., Pavía, P., Galván, V., Saravia, F. (2014). Neuronal and glial alterations, increased anxiety, and cognitive impairment before hippocampal amyloid deposition in PDAPP mice, model of Alzheimer's disease. Hippocampus. 24(3), 257-69. [20] Wright, A.L., Zinn, R., Hohensinn, B., Konen, L.M., Beynon, S.B., Tan, R.P., Clark, I.A., Abdipranoto, A., Vissel, B. (2013). Neuroinflammation and neuronal loss precede Aβ plaque deposition in the hAPP-J20 mouse model of Alzheimer's disease. PLoS One. 8(4), e59586. [21] Kitazawa, M., Cheng, D., Tsukamoto, M.R., Koike, M.A., Wes, P.D., Vasilevko, V., Cribbs, D.H., LaFerla, F.M. (2011). Blocking IL-1 signaling rescues cognition, attenuates tau pathology, and restores neuronal β-catenin pathway function in an Alzheimer's disease model. J Immunol. 187(12), 6539-49. [22] Simard, A.R., Soulet, D., Gowing, G., Julien, J.P., Rivest, S. (2006). Bone marrowderived microglia play a critical role in restricting senile plaque formation in Alzheimer's disease. Neuron. 49(4), 489-502. [23] Hickman, S.E., Allison, E.K., El Khoury, J. (2008). Microglial dysfunction and defective beta-amyloid clearance pathways in aging Alzheimer's disease mice. J Neurosci. 28(33), 8354-60. [24] Heneka, M.T., Kummer, M.P., Stutz, A., Delekate, A., Schwartz, S., Vieira-Saecker, A., Griep, A., Axt, D., Remus, A., Tzeng, T.C., Gelpi, E., Halle, A., Korte, M., Latz, E., Golenbock, D.T. (2013). NLRP3 is activated in Alzheimer's disease and contributes to pathology in APP/PS1 mice. Nature. 493(7434), 674-8. [25] Bhaskar, K., Konerth, M., Kokiko-Cochran, O.N., Cardona, A., Ransohoff, R.M., Lamb, B.T. (2010). Regulation of tau pathology by the microglial fractalkine receptor. Neuron. 68(1), 19-31. [26] Lent, R., Azevedo, F.A., Andrade-Moraes, C.H., Pinto, AV. (2012). How many neurons do you have? Some dogmas of quantitative neuroscience under revision. Eur J Neurosci. 35(1), 1-9. [27] Allen, N.J., Barres, BA. (2009). Neuroscience: Glia - more than just brain glue Nature. 457(7230), 675-7. [28] Ullian, E.M., Sapperstein, S.K., Christopherson, K.S., Barres, B.A. (2001). Control of synapse number by glia. Science. 291, 657-661. [29] Pannasch, U., Rouach, N. (2013). Emerging role for astroglial networks in information processing: from synapse to behavior. Trends Neurosci. 36(7), 405-17. [30] Sofroniew, M.V., Vinters, H.V. (2010). Astrocytes: biology and pathology. Acta Neuropathol. 119(1), 7-35. [31] Rodríguez, J.J., Yeh, C.Y., Terzieva, S., Olabarria, M., Kulijewicz-Nawrot, M., Verkhratsky, A. (2014). Complex and region-specific changes in astroglial markers in the aging brain. Neurobiol Aging. 35(1), 15-23. [32] Simpson, J.E., Ince, P.G., Lace, G., Forster, G., Shaw, P.J., Matthews, F., Savva, G., Brayne, C., Wharton, S.B.; MRC Cognitive Function and Ageing Neuropathology Study Group. (2010). Astrocyte phenotype in relation to Alzheimer-type pathology in the ageing brain. Neurobiol Aging. 31(4), 578-90. [33] Perez-Nievas, B.G., Stein, T.D., Tai, H.C., Dols-Icardo, O., Scotton, T.C., BarroetaEspar, I., Fernandez-Carballo, L., de Munain, E.L., Perez J, Marquie, M., Serrano-Pozo, A., Frosch, M.P., Lowe, V., Parisi, J.E., Petersen, R.C., Ikonomovic, M.D., Lopez, O.L., Klunk, W., Hyman, B.T., Gomez-Isla, T. (2013). Dissecting phenotypic traits linked to human resilience to Alzheimer's pathology. Brain. 136, 2510-2526. [34] Schwab, C., Klegeris, A., McGeer, P.L. (2010) Inflammation in transgenic mouse models of neurodegenerative disorders. Biochim Biophys Acta 1802, 889-902. [35] Furman, J.L., Sama, D.M., Gant, J.C., Beckett, T.L., Murphy, M.P., Bachstetter, A.D., Van Eldik, L.J., Norris, C.M. (2012). Targeting astrocytes ameliorates neurologic changes in a mouse model of Alzheimer's disease. J Neurosci. 