14: Immunological products and vaccines
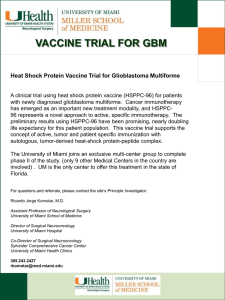
advertisement

14: Immunological products and vaccines Please select a topic: 14.4 Vaccines and antisera 14.5 Immunoglobulins Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 1 of 5 Date: 1.12.2012 14.4 Active immunity BCG Intradermal vaccine (BCG SSI®) Adsorbed Diptheria, tetanus and pertussis (acellular, component) and inactivated polio vaccine (InfanrixIPV) Adsorbed Diptheria (low dose), tetanus and pertussis (acellular, component) and inactivated polio vaccine (Repevax) Adsorbed Diptheria (low dose), tetanus and polio (inactivated) vaccine (Revaxis) Diptheria, tetanus and pertussis (acellular, component), poliomyelitis (inactivated) and Haemophilys tybe b conjugate vaccine (Pedicael) Haemophilus influenzae tybe b and meningitis group C vaccine (Menitorix) Hepatitis A vaccine – Occupational health only Hepatitis B vaccine (Engerix B, HBvaxPRO, Engerix B Paediatric) Influenza vaccine Measles, mumps and rubella vaccine (MMR Vax Pro, Priorix) Meningococcal group C vaccine (Meningitec, Menjugate) Pneumococcal vaccine (Prevenar, Pneumovax II, Prevenar 13) Varicella-zoster vaccine (Varivax) Diagnostic agents Tuberculin PPD 10 units/0.1ml injection Tuberculin PPD 2 units/0.1ml injection Prescribing Notes Vaccines for the childhood immunisation schedule should be obtained from local health organisations or from ImmForm (www.immform.dh.gov.uk)—not to be prescribed on FP10 (HS21 in Northern Ireland; GP10 in Scotland; WP10 in Wales). Preterm birth Babies born preterm should receive all routine immunisations based on their actual date of birth. The risk of apnoea following vaccination is increased in preterm babies, particularly in those born at or before 28 weeks postmenstrual age. If babies at risk of apnoea are in hospital at the time of their first immunisation, they should be monitored for 48 hours after immunisation. If a baby develops apnoea, bradycardia, or desaturation after the first immunisation, the second immunisation should also be given in hospital with similar monitoring. Seroconversion may be unreliable in babies born earlier than 28 weeks’ gestation or in babies treated with corticosteroids for chronic lung disease; consideration should be given to testing for antibodies against Haemophilus influenzae (type b), meningococcal C, and hepatitis B after primary immunisation. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 2 of 5 Date: 1.12.2012 Immunisation Schedule Neonates at risk only BCG Vaccine See section 14.4, BCG Vaccines Hepatitis B Vaccine See section 14.4, Hepatitis B Vaccine 2 months Diphtheria, Tetanus, Pertussis (Acellular, Component), Poliomyelitis (Inactivated), and Haemophilus Type b Conjugate Vaccine (Adsorbed) First dose Pneumococcal Polysaccharide Conjugate Vaccine (Adsorbed) First dose 3 months Diphtheria, Tetanus, Pertussis (Acellular, Component), Poliomyelitis (Inactivated), and Haemophilus Type b Conjugate Vaccine (Adsorbed) Second dose Meningococcal Group C Conjugate Vaccine First dose 4 months Diphtheria, Tetanus, Pertussis (Acellular, Component), Poliomyelitis (Inactivated), and Haemophilus Type b Conjugate Vaccine (Adsorbed) Third dose Meningococcal Group C Conjugate Vaccine Second dose Pneumococcal Polysaccharide Conjugate Vaccine (Adsorbed) Second dose 12–13 months Measles, Mumps and Rubella Vaccine, Live (MMR) First dose Pneumococcal Polysaccharide Conjugate Vaccine (Adsorbed) Single booster dose Haemophilus Type b Conjugate Vaccine and Meningococcal Group C Conjugate Vaccine Single booster dose Between 3 years and 4 months, and 5 years Adsorbed Diphtheria [low dose], Tetanus, Pertussis (Acellular, Component) and Poliomyelitis (Inactivated) Vaccine or Adsorbed Diphtheria, Tetanus, Pertussis (Acellular, Component) and Poliomyelitis (Inactivated) Vaccine Single booster dose Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 3 of 5 Date: 1.12.2012 Note: Preferably allow interval of at least 3 years after completing primary course Measles, Mumps and Rubella Vaccine, Live (MMR) Second dose 12–13 years (females only) 13–18 years Human Papilloma Virus Vaccine 3 doses; second dose 1–2 months, and third dose 6 months after first dose(1) Adsorbed Diphtheria [low dose], Tetanus, and Poliomyelitis (Inactivated) Vaccine Single booster dose During adult life, women of childbearing age susceptible to rubella Measles, Mumps and Rubella Vaccine, Live (MMR) Women of child-bearing age who have not received 2 doses of a rubellacontaining vaccine or who do not have a positive antibody test for rubella should be offered rubella immunisation (using the MMR vaccine)—exclude pregnancy before immunisation, but see also section 14.4, Measles, Mumps and Rubella Vaccine During adult life, if not previously immunised Adsorbed Diphtheria [low dose], Tetanus, and Poliomyelitis (Inactivated) Vaccine 3 doses at intervals of 1 month Booster dose at least 1 year after primary course and again 5–10 years later The two human papilloma virus vaccines are not interchangeable and one vaccine product should be used for the entire course. (1) Storage and use Vaccines should be protected from light. Unused vaccine in multidose vials without preservative (most live virus vaccines) should be discarded within 1 hour of first use; those containing a preservative (including oral poliomyelitis vaccine) should be discarded within 3 hours or at the end of a session. Particular attention must be paid to instructions on the use of diluents. Vaccines which are liquid suspensions or are reconstituted before use should be adequately mixed to ensure uniformity of the material to be injected. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 4 of 5 Date: 1.12.2012 14.5 Immunoglobulins Human normal immunoglobulin 5g injection (Vigam) Human normal immunoglobulin 750mg (16%) (Subgam – temporary alternative to human tetanus immunoglobulin. Human tetanus immunoglobulin 250 unit injection Anti-D immunoglobulin 500 unit injection (BPL) Anti-D immunoglobulin 300microgram/3ml syringe (Rhophylac) Varicella Zoster immunoglobulin Dose Consult product literature Prescribing notes Supplies of Human Norman Immunoglobulin (Vigam) are strictky controlled throughout the UK and use is limited to specific approved indications. Please contact pharmacy on ext 2316 prior to prescribing & order using prescription form for immunoglobulin which can be found at http://www.departments/medicines/prescriptions.html Varicella Zoster immunoglobulin should be requested from HPA via On-call Microbiologist. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 5 of 5 Date: 1.12.2012