BAAS Application
advertisement
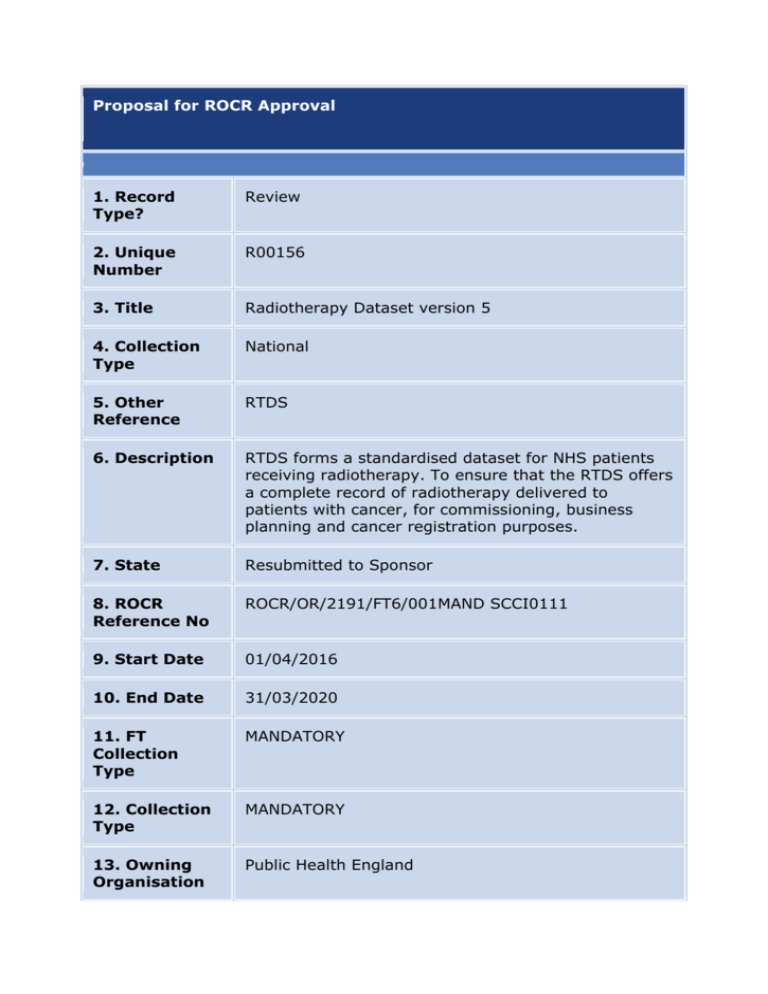
Proposal for ROCR Approval 1. Record Type? Review 2. Unique Number R00156 3. Title Radiotherapy Dataset version 5 4. Collection Type National 5. Other Reference RTDS 6. Description RTDS forms a standardised dataset for NHS patients receiving radiotherapy. To ensure that the RTDS offers a complete record of radiotherapy delivered to patients with cancer, for commissioning, business planning and cancer registration purposes. 7. State Resubmitted to Sponsor 8. ROCR Reference No ROCR/OR/2191/FT6/001MAND SCCI0111 9. Start Date 01/04/2016 10. End Date 31/03/2020 11. FT Collection Type MANDATORY 12. Collection Type MANDATORY 13. Owning Organisation Public Health England Proposal for ROCR Approval 14. Owning Department National Disease Registration 15. Owner Name and Contact Details Name: Stephen Raynor Email: Stephen.raynor@phe.gov.uk Tel No: 0203 682 0716 Location: Skipton House 80 London Road, Elephant & Castle, London, SE1 6LH 16. Senior Supporting Official Name Dr Jem Rashbass 17. Senior Supporting Official Contact Details Title: Dr Jem Rashbass, Director National Disease Registration Tel No: 07796 315426 Email: jem.rashbass@phe.gov.uk Location: PHE HQ, Wellington House, 133-155 Waterloo Road, London, SE1 8UG 18. Data Provider Burden Days 2900 18. Data Provider Burden £ £ 900184.6 18. Frequency Monthly 18. Source Organisations (Number of Acute Foundation Trust (50) Proposal for ROCR Approval orgs) 19. Set Up Costs £ 248321 20. Other Costs £ 160767.5 21. Total Costs £ 1309273.1 22. Please explain the reason for any increase or decrease in burden and provide details of the any other costs figure provided in Q20 This application is to change the destination of where data are transmitted to. The data extraction and submission costs for organisations remain at the same level there is no increase in costs. Set up Costs relate to the costs PHE incurs in establishing the infrastructure and resources for the service. Other costs express the recurrent costs of PHE in collecting analysing and reporting on RTDS. Additionally from a provider point of view PHE will not charge £1000 per organisation to access a reporting microsite (see 24 below). 23. Benefits to Patients and the NHS The original programme for the collection of radiotherapy data was commissioned by the National Cancer Intelligence Network (NCIN), now part of Public Health England (PHE). The transition to PHE has brought together the National Cancer Registration Service which already manages the Cancer Outcomes and Services Dataset and the national Systemic Anti Cancer Therapy Dataset under the Disease Registration Division, within the Chief Knowledge Officer's Directorate in PHE. Additionally, all former cancer analytical resources from the old cancer registries have been brought under the Chief Knowledge Officer's ambit within the Knowledge and Intelligence Teams. It follows that, along with the Systemic Anti-Cancer Therapy dataset (SACT), the RTDS should be brought into the National Cancer Proposal for ROCR Approval Registration Service within the Disease Registration Division, as an additional data repository in order to centralise data collection for cancer therapies and provide the programme with the extensive support available within PHE. It is a logical step which will see the programme benefit from centralised data quality and data capture systems across 160 providers of cancer care, reducing the number of resources required to deliver data across the NCRS yet increasing the yield in the data collected and the efficiency in its management. The benefits of the collection will allow outcomes analysis on all of the diagnostic and treatment events in a patient's cancer pathway which will inform service planning, delivery and commisioning for outcomes. 24. Financial benefits to running this collection NatCanSat the current organisation collecting the data charges £1000 per RT site to access their reporting microsite. PHE would provide an equivalent service free of charge thereby saving organisations, collectively up to £50,000 per annum. There is an overall reduction in the costs to PHE of bringing the service in-house of around £142k over 5 years. (see 22 above) 25. Publication methods Web site & PHE publications gateway 26. Publication Links www.gov.uk/phe 27. Requesting Organisation Public Health England 28. Collection Method Extract from existing NHS systems Proposal for ROCR Approval 29. NHS Mandate Commitment Improving Outcomes: A Strategy for Cancer and A Framework for Cancer Intelligence Gateway Reference 16920 30. Changes since last assessment The organisation collecting and managing the data has changed from NatCanSat to Public Health England. 