32(46), 16129-40. [36] Noble, W., Garwood, C., Stephenson, J., Kinsey, A.M., Hanger, D.P., Anderton, B.H. (2009) Minocycline reduces the development of abnormal tau species in models of Alzheimer's disease. FASEB J 23, 739-750. [37] Pettus, B.J., Chalfant, C.E., Hannun, Y.A. (2002). Ceramide in apoptosis: an overview and current perspectives. Biochim Biophys Acta. 1585(2-3), 114-25. [38] Kraft, A.W., Hu, X., Yoon, H., Yan, P., Xiao, Q., Wang, Y., Gil, S.C., Brown, J., Wilhelmsson, U., Restivo, J.L., Cirrito, J.R., Holtzman, D.M., Kim, J., Pekny, M., Lee, J.M.. (2013). Attenuating astrocyte activation accelerates plaque pathogenesis in APP/PS1 mice. FASEB J. 27(1), 187-98. [39] Bellucci, A., Westwood, A.J., Ingram, E., Casamenti, F., Goedert, M., Spillantini, M.G. (2004). Induction of inflammatory mediators and microglial activation in mice transgenic for mutant human P301S tau protein. Am J Pathol. 165(5), 1643-52. [40] Blurton-Jones, M., Kitazawa, M., Martinez-Coria, H., Castello, N.A., Müller, F.J., Loring, J.F., Yamasaki, T.R., Poon, W.W., Green, K.N., LaFerla, F.M. (2009). Neural stem cells improve cognition via BDNF in a transgenic model of Alzheimer disease. Proc Natl Acad Sci U S A. 106(32):13594-9. [41] Di Bona, D., Plaia, A., Vasto, S., Cavallone, L., Lescai, F., Franceschi, C., Licastro, F., Colonna-Romano, G., Lio, D., Candore, G., Caruso, C. (2008). Association between the interleukin-1beta polymorphisms and Alzheimer's disease: a systematic review and metaanalysis. Brain Res Rev. 59(1),155-63. [42] Li, Y., Liu, L., Barger, S.W., Griffin, W.S. (2003). Interleukin-1 mediates pathological effects of microglia on tau phosphorylation and on synaptophysin synthesis in cortical neurons through a p38-MAPK pathway. J Neurosci. 23(5), 1605-11. [43] Ghosh, S., Wu, M.D., Shaftel, S.S., Kyrkanides, S., LaFerla, F.M., Olschowka, J.A., O'Banion, M.K. (2013). Sustained interleukin-1β overexpression exacerbates tau pathology despite reduced amyloid burden in an Alzheimer's mouse model. J Neurosci. 33(11), 505364. [44] Curran, B., O'Connor J.J. (2001). The pro-inflammatory cytokine interleukin-18 impairs long-term potentiation and NMDA receptor-mediated transmission in the rat hippocampus in vitro. Neuroscience 108(1), 83-90. [45] Amadoro, G., Ciotti, M.T., Costanzi, M., Cestari, V., Calissano, P., Canu, N. (2006). NMDA receptor mediates tau-induced neurotoxicity by calpain and ERK/MAPK activation. Proc Natl Acad Sci U S A. 103(8), 2892-7. [46] Yamada, K., Holth, J.K., Liao, F., Stewart, F.R., Mahan, T.E., Jiang, H., Cirrito, J. R., Patel, T. K., Hochgrafe, K., Mandelkow E. M., Holtzman, D. M. (2014). Neuronal activity regulates extracellular tau in vivo. J Exp Med. 211(3), 113-25. [47] Clavaguera, F., Grueninger, F., Tolnay, M. (2014). Intercellular transfer of tau aggregates and spreading of tau pathology: Implications for therapeutic strategies. Neuropharmacology. 76 Pt A:9-15. [48] Chung, W.S., Clarke, L.E., Wang, G.X., Stafford, B.K., Sher, A., Chakraborty, C., Joung, J., Foo, L.C., Thompson, A., Chen, C., Smith, S.J., Barres, B.A. (2013). Astrocytes mediate synapse elimination through MEGF10 and MERTK pathways. 504(7480), 394-400. [49] Ross, F.M., Allan, S.M., Rothwell, N.J., Verkhratsky, A. (2003). A dual role for interleukin-1 in LTP in mouse hippocampal slices. J Neuroimmunol. 144(1-2), 61-7. [50] Mandolesi, G., Musella, A., Gentile, A., Grasselli, G., Haji, N., Sepman, H., Fresegna, D., Bullitta, S., De Vito, F., Musumeci, G., Di Sanza, C., Strata, P., Centonze, D. (2013). Interleukin-1β alters glutamate transmission at purkinje cell synapses in a mouse model of multiple sclerosis. J Neurosci. 33(29), 12105-21.