31. Data in operational systems Yes 32. Plans for collecting this data from operational systems 33. If the data was not collected, what would the consequences be It would be impossible to identify the cost and effectiveness of the use of radiotherapy in England. NHS England would not be able to monitor QIPP relating to Breast and Bone metastases and other service specifications of national commissioning. The cancer registry's statutory obligations and cancer outcomes analysis would be at risk. 34. Is there an impact assessment or business case for this collection? If so please attach Yes 35. Process required for others to go through to Data will be made available for legitimate service providers and commisisoners freely in addition to standard reports. However, all requests for explicitly identifiable and potentially identifiable data held by Proposal for ROCR Approval obtain the data PHE need to be made in writing to the Office for Data Release by email to ODR@phe.gov.uk Requests may be made by the applicant directly or via a receiving office. Data requests should be accompanied by a completed ODR form and supporting documents (such as study protocol, data specification and data management procedures) which outline the rationale for the data request, specific data fields, and expected timescales. PHE will only provide access to identifiable or potentially identifiable data where there is an acceptable legal gateway, for example Section 251. The ODR meets weekly to decide the outcome of data requests. Where possible, the applicant will be informed of one of three outcomes within 2 weeks of receiving the initial request. 36. Keywords Radiotherapy, Cancer, Linear Accelerator 37. National / Official statistic National 38. Method used to store the data Original data submission files will generally be stored on NCRS file servers, with file encryption passwords in a secure keystore to which only authorised NCRS administrators have access. Where NCRS provides a file submission service, the uploaded files will be encrypted with public/private key encryption, before they are retrieved and moved to the NCRS file servers. The files are eventually processed and loaded into database tables, as part of the NCRS database. Original data submission files will generally be stored on NCRS file servers, with file encryption passwords in a secure keystore to which only authorised NCRS administrators have access. Where NCRS provides a file submission service, the uploaded files will be encrypted with public/private key encryption, before they are retrieved and moved to the NCRS file servers. The files are eventually processed and loaded into database tables, as part of the NCRS database. Proposal for ROCR Approval 39. Why sampling is not used The purpose of the standard is to have a complete record of all radiotherapy undertaken in England. This is essential for the purposes of commissioning and cancer registration. 40. Details of any pilots PHE is working with pilot Radiotherapy providers to understand the technical demands of obtaining and redirecting the data extracts to PHE. The sites being consulted are: Guy's and St Thomas' NHS Trust Imperial College Hospital NHS Trust The Norfolk and Norwich NHS Trust Leeds Teaching Hospitals NHS Trust Many more sites will be contacted and worked with during 2015/16 41. Equalities dimensions used in the collection Age/Date of Birth, Gender, Ethnicity (NHS standard 16 + 1) 42. Policy that the collection supports The detail of the national radiotherapy programme and in support of understanding radiotherapy can be found at http://www.ncat.nhs.uk/our-work/ensuring-bettertreatment/radiotherapy Improving Outcomes: A Strategy for Cancer (2011) sets out that "Access to radiotherapy is critical to improving outcomes and, to improve outcomes from radiotherapy, there must be equitable access to high quality, safe, timely, protocoldriven quality-controlled services focused around patients’ needs”. Detailed modelling suggests that 52% of cancer patients should receive radiotherapy as part of their treatment. In 2007, it was estimated than only 37% of cancer patients accessed this treatment. While radiotherapy capacity has increased, the demand has not increased at the rate previously predicted and there remain variations in activity across the country. 43. IG Data type Patient identifiable